Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.9 n.4 Centurion Jan. 2010
CASE REPORT AND REVIEW OF THE LITERATURE
Traumatic hip dislocation in children: the role of MRI
F SprongI ; C SnyckersII
IMBChB(Pret), Registrar (Ortho)
IIMBChB(Pret), FCS(SA)Ortho, MMed(Orth Surg)UP, Consultant, Steve Biko Academic Hospital, University of Pretoria
ABSTRACT
We report a case of traumatic left hip dislocation in a nine-year-old child following the article: Firth GB, Mazibuko AD, Munir M. Traumatic dislocation of the hip joint in children. SAOJ Autumn 2010; 9(1):68-71. This article, as do others, refers to the use of MRI and CT scan in investigating young patients with hip dislocations. These authors conclude that a CT scan or MRI is probably always indicated.1 In this case report and literature review, we focus on the role of special investigations and the indication to perform either a CT scan or MRI in this young age group. The routine use of MRI and CT scan following hip dislocations in children is probably unnecessary and should only be done when indicated. This includes incongruent joint reduction noted on postreduction plain films and instability after reduction. There is not enough evidence to perform further investigations routinely without indication as they are costly, CT scans expose the child to radiation and MRI may involve anaesthesia or sedation of the child. If indicated, especially in the young child, an MRI scan provides more information and is the investigation of choice.
Case report
A nine-year old boy was referred to our hospital following an injury to his left hip after being tripped playing soccer at school. He was initially seen and assessed at a district hospital where he received analgesia and the referral to our hospital was arranged. He arrived at our institution 2 hours and thirty minutes after his injury.
On arrival, physical examination revealed the affected leg to be internally rotated, flexed, shortened and adducted. Both lower limb pulses were palpable and equal. There was no motor or sensory deficit on neurological examination. Plain radiographs confirmed the clinical diagnosis of a posterior hip dislocation without any visible fractures or bony fragments visible on these films (Figure 2).


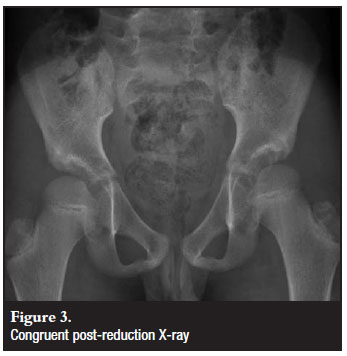
The child was given Dormicum and pethidine intravenously in the casualty department and the dislocation was reduced using a technique described by Nordt2 (Figure 1). Post reduction the hip was stable. Plain films confirmed a congruent reduction. Although the post-reduction X-rays were congruent (Figure 3) and the hip stable, we decided to perform a CT and MRI scan to determine the presence of any acetabular fragments or femoral head fractures and to exclude any soft tissue interposition or labral tears.
CT scan confirmed a congruent reduction of the joint with a small avulsion fragment from the superior aspect of the fovea attached to the round ligament, not causing any interposition (Figure 4). No fractures were noted in the acetabulum.

MRI noted the round ligament avulsion with infero-medial displacement of this structure, but not causing any joint space widening (Figure 5). Cartilage damage on the superior area adjacent to the fovea was also reported with surrounding bone oedema. No labral tears or soft tissue interposition was noted. High signal intensity along the muscular and fascial planes pointed out diffuse surrounding soft tissue oedema.

The child was admitted to the ward and skin traction was applied with strict bed rest, non-weight bearing for three weeks. He was discharged after three weeks partial weight bearing to follow up six weeks post injury.
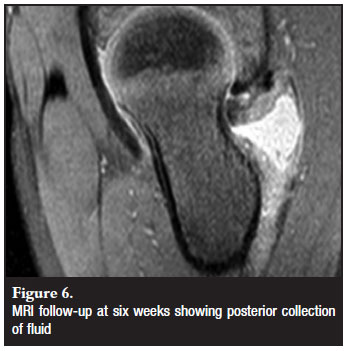
MRI was repeated six weeks later to detect any early signs of avascular necrosis and to correlate these findings with the initial MRI scan done after admission (Figure 6). The surrounding soft tissue oedema was markedly reduced with a small residual effusion present in the hip joint. Thinning of the cartilage in the femoral head around the fovea correlated with the previously mentioned cartilage damage. The avulsed fragment remained undisplaced. The femoral head appeared normal with no evidence of avascular necrosis (Figure 7). A small fluid collection was noted posterior to the femoral neck. Clinically the child had no limp and was mobilising pain free without any walking aid.

Review of the literature
Pathophysiology
Traumatic hip dislocations in children are very rare (5% of all hip dislocations occur in patients younger than 14 years of age).3,4,5 There is a correlation between the age of the patient and the force required to dislocate the hip. Dislocations of the hip may occur as a result of low-energy injuries sustained during minor trauma while participating in sporting activities, usually in younger children (<10 years).6 High energy trauma or an increase in force, such as seen in motor vehicle accidents, cause hip dislocations in older children (>10 years).6-9 The absence of femoral or acetabular bony lesions (83% of cases) may be due to the flexibility of the periarticular structures.6,7,9 Isolated posterior dislocations occur in the majority of cases.3,4,6,8-11
Males are more commonly affected than females and it seems that the left hip is more involved than the right.3,10,11 Dislocations in children are scarce and therefore clinical trials stretch over long periods and are often multi-centred. Most of the larger series reported on were published at least 20 years ago. With the newer advantage of CT and MRI scans to evaluate these patients, the prevalence of soft tissue and cartilage damage may be picked up more accurately if investigated well.12 Due to the high cost, radiation exposure and the technical difficulty of doing these examinations in children, the indications for further imaging must be well motivated.
Clinical presentation
A complete and thorough history must include the mechanism of injury. Additional trauma may distract the examiner into either missing a dislocated hip or only focusing on the dislocation and missing associated injuries. Injuries that may occur with a hip dislocation in a child include fractures of the acetabulum, femoral head, or greater trochanter as well as growth plate injuries to either the femoral head or acetabulum, and femoral shaft fractures.3,6,7 Posterior dislocations present with the hip in flexion, adduction and internal rotation. Anterior dislocations (extremely rare) present with the hip in extension, abduction and external rotation.
Vascular and neurological examination with detailed documentation is a medico-legal necessity.
Special investigations
An early reduction is an absolute priority and is the only factor that may decrease the risk of avascular necrosis.4,6-8,13 Good quality radiographs are usually sufficient to confirm the diagnosis of a hip dislocation and a congruent reduction. If there is any doubt about concentric reduction, further imaging of the affected joint is indicated.9 The early diagnosis of incomplete reduction may prevent the devastating complications following incongruent joints post reduction.4 In their series of 35 cases, reported by Vialle et al,9 CT scan was only performed in cases where the post-reduction joint space remained incongruent. In fact, any suspicion of joint incongruency and post-reduction instability is an indication for further examination and possible open reduction.6,12,13 This includes a break in Shenton's line, if the femoral head is not concentric in the acetabulum or if the joint space is increased14 in comparison to the normal side.
Rubel et al reported on two cases where X-rays and CT scans could not determine the amount of posterior wall involvement after posterior hip fracture dislocation in children. In both cases the post-reduction clinical examination revealed instability, necessitating the need for an MRI scan.12 Posterior wall involvement occurs in 17%-33% of children with a posterior hip dislocation.12 Due to immature bone in children, CT scans may be ineffective in determining the true size of posterior wall fragments in unstable hips after reduction. The author concluded that MRI scan was both very sensitive and accurate in determining the actual size of the fragment which was confirmed intra-operatively.12
Chun et al reported on a surgically confirmed case of acetabulum labrum entrapment diagnosed pre-operatively by MRI.4 MRI proved to be superior to CT in delineating more soft tissue pathology, whereas CT could only demonstrate calcified intra-articular bony fragments. The author concluded that MRI is the technique of choice in a non-concentric hip post reduction, where soft tissue interpositioning is suspected.4
Although MRI scan was more sensitive in detecting bony ischaemia and soft tissue interposition, it was not a predictor of epiphyseal necrosis.9
Treatment
Most cases of hip dislocation in children can be treated non-surgically with immediate closed reduction, preferably within six hours of injury.3,4,6,11,13,15 Reduction should ideally be performed in theatre under general anaesthesia to obtain complete muscle relaxation.3,7,8 Care must be taken not to cause any further damage to growth plates. Post-reduction X-rays will determine the need for further investigations (see special investigations).
No consensus regarding the post-reduction nonweight bearing period exists and it seems that the time spent in traction does not alter the final outcome.3,7,8,10 A congruent, stable hip post reduction can be treated with three weeks of skin traction in bed, followed by partial weight bearing for another three weeks.3,13 The patient should be followed up for at least two years to detect any early complications such as avascular necrosis of the femoral head.13 We advise an MRI examination before the patient takes part in contact sports.
In the event of instability and/or incongruent reduction, an open reduction should be performed, following CT or MRI to determine the cause. Open reduction is required in fewer than 7% of cases4 where entrapment of capsular and/or osteochondral fragments may prevent congruent reduction. In the majority of cases the surgical approach depends on the direction of the dislocation with a posterior approach being favoured for a posterior dislocation and vice versa.3,6 The incidence of soft tissue interposition, after closed reduction, ranges between 15% and 25%.9,11
Complications
• Avascular necrosis of the femoral head is the most feared complication. The incidence following hip dislocation ranges from 0% to 15%. Provided early reduction is performed and no femoral head fractures or growth plate injuries co-exist, this percentage can be very low.1,3,6,9,10
• Neurological compromise involving the sciatic nerve may occur in 5% to 20% of cases.3,6,13 Exploration of the nerve is seldom necessary unless open reduction is required for other reasons.6 Return of function can be expected in most cases.
• Vascular injuries are extremely rare, but potentially devastating. The femoral vessels may be injured or compressed during an anterior dislocation of the hip. Immediate reduction can lead to restoration of this problem but practitioners must be aware of this complication.13
• Osteoarthritis in children following hip dislocations is rare and the incidence can be decreased by early reduction and achieving joint congruency. The amount of trauma involved also determines the prognosis. Arthritic changes in the joint usually develop secondary to avascular necrosis.3,10
• Coxa magna is a common occurrence in children following hip dislocations. Reactive hyperaemia and associated soft tissue damage may be the cause of femoral head overgrowth seen in 13% to 47% of cases.7,11 This condition is usually asymptomatic and does not predict the final outcome.
• Other complications include recurrent dislocations, irreducible dislocations, heterotopic bone formation and premature closure of the triradiate cartilage.
Conclusion
MRI scan is both more sensitive and specific in determining the actual size of the fragment which may be very important in surgical decision-making.12 MRI also provides useful information of the surrounding soft tissues as a possible cause for instability or recurrent dislocations.4 Soft tissue interposition is a common finding.1 However, MRI is technically more difficult and expensive and may necessitate a general anaesthetic in younger children.
As noted in our case report, the routine use of MRI and CT scan following hip dislocations in children is unnecessary and should only be done when indicated. This includes incongruent reduction noted on post-reduction plain films and instability after reduction.
Key points to note
• Hip dislocations in children can occur as a result of minimal trauma, especially in younger children.
• Look for associated injuries including head, chest and abdominal trauma.
• Immediate reduction (within six hours) reduces the risk of complications.
• Any sign or suspicion of post-reduction incongruency or instability necessitates the need for further investigations.
• A congruent post-reduction X-ray with a clinically tested stable hip does not need further investigations.
• CT scan may be ineffective in determining the true size of bony fragments or posterior wall fractures in young children due to the nature of immature bone.
• MRI scan is more sensitive and accurate in determining actual fracture size in children and provides additional information regarding the soft tissues adjacent to, or within the joint.
References
1. Firth GB, Mazibuko AD, Munir M. Traumatic dislocation of the hip joint in children. SAOJ 2010;9(1):68-71. [ Links ]
2. Nordt WE,3rd. Maneuvers for reducing dislocated hips. A new technique and a literature review. Clin Orthop 1999 Mar(360):260-64. [ Links ]
3. Salisbury RD, Eastwood DM. Traumatic dislocation of the hip in children. Clin Orthop. 2000 Aug;377:106-11. [ Links ]
4. Chun KA, Morcuende J, El-Khoury GY. Entrapment of the acetabular labrum following reduction of traumatic hip dislocation in a child. Skeletal Radiol 2004 Dec;33(12):728-31. [ Links ]
5. Hamilton PR, Broughton, NS. Traumatic hip dislocation in childhood. Journal of Pediatric Orthopaedics 1998 September/October;18(5):691-94. [ Links ]
6. Herrera-Soto JA, Price CT. Traumatic hip dislocations in children and adolescents: pitfalls and complications. J Am Acad Orthop Surg 2009 Jan;17(1):15-21. [ Links ]
7. Kutty S, Thornes B, Curtin WA, Gilmore MF. Traumatic posterior dislocation of hip in children. Pediatr Emerg Care 2001 Feb;17(1):32-35. [ Links ]
8. Forde JC, Khan KS, Awan N. Traumatic posterior dislocation of the hip in a 3-yearold child. Pediatr Emerg Care 2009 Sep;25(9):584-85. [ Links ]
9. Vialle R, Odent T, Pannier S, Pauthier F, Laumonier F, Glorion C. Traumatic hip dislocation in childhood. J Pediatr Orthop 2005 Mar-Apr;25(2):138-44. [ Links ]
10. Schlonsky J, Miller PR. Traumatic hip dislocations in children. J Bone Joint Surg Am 1973 Jul;55(5):1057-63. [ Links ]
11. Offierski CM. Traumatic dislocation of the hip in children. J Bone Joint Surg Br 1981 Aug;63-B(2):194-97. [ Links ]
12. Rubel IF, Kloen P, Potter HG, Helfet DL. MRI assessment of the posterior acetabular wall fracture in traumatic dislocation of the hip in children. Pediatr Radiol 2002 Jun;32(6):435-39. [ Links ]
13. Engelbrecht PR, Gräbe RP. Traumatic dislocation of the hip in children. A report of 4 cases. S Afr J Surg. 1992 Dec;30(4):175-77. [ Links ]
14. Canale ST, Manugian AH. Irreducible traumatic dislocations of the hip. J Bone Joint Surg Am1979 Jan;61(1):7-14. [ Links ]
15. Quick TJ, Eastwood DM. Pediatric fractures and dislocations of the hip and pelvis. Clin Orthop 2005 Mar(432):87-96. [ Links ]
 Reprint requests:
Reprint requests:
Dr F Sprong
fsprong@telkomsa.net
The content of this article is the sole work of the authors. No benefits of any form have been received from a commercial party














