Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SA Orthopaedic Journal
versión On-line ISSN 2309-8309
versión impresa ISSN 1681-150X
SA orthop. j. vol.9 no.4 Centurion ene. 2010
CLINICAL ARTICLE
Misdiagnosis of hip pain could lead to unnecessary spinal surgery
Dr Allan A van Zyl
MBChB(Pret), MMed(Orth), FCS(Orth)SA, Medi-Clinic Hospital, Bloemfontein, South Africa
ABSTRACT
Osteoarthritis of the hip occurs in 10-30% of adults and is especially common in the elderly. Twenty-one per cent of people over the age of 65% are also shown to have degenerative spinal stenosis. It thus follows that patients with osteoarthritis of the hip could have a concomitant degree of spinal stenosis.1,2
Introduction
The symptoms of hip pain and spinal stenosis leg pain can be very similar with only subtle differences in both history and clinical examinations. To further compound the clinical problem the symptoms of spinal stenosis can be aggravated by pre-existing hip arthritis as well as knee arthritis (the so-called hip-spine syndrome and knee-spine syndrome).3,4 This is due to a degree of hip flexion contracture which forces the lumbar spine into increased lumbar lordosis when standing or walking. Spinal stenosis is classically diagnosed in patients with leg pain that occurs during standing or walking and is relieved when the individual sits down (neurological claudication). It is a clinical diagnosis, which is only confirmed by radiological investigations, usually magnetic resonance imaging (MRI). Research shows that in as many as 50% of elderly patients, MRI could give a false positive diagnosis of spinal stenosis. It is thus clear that if the clinical diagnosis is incorrect, it is quite possible to find enough evidence on MRI to prompt the surgeon into performing spinal surgery in this group of elderly patients.
Other pathology apart from degenerative hip and knee joints could refer pain to the thigh, including: lumbar facet arthritis, pelvic fractures and gynaecological disorders to name just a few.
If indications for spinal surgery in patients with existing hip pathology include pain in the area of the hip joint, the result may be that symptoms persist and can often give rise to further surgery on the spine (if the hip pathology remains undetected). This wrong-site surgery is not only unfortunate but also detrimental to the patients and results in frequent malpractice lawsuits, many of which are currently being investigated by the Health Professions Council of South Africa.5,6
This was evident to me when a couple of patients were seen in quick succession where spinal surgery did not relieve their leg pain resulting in a lot of discontent, as it was found that not only was their initial pain not relieved, but it was now of a higher intensity than before the procedures. After examination of the hip it was revealed that arthritis in this joint was the primary cause of pain. Following hip replacement surgery, all cases resulted in complete relief of pain. It was then decided to analyse, retrospectively, the primary total hip replacements that were performed at Medi-Clinic Hospital in Bloemfontein to look for concomitant spinal surgery.
Method
A retrospective analysis was performed on patients who had total hip replacement (THR) surgery in my private practice with specific reference to previous as well as subsequent spinal surgery following their THR.
Results
Over a period of 8 years (1992-2000) 949 primary total hip replacements were performed in 814 patients. Sixty-six (8.11%) of these patients had spinal surgery. Sixty-one patients had spinal surgery before their hip surgery and only five after their hip surgery. Of the 61 patients who underwent spinal surgery prior to their THR, 15 patients (24%) stated that their leg pain was not relieved postoperatively. This pain was resolved following their THR procedure. It follows that these 15 patients possibly underwent wrongsite surgery. Correct diagnosis of these patients also took a long time. Many patients were subject to numerous MRI scans, had multiple epidural injections and were unfortunately subjected to repeat back surgery as they continued to complain of their leg pain, the source of which was hip pathology.
Some examples of the 15 patients follow.
Case 1
• 61-year-old female
• (L) thigh pain radiating below the knee
• Underwent a L5/S1 fusion and laminectomy
• Nine months later she had a repeat fusion
• Wound sepsis developed and resulted in removal of hardware
• She subsequently endured repeated pain blocks and epidurals
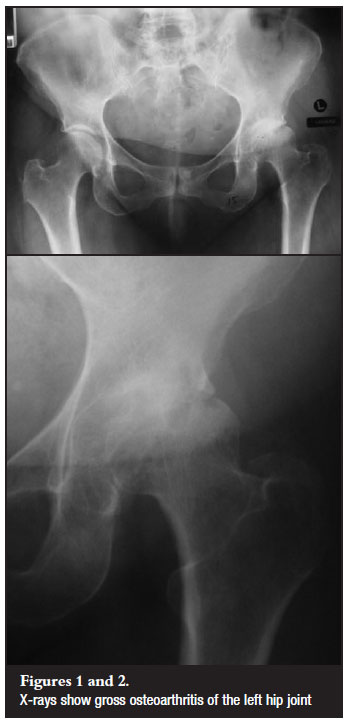
• Eleven months after her second back operation she was seen with gross osteoarthritis of the (L) hip and a THR was performed with alleviation of her pain (Figures 1, 2 and 3).

Case 2
• 76-year-old male
• Underwent two laminectomies the last of which was done 2 months previously
• Patient developed a pulmonary embolism postoperatively
• Once again gross osteoarthritis of the hip was seen with partial collapse of the head was seen and a THR performed (Figures 4 and 5).

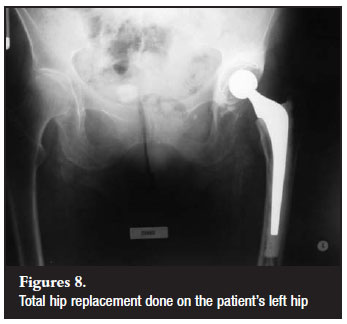
Case 3
• 85-year-old female
• Pain (L) thigh radiating to the ankle
• Underwent a laminectomy seven months previously
• Her (L) leg was 2.5 cm shorter
• X-rays show progressive osteoarthritis of the (L) hip with head and acetabular erosion and a THR was performed (Figures 6, 7 and 8).

Discussion
The incorrect diagnosis of spinal stenosis in patients with primary hip arthritis can lead to devastating consequences, especially if this leads to inappropriate spinal surgery, repeated spinal surgery and costly investigations.
During normal gait, the pelvis rotates by up to 40 degrees with two degrees of rotation at each lumbar level. In addition to this, there is a 5 cm oscillation and a 2.5 cm medial and lateral movement.7 No record of gait analysis and the effect on the lumbar spine in the arthritic hip could be found in the literature. It can however be assumed that, with these abnormal gait patterns, an increased strain at each lumbar level exists. Furthermore a flexion contracture of the hip will further increase lumbar lordosis and shift the lordosis more proximally which will increase spinal stenosis symptoms in borderline cases.8
It also follows that normalisation of gait and relief of hip flexion contractures following a THR may result in less stress on the lumbar spine. The converse may also be true where spinal stenosis symptoms may come to the fore once patients are more mobile. This however is a rare occurrence in my experience.
If a patient presents with both hip and spine pathology and surgery is indicated, it is my opinion that the THR should be performed initially in an attempt to correct abnormal biomechanics. This is further motivated by the fact that hip joint arthroplasty has a better and more predictable outcome than spinal surgery.2
To minimise the occurrence of this, I would like to emphasise the following in addition to an appropriate clinical history and examination:
1. Ask the patient if he can reach his toes easily (for washing or nail clipping). If there is a difference between the two legs, this can be an early sign of the onset of hip stiffness in association with hip arthritis.
2. Be wary when seeing patients who have been admitted to hospital for leg pain. It can sometimes be difficult to get patients out of bed and walking due to various social and time-consuming factors (this can also occur in a busy practice where patients are taken to the examination couch where walking is not observed by the examiner). It is quite easy to miss the typical Trendelenburg gait of hip arthritis sufferers as well as the typical 'hand under the thigh' help for the arthritic hip when getting on or off the examination couch.
3. Always make a point of examining the joint above and below the suspected area of pathology. This includes examining the hip joint in cases of back problems.
4. Ask your radiology department to routinely include an anterior-posterior X-ray of the pelvis when asking for X-rays of the lumbar spine.
5. Always examine your patient before looking at the MRI. Imaging should be used to confirm clinical diagnosis of spinal stenosis and should not be used for pure diagnostic purposes. Cases have been reported where patients have been booked for surgery based on MRI results alone. This is not a recommended approach.
6. Avoid a tunnel vision approach in your field of expertise. Pathology in the hip and spine can co-exist. Correct diagnosis is important and the patient needs to be treated as a whole.
Conclusion
Hip arthritis and spinal stenosis occur commonly in elderly patients. It is essential that one recognises this problem when patients are primarily referred for hip or spinal complaints. Hip arthritis is usually an uncomplicated diagnosis that should not be overlooked as this could result in costly and potentially hazardous diagnostic and operative spinal interventions.
References
1. Swezey, RL. Over diagnosed sciatica and stenosis, under diagnosed hip arthritis. Orthopaedics, Feb 2003;26(2):173-74. [ Links ]
2. McNamara MJ, Barret KG, Christie MJ, Spengler DM. Lumbar spinal stenosis and lower extremity arthroplasty. Journal of Arthroplasty, June 1993;8(3):273-77. [ Links ]
3. Offisski CM, Macnab I. Hip-spine syndrome. Spine 1983;8:316-21. [ Links ]
4. Murate Y, Takahashi K, Yamagota M, et al. The knee-spine syndrome. Journal of Bone and Joint Surgery (Br). Jan 2003;85B.1:95-99. [ Links ]
5. Gräbe R. Editorial: Wrong site surgery. SA Orthopaedic Journal, Aug 2004;3/3:8-14. [ Links ]
6. Du Toit G. Wrong level spinal surgery. SA Orthopaedic Journal Aug 2004;3/3:16-22. [ Links ]
7. Hoppenfeld, Stanley. Physical examination of the spine and extremities. 1976 Appleton-Century-Crofts. [ Links ]
8. Jackson RP, Peterson MD, McManus AC, Hales C. Compensatory spinopelvic balance over the hip axis and better reliability in measuring lordosis to the pelvic radius on standing lateral radiographs of adult volunteers and patients. Spine 1998;23:16, 1750-67. [ Links ]
 Reprint requests:
Reprint requests:
Dr Allan A van Zyl
PO Box 28772
Danhof 9310
Tel: 051 448-3051/ Fax: 051 488-3020
email: Dr.allanvanzyl@bfn.co.za














