Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.9 n.3 Centurion Jan. 2010
CLINICAL ARTICLE
Controversies in the management of tibial plateau fractures
PC Pelser
MBChB. Registrar, Department of Orthopaedic Surgery, University of the Free State
ABSTRACT
Over the past decades, a greater understanding of the mechanism of long-bone injury has led to a proliferation of treatments of these fractures. Various surgical techniques have been developed and enhanced, offering the modern-day surgeon a wide choice of fixation options and devices, all with their own indications, contraindications and potential problems. The treatment of the soft-tissue injuries that so often accompany tibial plateau fractures (TPFs) and the type of material that is best for the filling of subchondral defects after the reduction of depressed fractures are among a range of subjects that are also matters of controversy.
Based on a wealth of literature, this paper takes a critical look at the controversies that have developed regarding aspects of the classification, treatment modalities and prognosis of TPF with reference to related matters. After discussing each of these aspects of TPF separately, the author makes recommendations.
Introduction
Tibial plateau fractures (TPFs) represent a complex group of injuries that involve one of the major weight-bearing joints in the human body. Our understanding of the mechanism of injury, the associated injuries and the prognostic factors has evolved over the years.1,2 Accordingly there has been much advancement in the classification, evaluation, prognostication and especially treatment of these fractures. As with any evolving topic, many issues have not been settled and therefore some controversies regarding the management of TPF remain. This paper will review these controversies and aims to make recommendations according to the latest literature.
Controversies
Classification systems
In order to compare research and results and to aid in communication, treatment and determination of prognosis, a universal classification system of TPF is needed. The requirements of such a system would be reproducibility and reliability (both intra- and interobserver), ease of use and inclusiveness. Despite the abundance of available classification systems, none fully complies with all of the requirements. The Hohl and Moore3 classification fails to be inclusive of all fracture types, while a Turkish classification according to concomitant fibula fractures is mostly of prognostic value.4
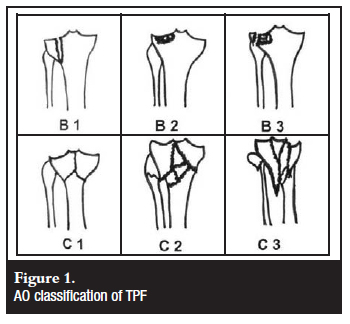
Both the AO (Arbeitsgemeinschaft für Osteosynthesefragen)5 (Figure 1) and Schatzker classifications6 (Figure 2) are widely used, but both show suboptimal reliability. Both classifications are, however, based on X-ray imaging only, and studies have shown that computer tomography (CT) and especially spiral CT (SCT) substantially improved the reliability of both classifications.7,8,9 Moreover, SCT with 3-dimensional reconstructions (3-D) significantly improved the treatment planning in complex TPF.7 Although the AO classification has been adopted by two major journals (JBJS and the Journal of Orthopaedic Trauma), the Schatzker classification has been shown to be superior with regard to interobserver and intra-observer reliability as well as ease of use and simplicity.3 Neither of these systems includes dislocations or associated soft-tissue injuries.

Recommendation
Familiarity with any one classification will lead to better reliability, therefore a surgeon or institution should adopt either the AO or Schatzker classification and use it consistently. If plain X-rays fail to facilitate classification of a fracture, or in complex fractures, CT or SCT 3-D should be obtained. Attention must be paid to associated injuries and dislocations. For research and publication purposes, it seems to be prudent to include both classification systems.
Imaging and radiology
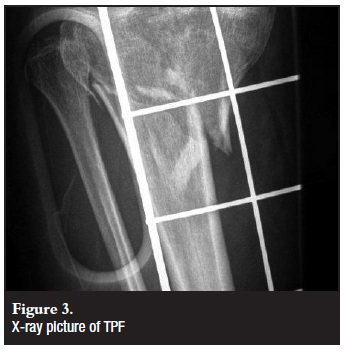
Radiological evaluation of TPF always commences with a trauma series of X-rays (XR) (Figure 3). These will routinely include anteroposterior (AP), lateral and oblique views.2 Due to the complex nature of these injuries and the high incidence of associated injuries, further imaging is often necessary. The role of CT and MRI (magnetic resonance imaging) is still controversial to some extent.
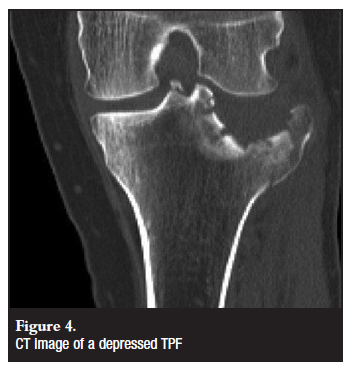
CT is more effective in demonstrating the fracture anatomy (Figure 4) and amount of fragments than XR and has been shown to increase the accuracy of fracture classification and surgical planning.7 This is especially true for complex and bicondylar TPF. According to Mui et al, CT can even be utilised to exclude ligament injury.10 SCT delivers a lower XR dose than conventional XR tomographic studies.7
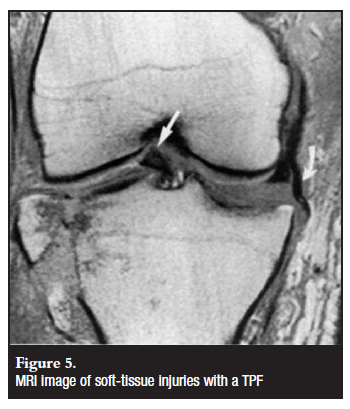
MRI has a high sensitivity for demonstrating soft-tissue injuries (Figure 5) and is also effective in demonstrating the fracture pattern.10 Due to the high rate of concomitant soft-tissue injuries in TPF, there is a move towards more frequent MRI studies.11 The limitations to this approach are the high cost of MRI and its limited availability.
Recommendation
Standard AP, lateral and oblique XR films must form the basis for diagnosis, classification and surgical planning in TPF. CT and SCT-3D are indicated in complex fractures (Schatzker 4-6) or where classification and surgical planning cannot be made on XR alone. It is also used to diagnose hidden fractures not seen on XR. MRI is most useful for the pre-operative diagnosis of meniscus and ligamentous injuries in TPF that would otherwise have been treated percutaneously or conservatively.12
XR tomography has been replaced by SCT-3D.
Indications for surgical treatment
There is general consensus in the literature that TPFs that are stable and show minimal displacement do not require surgery.6,13,14 Contraindications to surgery have also been well established, namely severe soft-tissue swelling, active infection near the fracture site, comorbid conditions that preclude anaesthesia or appropriate postoperative rehabilitation, as well as surgeon or implant incapability to address the injury.13
The precise amount of fracture displacement, angulation, articular depression and condylar widening as well as associated soft-tissue injuries that require surgical intervention are still matters of debate. The main reason for this is the lack of correlation between the abovementioned parameters and the clinical outcome.15-20 This is further confounded by patient age, health status and functional demands. Despite all these variables, there are some indications for surgery that seem to be well accepted.13,15
Recommendation
Fracture-specific indications for surgery are the following:
• intra-articular step-off of more than 2 mm
• condylar widening of more than 5 mm
• angulation (varus-valgus or sagittal) more than 5º
Other indications for surgery would be:
• associated compartment syndrome
• ipsilateral tibia or fibula fractures
• compound fractures
The appropriate management should be individualised in each case according to these guidelines and patientspecific factors.
Surgical technique and fixation modalities
Various surgical techniques and approaches have been described, all with their own advantages and disadvantages. Likewise, numerous fixation options and devices are available, all with their own indications, contraindications and potential problems. The treatment of associated soft-tissue injuries and variable options for cancellous defect augmentation are also matters of controversy.
Approach and incision
Due to the relative subcutaneous nature of the tibia and the associated soft-tissue injuries with TPF, there is a high risk for wound complications.2,21,23 The matter is complicated by the need for excellent reduction and fracture visualisation, stable fixation and the extent of the fracture. The amount of soft-tissue dissection necessary with single or double incisions varies significantly. When the likelihood of future knee arthroplasty is also taken into consideration it becomes clear that the surgical approach in TPF is of utmost importance.
Although a single anterior incision allows access to both tibial condyles and has the fewest implications for future arthroplasty surgery, it necessitates extensive soft-tissue dissection and has the potential of wound complications.21,24 A dual-incision approach for double plating reduces the risk of wound breakdown when compared to a single incision due to more direct access to the fracture and less dissection.18,22 Locking-plate technology might obviate the need for medial exploration and instrumentation and allow minimallyinvasive techniques through an anterolateral incision in many bicondylar TPFs.2,24,25,26
Recommendation
A two-incision approach centred over the fragments but not directly over the plates is recommended for bicondylar TPFs that are not amenable to lateral locking-plate fixation alone. Care must be taken to leave an adequate skin gap between the incisions.
A single anterolateral incision is sufficient for fractures that can be stabilised with lateral buttress plating or locking plates and the dissection can be further minimised by using minimally invasive techniques.
A posteromedial incision is indicated for medial fracture-dislocations, posteromedial-plateau fractures and posterior metaphyseal-wedge fractures.
Raft screws
Treatment of split-depression fractures of the lateral plateau (Schatzker 2 and 3) entails reduction of the articular surface and augmentation of the subsequent cancellous cavity. Fixation can then be accomplished by subchondral parallel screws with or without a lateral buttress plate. Traditionally two large-fragment 6.5 mm cancellous lag screws were used, but alternative methods utilising small-fragment 3.5 mm screws have been described,1,27,28 as well as cannulated screws and arthroscopic assistance.29,30 Biomechanical studies show that smaller screws placed nearer to the subchondral bone have adequate construct stiffness while providing greater support to prevent depression and more favourable elasticity underneath the articular cartilage than larger screws.27
Recommendation
Buttress plating in Schatzker-type 1, 2 and 3 fractures to support raft-screw fixation is necessary for all TPFs with poor bone quality or fragment instability.2,29
A raft made up of four parallel 3.5 mm cortical screws is advisable for depressed TPFs with good bone stock and adequate augmentation of the defect.27,28
Lateral locking plate in medial TPF
Medial TPF (Schatzker 4) treatment traditionally entailed medial buttress plating, but the problem of prominent hardware and the ease of use of laterally placed minimally invasive locking plates has challenged this treatment option. Buttress plating has been shown to allow less displacement of medial fragments than conventional lateral plating,31 but fixed-angle plates have greater stability than regular tension-band lateral plating.32 The size and position of the medial fragment determines whether lateral locking-plate fixation will have an adequate grip and stabilising effect on medial TPF.33 Inadequate stabilisation of these fractures will lead to varus deformity of the tibia.12
Recommendation
Medial buttress plating through an anteromedial approach is indicated for isolated medial plateau fractures. Lateral locking plates are best suited for bicondylar fractures.
Lateral locking plate vs dual plating in bicondylar TPF
Lateral locking-plate fixation for bicondylar TPF has the advantage of a single lateral incision and therefore no devascularisation of the medial fragment and reduced wound complications.24 The fixed-angle construct is thought to have sufficient stability to treat these unstable fractures.2,25,34,35 Medial and lateral buttress plating with the resultant 'dead-bone sandwich' (Figure 6) has, however, been replaced by anteromedial anti-gliding plate and lateral buttress-plate combinations with less soft-tissue complications.36 This technique has the advantage over locking plates in that interfragmentary compression can be achieved through the plate and screws, and dual plating still remains the most rigid construct to treat bicondylar TPF.2,25 Some studies suggest that the use of a lateral locking plate alone involves a higher risk of loss of reduction and malunion than dual plating.2,24,37

Recommendation
Although dual plating remains an effective form of treatment for bicondylar TPF, lateral locking plates (especially when combined with interfragmentary screws) is a good alternative, especially for high-energy injuries with severe soft-tissue compromise and medial wounds, as well as in osteoporotic fractures or poor bone quality (Figure 7).

The fracture configuration must be taken into consideration when applying lateral locking plates in order to recognise the need for alternative or additional fixation devices such as interfragmentary screws and posteromedial anti-gliding plates.33
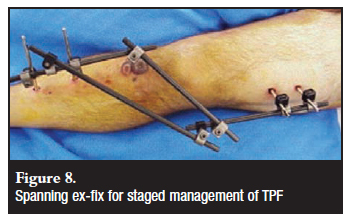
External fixation
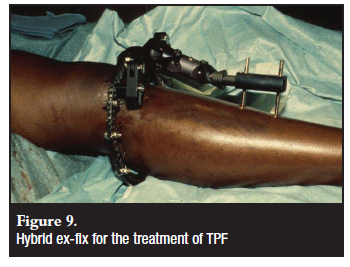
The use of spanning external fixators as part of the staged management of TPF, especially in high-energy injuries (Figure 8), is well established.22 A high index of suspicion should, however, be maintained for the development of compartment syndrome after restoration of length, and the foot should not be incorporated into the frame to facilitate clinical evaluation for compartment syndrome.38 Some controversy remains, however, about the role of external fixators with or without minimal internal fixation and ring or fine-wire/Ilizarov frames. Although soft-tissue dissection and therefore also complications can be minimised with the use of external fixators, the maintenance of reduction can be problematic.39 Pin-track sepsis might be easily managed in most cases,19 but joint capsule penetration with resultant septic arthritis can be a major cause of morbidity.23 Dormant infection after pin-track sepsis will be a concern in future arthroplasty, but limited soft-tissue dissection and less hardware and scarring will be beneficial.18 Articular reduction and the identification and treatment of associated soft-tissue injuries are less effectively achieved through external fixation techniques, but this does not seem to cause any deterioration in the clinical outcome as compared to open reduction and internal fixation (ORIF).16,18,19 A shorter duration of hospital stay and fewer complications with external fixation have to be weighed against patient discomfort and potential loss of motion.2 Fine wire-ring fixation seems to be stronger than hybrid devices (Figure 9) or monolateral fixators, and compares favourably with double-plating techniques.40
Recommendation
Fine wire-ring fixators (Ilizarov frames) are a good option in the treatment of TPF with extensive soft-tissue damage, severe metaphyseal-diaphyseal comminution, extension into the tibial shaft and limited intra-articular displacement.13 Articular reduction and fixation can be achieved by olive wires or minimal ORIF with percutaneous lag screws. Placement and care of pins must be meticulous to avoid complications. Pins must be placed outside the joint capsule and away from future sites of internal fixation.
Arthroscopy
Arthroscopic reduction and internal fixation (ARIF) in the treatment of TPF is reported to have fewer complications than ORIF, but since the technique has mostly been used in less severe fractures, this finding might be insignificant. The increase in theatre time might increase the risk of infective and thrombotic complications, but is off-set by faster rehabilitation and decreased hospital stay.23,41 Fluid leakage and lower-leg compartment syndrome is a very real danger, but if the technique is applied carefully and correctly this can be prevented.14,29 Intra-articular visualisation aids in more precise fracture reduction, but adequate fixation and the application of bone graft or substitutes for depressed fractures remain essential for preventing displacement and poor outcome.14,23 One of the most claimed advantages of ARIF is the ability to treat associated intra-articular lesions like meniscus tears, but the acute reconstruction of anterior cruciate ligament (ACL) injuries is not recommended due to the additional soft-tissue damage.14
Recommendation
ARIF remains an adjunct and non-essential technique in the treatment of low-energy TPF. Fluid inflow must be gravitational only and an early bone window through an anteromedial incision is recommended to enhance outflow.29 Appropriate and adequate fixation must still be employed. Repair of tibial spine fractures, removal of small osteochondral fragments and debridement or repair of meniscus injuries can be done effectively.
Bone graft and substitutes
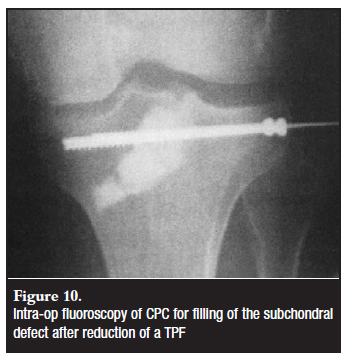
The filling of subchondral defects after reduction of depressed fractures is generally accepted as necessary, but the type of material is still controversial.2 Taking autogenous cancellous bone graft (usually from the iliac crest) has been standard practice, but the use of calcium phosphate cement (CPC), calcium sulphate, freeze-dried cancellous allograft, bovine xenograft and even trabecular metal has been proposed.42-45 Iliac-crest graft harvesting is marred by the possibility of donor site morbidity and complications, but it remains the cheapest and most readily available option.46 Yet, the total cost of treatment with CPC might actually be lower than that of autograft-treated patients due to faster rehabilitation and a shorter hospital stay.47
Although the proximal tibial metaphysis has been shown to be a reliable donor site48 it is of doubtful use in the scenario of acute TPF. For the treatment of TPF non-unions, autograft remains the golden standard.49,50
Studies have shown the stiffness and compressive strength of calcium phosphate and sulphate cement to be better than that of cancellous bone and therefore less fracture subsidence and even earlier weight bearing is possible.42,51 Calcium sulphate has become available in an injectable formula but the exothermic effect on the overlying chondrocytes is still to be determined. The rapid resorption rate has the advantage that intra-articular extravasation does not need to be removed.42 Tricalcium phosphate (TCP) granules have faster bone integration than calcium phosphate, but do not allow immediate stability and have sub-optimal cavity filling.52 The newer CPC cures rapidly with an isothermic reaction, but slow absorption and incorporation necessitate the removal of intra-articular spillage.4,53 Unlike allografts, CPC carries no risk for disease transmission, and no adverse wound effects have been reported.46,47,54-56
Osteochondral allograft can be successfully utilised in the treatment of articular defects after TPF, but is not indicated in the acute management of these fractures.57
Recommendation
Autogenous cancellous bone graft remains the golden standard in the treatment of depressed TPF. Injectable CPC is a viable alternative with obvious support from the industry. Careful application of CPC under fluoroscopic control (Figure 10) will effectively fill the subchondral gap with early stability, permitting faster rehabilitation. Stable fixation of the fracture should still be performed according to general guidelines.
Treatment of associated soft-tissue injuries
Soft-tissue injuries associated with TPF are numerous and common, despite variable incidence reports in the literature.1,2,18,20,29,30,58 The most common findings are ACL injuries, lateral and medial meniscus lesions, collateral ligament injuries, posterior cruciate ligament injuries and patella-tendon avulsion. Popliteal artery injuries are rare but must not be missed. Likewise, peroneal nerve injuries are mostly associated with fracture-dislocation type injuries. Although accelerated post-traumatic osteoarthritis (OA) is seen in unstable knees after TPF,23 clinical outcomes are similar for patients with and without initial intra-articular soft-tissue repair.18 Instability in the acute setting is difficult to confirm due to the underlying fracture, and as a late complication instability can be the cause or result of post-traumatic OA.59 Meniscus injuries are often detachments or in the red zone and therefore repairable,14,60 while meniscectomy is associated with a poor outcome.23,59 Fracture type, configuration and depression do not correlate with the incidence of meniscus injury, but MRI is both sensitive and specific for diagnosis.11 ACL repair is not advised in the acute setting and, due to arthrofibrosis, ACL-deficient knees may not show significant instability to necessitate reconstruction.41
Recommendation
Avulsion fractures need to be repaired as part of the initial management of TPF. Meniscus injuries can be repaired through open techniques or arthroscopy, but meniscectomy is contraindicated. Most collateral-ligament injuries have an acceptable outcome with conservative treatment. Likewise, ACL injuries only need secondary reconstruction if the knee is unstable after rehabilitation.
Pre-operative and postoperative assessment of the vascular and neurological status of the affected leg is of utmost importance at first presentation.
Rehabilitation
The principle of stable fixation and early movement is of particular importance in TPF. Early range-of-motion exercises and continuous passive movement are used to prevent arthrofibrosis. The speed at which weight bearing can be allowed is, however, controversial.61 Reports in the literature vary from partial weight bearing at two days postoperatively47 to full weight bearing (FWB) at 6 to 8 weeks1,39 and up to 12 weeks.17,24 The convention is for FWB to be commenced at 6 weeks, but this might not be applicable for all fracture types and all patient groups.
Recommendation
Depression fractures should remain non-weight bearing (NWB) for 6 weeks, unless they are low-energy injuries treated with calcium phosphate cement, in which case partial weight bearing can be allowed as pain permits. High energy, unstable fracture patterns are best kept NWB until signs of union are visible, usually around 8 to 12 weeks postoperatively. Range of motion exercises are best started 10 to 14 days postoperatively to allow wound stabilisation.
Future developments
The use of computer-assisted surgery (CAS) to obtain optimal alignment and the role of cartilage regeneration in the treatment of post-traumatic OA are areas of treatment that await further research.
References
1. Burri C, Bartzke G, Coldewey J, Muggler E. Fractures of the tibial plateau. Clin Orthop 1979; 138: 84-94. [ Links ]
2. Musahl V, Tarkin I, Kobbe P, Tzioupis C, Siska PA, Pape H-C. New trends and techniques in open reduction and internal fixation of fractures of the tibial plateau. J Bone Joint Surg [Br] 2009; 91-B: 426-33. [ Links ]
3. Maripuri SN, Rao P, Manoj-Thomas A, Mohanty K. The classification systems for tibial plateau fractures: How reliable are they? Injury 2008; 39:1216-21. [ Links ]
4. Bozkurt M, Turanli S, Doral MN, Karaca S, Dogan M, Sesen H, Basbozkurt M. The impact of proximal fibula fractures in the prognosis of tibial plateau fractures: a novel classification. Knee Surg Sports Traumatol Arthrosc 2005; 13: 323-8. [ Links ]
5. Murphy WM, Leu D. Fracture classification: biological significance. In: Ruedi TP, Murphy WM (eds). AO Principles of fracture management. Thieme; 2000: 46-53. [ Links ]
6. Schatzker J, McBroom R. The tibial plateau fracture: The Toronto experience 1968-1975. Clin Orthop 1979; 138: 94-104. [ Links ]
7. Wicky S, Blaser PF, Blanc CH, Leyvraz PF, Schnyder P, Meuli RA. Comparison between standard radiology and spiral CT with 3D reconstruction in the evaluation, classification and management of tibial plateau fractures. Eur Radiol 2000; 10: 1227-32. [ Links ]
8. Walton NP, Harish S, Roberts C, Blundell C. AO or Schatzker? How reliable is classification of tibial plateau fractures? Arch Orthop Trauma Surg 2003; 123: 396-8. [ Links ]
9. Hu Y-L, Ye F-G, Ji A-I, Qiao G-X, Liu H-F. Three-dimensional computer tomography imaging increases the reliability of classification systems for tibial plateau fractures. Injury 2009; 40: 1282-5. [ Links ]
10. Mui LW, Engelsohn E, Umans H. Comparison of CT and MRI in patients with tibial plateau fracture: can CT findings predict ligament tear or meniscal injury? Skeletal Radiol 2007; 36: 145-51. [ Links ]
11. Mustonen AOT, Koivikko MP, Lindahl J, Koskinen SK. MRI of acute meniscal injury associated with tibial plateau fractures: Prevalence, type, and location. AJR 2008; 191: 10021009. [ Links ]
12. Jacofsky DJ, Haidukewych GJ. Tibial Plateau Fractures. In: Scott WN. Insall & Scottsurgery of the knee. Churchill Livingstone: Elsevier; 2006: 1133-46. [ Links ]
13. Hall JA, Beuerlein MJ, McKee MD, and the Canadian Orthopaedic Trauma Society. Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures surgical technique. J Bone Joint Surg [Am] 2009; 91 Suppl 2 (part 1): 74-88. [ Links ]
14. Hung S, Chao E-K, Chan Y-S, Yuan L-J, Chung P C-H, Chen C-y, Lee MS, Wang C-J. Arthroscopically assisted osteosynthesis for tibial plateau fractures. J Trauma 2003; 54: 356-63. [ Links ]
15. Ali AM, El-Shafie M, Willet KM. Failure of fixation of tibial plateau fractures. J Orthop Trauma 2002; 16: 323-9. [ Links ]
16. Mahadeva D, Costa ML, Gaffey A. Open reduction and internal fixation versus hybrid fixation for bicondylar tibial plateau fractures: A systematic review of the literature. Arch Orthop Trauma Surg 2008; 128: 1169-75. [ Links ]
17. Barei DP, Nork SE, Mills WJ, Coles CP, Henley MB, Benirschke K. Functional outcomes of severe bicondylar tibial plateau fractures treated with dual incisions and medial and lateral plates. J Bone Joint Surg [Am] 2006; 88-A: 1713-21. [ Links ]
18. Canadian Orthopaedic Trauma Society. Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures. J Bone Joint Surg [Am] 2006; 88-A: 2613-24. [ Links ]
19. Chin T Y-P, Bardana D, Bailey M, Williamson OD, Miller R, Edwards ER, Essre MP. Functional outcome of tibial plateau fractures treated with fine-wire fixator. Injury 2005; 36: 1467-75. [ Links ]
20. Delamarter RB, Hohl M, Hopp E. Ligament injuries associated with tibial plateau fractures. Clin Orthop 1990; 250: 226-33. [ Links ]
21. Stevens DG, Beharry R, McKee MD, Waddell JP, Schemitsch EH. The long-term functional outcome of operatively treated tibial plateau fractures. J Orthop Trauma 2001; 15: 312-21. [ Links ]
22. Barei DP, Nork SE, Mills WJ, Henley MB, Benirschke SK. Complications associated with internal fixation of high-energy bicondylar tibial plateau fractures utilizing a two-incision technique. J Ortop Trauma 2004; 18: 649-57. [ Links ]
23. Papagelopoulos PJ, Partsinevelos AA, Themistocleous GS, Mavrogenis AF, Korres DS, Soucacos PN. Complications after tibia plateau fracture surgery. Injury 2006; 37: 475-84. [ Links ]
24. Jiang R, Luo C-F, Wang M-C, Yang T-Y, Zeng B-F. A comparative study of Less Invasive Stabilization System (LISS) fixation and two-incision double plating for the treatment of bicondylar tibial plateau fractures. The Knee 2008; 15: 139-43. [ Links ]
25. Egol KA, Su E, Tejwani NC, Sims SH, Kummer FJ, Koval KJ. Treatment of complex tibial plateau fractures using the less invasive stabilization system plate: clinical experience and laboratory comparison with double plating. J Trauma 2004; 57: 340-6. [ Links ]
26. Russel N, Tamblyn P, Jaarsma R. Tibial plateau fractures treated with plate fixation: To lock or not to lock. Eur J Orthop Surg Traumatol 2009; 19: 75-82. [ Links ]
27. Karunakar MA, Egol KA, Peindl R, Harrow ME, Bosse MJ, Kellam JF. Split depression tibial plateau fractures: A biomechanical study. J Orthop Trauma 2002; 16: 172-7. [ Links ]
28. Patil S, Mahon A, Green S, McMurray I, Port A. A biomechanical study comparing a raft of 3.5mm cortical screws with 6.5mm cancellous screws in depressed tibial plateau fractures. The Knee 2006; 13: 231-5. [ Links ]
29. Rossi R, Bonasia DE, Blonna D, Assom M, Catoldi F. Prospective follow-up of a simple arthroscopic-assisted technique for lateral tibial plateau fractures: Results at 5 years. The Knee 2008; 15: 378-83. [ Links ]
30. Gill TJ, Moezzi DM, Oates KM, Sterett WI. Arthroscopic reduction and internal fixation of tibial plateau fractures in skiing. Clin Orthop 2001; 383: 243-9. [ Links ]
31. Wu C-C, Tai C-L. Plating treatment for tibial plateau fractures: A biomechanical comparison of buttress and tension band positions. Arch Orthop Trauma Surg 2007; 127: 19-24. [ Links ]
32. Ratcliff JR, Werner FW, Green JK, Harley BJ. Medial buttress versus lateral locked plating in a cadaver medial tibial plateau fracture model. J Orthop Trauma 2007; 21: 444-8. [ Links ]
33. Barei DP, O'Mara TJ, Taitsman LA, Dunbar RP, Nork SE. Frequency and fracture morphology of the posteromedial fragment in bicondylar tibial plateau fracture patterns. J Orthop Trauma 2008; 22: 176-83. [ Links ]
34. Gosling T, Schandelmaier P, Marti A, Hufner T, Partenheimer A, Krettek C. Less invasive stabilization of complex tibial plateau fractures. J Orthop Trauma 2004; 18: 546-51. [ Links ]
35. Mueller KL, Karunakar MA, Frankenburg EP, Scott DS. Bicondylar tibial plateau fractures: a biomechanical study. Clin Orthop 2003; 412: 189-95. [ Links ]
36. Horwitz DS, Bachus KN, Craig MA, Peters CL. A biomechanical analysis of internal fixation of complex tibial plateau fractures. J Orthop Trauma 1999; 13: 545-9. [ Links ]
37. Higgins TF, Klatt J, Bachus KN. Biomechanical analysis of bicondylar tibial plateau fixation: How does lateral locking plate fixation compare to dual plate fixation? J Orthop Trauma 2007; 21: 301-6. [ Links ]
38. Stark E, Stucken C, Trainer G, Tornetta P. Compartment syndrome in Schatzker Type VI plateau fractures and medial condylar fracture-dislocations treated with temporary external fixation. J Orthop Trauma 2009; 23: 502-6. [ Links ]
39. Subasi M, Kapukaya A, Arslan H, Ozkul E, Cebesoy O. Outcome of open comminuted tibia plateau fractures treated using an external fixator. J Orthop Sci 2007; 12: 347-53. [ Links ]
40. Ali AM, Saleh M, Bolongaro S, Yang L. The strength of different fixation techniques for bicondylar tibial plateau fractures: A biomechanical study. Clin Biomech 2003; 18: 864-70. [ Links ]
41. Ohdera T, Tokunaga M, Hiroshima S, Yoshimoto E, Tokunaga J, Kobayashi A. Arthroscopic management of tibial plateau fractures: Comparison with open reduction method. Arch Orthop Trauma Surg 2003; 123: 489-93. [ Links ]
42. Yu B, Han K, Zhang C et al. Treatment of tibial plateau fractures with high strength injectable calcium sulphate. Int Orthop 2009; 33: 1127-33. [ Links ]
43. Lasanianos N, Mouzopoulos G, Garnavos C. The use of freeze-dried cancellous allograft in the management of impacted tibial plateau fractures. Injury 2008; 39: 1106-12. [ Links ]
44. Bansal MR, Bhagat SB, Shukla DD. Bovine cancellous xenograft in the treatment of tibial plateau fractures in elderly patients. Int Orthop 2009; 33: 779-84. [ Links ]
45. Benoit B, Fouad Z, Laflamme G-H et al. Augmentation of tibial plateau fractures with Trabecular Metal: a biomechanical study. J Orthop Surg Research 2009; 4: 37. [ Links ]
46. Bajammal SS, Zlowodski M, Lelwica A et al. The use of calcium phosphate bone cement in fracture treatment. J Bone Joint Surg [Am] 2008; 90: 1186-96. [ Links ]
47. Lobenhoffer P, Gerich T, Witte F, Tscherne H. Use of injectable calcium phosphate bone cement in the treatment of tibial plateau fractures: A prospective study of twenty-six cases with twenty-month mean follow up. J Orthop Trauma 2002; 16: 143-9. [ Links ]
48. Alt V, Meeder P-J, Seligson D et al. The proximal tibia metaphysis: A reliable donor site for bone grafting? Clin Orthop 2003; 414: 315-21. [ Links ]
49. Wu C-C. Salvage of proximal tibial malunion or nonunion with the use of angled blade plate. Arch OrthopTrauma Surg 2006; 126: 82-7. [ Links ]
50. Toro-Arbelaez J, Gardner MJ, Shindle MK et al. Open reduction and internal fixation of intraarticular tibial plateau nonunions. Injury 2007; 38: 378-83. [ Links ]
51. Yetkinler DN, McClellan RT, Reindel ES et al. biomechanical comparison of conventional open reduction and internal fixation versus calcium phosphate cement fixation of a central depressed tibial plateau fracture. J Orthop Trauma 2001; 15: 197-206. [ Links ]
52. Shen C, Ma J, Chen X-D, Dai L-Y. The use of ß-TCP in the surgical treatment of tibial plateau fractures. Knee Surg Sport Traumatol Arthrosc 2009; 17: 1406-11. [ Links ]
53. Welch RD, Zhang H, Bronson DG. Experimental tibial plateau fractures augmented with calcium phosphate cement or autologous bone graft. J Bone Joint Surg [Am] 2003; 85-A: 222-31. [ Links ]
54. Horstmann WG, Verheyen CCPM, Leemans R. An injectable calcium phosphate cement as a bone graft substitute in the treatment of displaced lateral tibial plateau fractures. Injury 2003; 34: 141-4. [ Links ]
55. Simpson D, Keating JF. Outcome of tibial plateau fracture managed with calcium phosphate cement. Injury 2004; 35: 913-8. [ Links ]
56. Russel TA, Leighton RK. Comparison of autogenous bone graft and endothermic calcium phosphate cement for defect augmentation in tibial plateau fractures: A multicenter, prospective, randomized study. J Bone Joint Surg [Am] 2008; 90-A: 2057-61. [ Links ]
57. Shasha N, Krywulak S, Backstein D et al. Long-term follow-up of fresh tibial osteochondral allografts for failed tibial plateau fractures. J Bone Joint Surg [Am] 2003; 85-A Suppl 2: 33-9. [ Links ]
58. Blokker CP, Rorabeck CH, Bourne RB. Tibial plateau fractures: An analysis of the results of treatment in 60 patients. Clin Orthop 1984; 182: 193-199. [ Links ]
59. Honkonen SE. Degenerative arthritis after tibial plateau fractures. J Orthop Trauma 1995; 9:273-7 [ Links ]
60. Barrett MO, Kazmier P, Anglen JO. Repair or reattachment of the meniscusafter fixation of a tibial plateau fracture. J Orthop Trauma 2005; 19:198-200. [ Links ]
61. Hsu C-J, Chang W-N, Wong C-Y. Surgical treatment of tibial plateau fracture in elderly patients. Arch Orthop Trauma Surg 2001; 121:67-70. [ Links ]
 Reprint requests:
Reprint requests:
Dr PC Pelser
Private Bag X20598
9300 Bloemfontein South Africa
Tel: (051) 405-2242, Fax: (051) 430-7101
The content of the article is the sole work of the author. No benefits of any form have been or are to be received from a commercial party related directly or indirectly to the subject of the article.














