Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.9 n.3 Centurion Jan. 2010
CASE REPORT AND REVIEW OF THE LITERATURE
Avulsion fracture of the calcaneal tuberosity
M RadzilaniI; EJ D'AltonII; R GoleleIII
IMBChB. Registrar, Department of Orthopaedics, Dr George Mukhari Hospital, Pretoria
IIMBChB(Pret), MMed(Orth). Consultant, Dr George Mukhari Hospital, Pretoria
IIIMBChB(Natal), MFGP(SA), MMed(Orth), FCSOrth(SA). Professor and Head of Department Orthopaedics Surgery, University of Limpopo (Medunsa campus)
Introduction
Avulsion fractures of the calcaneal tuberosity are uncommon injuries. Calcaneal fractures account for 1.5% of all fractures. Avulsion fractures of the calcaneal tuberosity comprise only 1.5% to 3% of calcaneal fractures. The peak incidence is in females in their seventh decade as a consequence of diminished bone mineral density.1-4
We present a male patient who presented with an avulsion fracture of the calcaneal tuberosity.
The purpose of this report is to emphasise the comparative rarity of avulsion fractures of the os calcis, the importance of early diagnosis, and the necessity for instituting treatment in order to avoid subsequent complications.
Case report
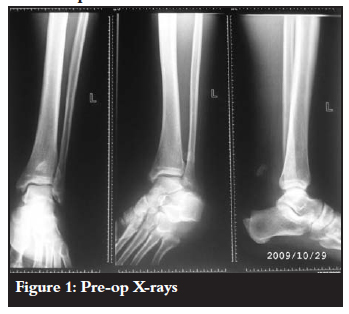
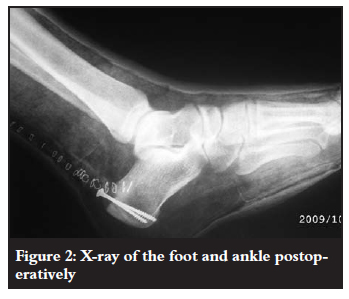
The fracture shown in Figure 1 occurred in a 50-year-old male electrician. He was treated in a Plaster of Paris cast at the peripheral hospital and was referred to us a week after injury. He gave a history that he missed a step and fell while on duty, landing with the left ankle in maximum dorsiflexion. The left foot started swelling and he was unable to bear weight or plantarflex. He has been smoking ten cigarettes a day for the past 30 years. He has also been drinking about 800 ml of beer a week for the past 30 years. Examination showed a swollen and tender left foot, with a palpable bony hard mass about 10 cm proximal to tendon Achilles insertion. He walked with an antalgic gait with the foot kept plantigrade to slight dorsiflexion. Thompson's test was positive. A diagnosis of a ruptured tendon Achilles was made. X-rays revealed a bony avulsion of the posterior tuberosity of the calcaneus lying about 10 cm proximal to its insertion (Figure 1). The patient was taken to theatre for surgery two days later. Intraoperatively it was found that the upper one-third of the calcaneal tuberosity was avulsed with the bony fragment lying more than 10 cm high from its insertion. The bony fragment was reduced and fixed with compression screws (Figure 2). The patient received 2 g intravenous cloxacillin intra-operatively and 1 g 12 hours postoperatively.
Postoperatively the patient was treated with a gravitydependent below-knee cast and elevation until the swelling subsided. After three days the patient was discharged in a below-knee cast for further elevation at home. At two weeks during follow-up it was found that the patient had developed superficial sepsis along the incision site (Figure 3). A pus swab cultured Staphylococcus aureus which was sensitive to cloxacillin.

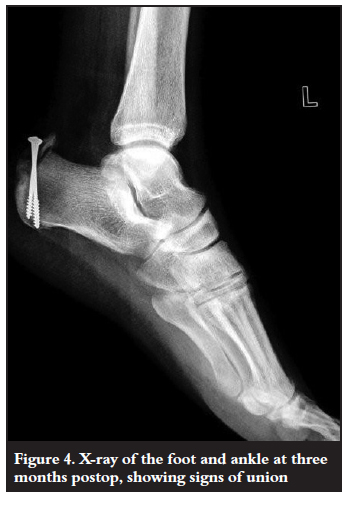
The sepsis was treated for two weeks with dressings and oral antibiotics until the wound was healed. During this time the ankle was immobilised with an ankle orthosis with a limiting up-stop. A below-knee cast was then applied in plantarflexion for four weeks. Subsequently, a below-knee cast was applied with the ankle in plantigrade position. This was kept for an additional four weeks. After 10 weeks he was allowed to fully weight bear and was referred to physiotherapy for rehabilitation with an emphasis on heel cord stretching. X-rays taken at 10 weeks showed early signs of union (Figure 4). At six months the fracture was united (Figure 5).
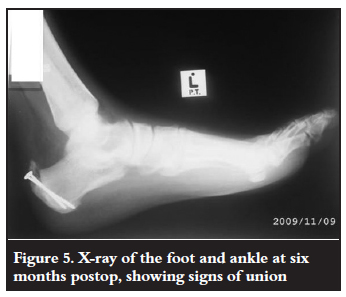
The patient returned to work 12 weeks after the injury. He was able to run, climb stairs and to stand on his toes as shown in Figure 6. The patient had no residual disability.

Discussion
Malgaigne described avulsion fractures of the tuberosity of the calcaneus as early as 1843. Different types of calcaneal avulsion fractures have been described by various authors since then.2,5
Fractures of the calcaneus are determined by the direction of the force and the position of the foot during the accident, as well as by the age of the patient, strength of the skeleton and tone of the muscles.2
Anatomy
Surgical anatomy reveals a variable tendo-achilles insertion into the posterior tuberosity of the calcaneus (Figure 7). In most cases insertion is to the middle third of the posterior tuberosity and there is a bursa between the tendon and the upper third of posterior tuberosity. Some people have a more extensive insertion of the tendo-achilles into the calcaneus.3
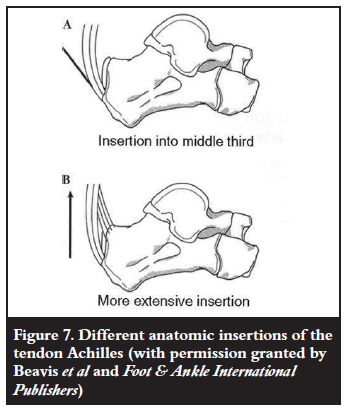
Neonates have a thick, continuous sheet of fibres connecting the Achilles tendon and the plantar fascia. With age the continuity between these two structures diminishes and this is demonstrated only as a zone of periosteum on the postero-inferior calcaneus between the Achilles tendon insertion and the plantar fascia attachment. Calcification of the retrocalcaneal bursa adjacent to the insertion could alter the actual zone of tendon attachment.3
Pathogenesis
These fractures are avulsion extra-articular fractures. Tuberosity avulsion fractures occur while the foot is in plantarflexion and the forces are transmitted through the tuberosity. They result from contraction of the gastrocnemius-soleus complex, often occurring after a lowimpact fall causing forced dorsiflexion, pulling the Achilles tendon, and causing avulsion of a fragment of bone.2,3,6
If the foot is in pronation during the fall, the whole tuberosity is involved.
When the force is transmitted to the bone from the loaded tendon, it is directed towards the plantar fascia by a series of high-oriented trabeculae. The superior fragment is displaced upwards, presumably due to the pull of tendo-achilles, and rotated so that the posterosuperior border moves upwards and the posteroinferior edge moves posteriorly, compressing the skin at the back of the heel. The fragment hinges on its anterior apex as it displaces so that a fracture which had minimal displacement anteriorly is often significantly displaced posteriorly, potentially giving rise to a heel boss, pressure necrosis and formation of an ulcer. This phenomenon explains the disability resulting from socalled 'undisplaced' fractures.4
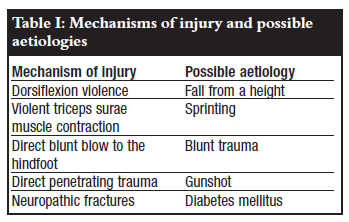
Mechanisms of injury and possible aetiologies has been described as shown in Table I1,3,4,7-9.
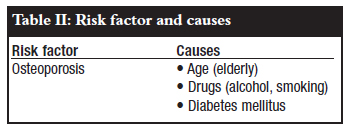
Risk factors
The major risk factor for these fractures is osteoporosis and its causes (Table II). There is little reference in the literature to these fractures in children and Sever's disease has been identified as a possible cause.10-13
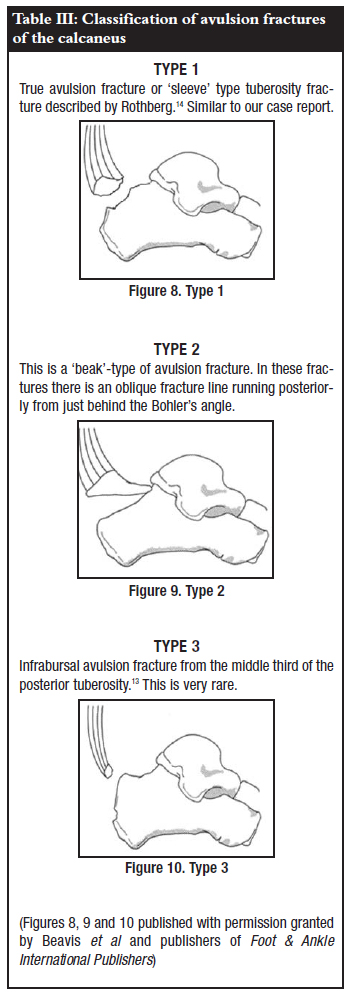
Classification
Classification of avulsion fractures of the calcaneus is shown in Table III and Figures 8-10.
Management
Management is governed by the age, health and functional demands of the patient as well as the degree of separation of the fracture fragments. With minimal or no displacement (< 1 cm), conservative treatment either in an equinus cast or a functional boot has yielded satisfactory results.1 This is accomplished by treatment in a short-leg equinus cast for six weeks non-weight-bearing. The patient is then gradually brought out of equinus and weight-bearing is increased. However, as with Achilles tendon ruptures that are treated in a cast, some patients are aware of diminished power of plantarflexion.
In displaced fractures skin necrosis as a result of pressure from the underlying fragment is a real danger. It should be remembered that the soft tissue overlying the tendon Achilles and calcaneal tuberosity is thin with a precarious blood supply. For these reasons these fractures should be treated as emergencies with open reduction and internal fixation.6 In our case the lateral-based flap incision may have contributed to poor blood supply and septic complication.
Methods of fixation include suturing of the avulsed bone fragment, suture anchors, tension band wiring and screw fixation as it was in our case.1,15 The choice of technique depends on the size of the avulsed bone fragment and the degree of osteopaenia.3
Screw fixation has been advocated; however, it should be kept in mind that these fractures are insufficiency fractures. Screw purchase in the bone is poor and healing takes longer to occur.
A better method of fixation would be tension band wiring as described by Brunner and Weber.16 In retrospect we should have used this method.
The fracture is then protected in a short-leg equinus cast for six to eight weeks, non-weight bearing until there is radiological evidence of bony union. After union, an ankle orthosis with a limiting up-stop is issued for up to one year. Union in this fracture has been reported in the literature from 10 weeks to a year 1,3
Neuropathic fractures takes longer to heal compared to traumatic fractures in young adults.8,9
Conclusion
Tuberosity avulsion fractures are rare. They represent a subset of calcaneal fractures that should be addressed urgently to avoid complications, particularly skin breakdown.
Non-operative treatment has been shown to yield poor results. The golden standard is surgical treatment.
References
1. Robb CA, Davies MB. A new technique for fixation of calcaneal tuberosity avulsion fractures. Foot and Ankle Surgery 2003;9:221-4. [ Links ]
2. Stockenhuber N, Wildburger R, Szyszkowitz R. Fractures of the os calcis. Current Orthopaedics 1996;10:230-8. [ Links ]
3. Beavis RC, Rouke K, Court-Brown C. Avulsion fracture of the calcaneal tuberosity. Foot & Ankle International 2008;29:863-6. [ Links ]
4. Squires B, Allen PE, Livingstone J, Atkins RM. Fractures of the tuberosity of the calcaneus JBJS [Br] 2001;83-B:55-61. [ Links ]
5. Schepers T, den Hartog D, Abida Z. Posterior capsular avulsion fracture of the calcaneus: an uncommon avulsion fracture. Journal of Foot & Ankle Surgery 2007;46(5):409-10. [ Links ]
6. Hess M, Booth B, Laughlin RT. Calcaneal avulsion fracture: complications from delayed treatment. American Journal of Emergency Medicine 2008;26:254. [ Links ]
7. Cooper DE, Heckman JD. The heel of Achilles: Calcaneal avulsion fracture from a gunshot wound. American Orthopaedic Foot & Ankle Society 1989;9(4/Feb). [ Links ]
8. Kathol MH, El-Khoury GY, Moore TE, Marsh JL, Calcaneal insufficiency avulsion fractures in patients with diabetes mellitus. Musculoskeletal Radiology 1991; 180(3):725-9. [ Links ]
9. Biell III WC, Morgan JM, Wagner WF, Gabriel R. Neuropathic calcaneal tuberosity avulsion fractures. CORR 1993 Nov;No269:8-13. [ Links ]
10. Cole J.R, Brown HP, et al. Avulsion fracture of the tuberosity of the calcaneus in children. JBJS 1995;7-A(10):1568-71. [ Links ]
11. Birtwistle SJ, Jacobs L. An avulsion fracture of the calcaneal apophysis in a young gymnast. International Journal of the Care of the Injured 1995;26(6). [ Links ]
12. Mooney V. Avulsion of the epiphysis of the os calcis. JBJS (A) 1935;17:1056-57. [ Links ]
13. Ogden JA, Ganey TM, Hill JD. Sever's injury: A stress fracture of the immature calcaneal metaphysis. J Paedtr Orthop 2004;24(5):488-92. [ Links ]
14. Rothberg AS. Avulsion fracture of the os calcis. J Bone Joint Surg [Am] 1939;21-A:218-20. [ Links ]
15. Khazen GE, Wilson AN, Ashfaq S, Parks BH. Fixation of calcaneal avulsion fractures using screws with and without suture anchors: A biomechanical investigation. The Journal of Foot & Ankle International 2007;28(11). [ Links ]
16. Brunner CF, Weber BG. Special techniques in internal fixation. Berlin: Springer-Verlag 1982, pp16-53. [ Links ]
 Reprint requests:
Reprint requests:
Dr M Radzilani
PO Box 224
0204 Medunsa
Tel: (012) 521-4005, Fax: (012) 521-4029
E-mail: mpho@ul.ac.za
No benefits of any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.














