Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.9 n.3 Centurion Jan. 2010
CLINICAL ARTICLE
Known primary with secondary disease: is tissue diagnosis necessary?
IJ VlokI; RN DunnII
IMBChB(US), MMed(US), FC Neurosurgery. AOSpine Fellow
IIMBChB(UCT), MMed(UCT), FCS(SA)Orth. Consultant Orthopaedic and Spine Surgeon, Associate Professor, University of Cape Town, Head Orthopaedic Spine Services: Groote Schuur Hospital
ABSTRACT
Spinal metastasis as the presenting problem is frequently encountered in oncological practice. This scenario is often complicated by an unknown primary or a previously diagnosed primary some years before. Once identified, the primary is often more accessible than the spine metastasis in terms of biopsy. This raises the issue of whether the metastatic lesion's histology can be inferred from the previously known primary or in fact the current primary's histology.
A case is reported which highlights the inherent risks of these assumptions. It identifies the need for adequate specimen when performing a biopsy. The limits of fine needle biopsy must be recognised. Involvement of the cervico-thoracic junction should be recognised as an unstable area with early aggressive surgical intervention necessary to stabilise and prevent deformity and associated neural compression. Finally, local metastatic tissue should always be sent for histological assessment.
Introduction
Spinal metastasis as the presenting problem is frequently encountered in oncological practice as 10% of tumours metastasise to the spine. This scenario is often complicated by an unknown primary or a previously diagnosed primary some years before.
Once identified, the primary is often more accessible than the spine metastasis in terms of biopsy. This raises the issue of whether the metastatic lesion's histology can be inferred from the previously known primary or in fact the current primary's histology.
A case is reported which highlights the inherent risks of these assumptions. As always, clinical practice is based on probability and has the potential for surprise, necessitating an open mind in terms of differential diagnosis.
Case report
A 70-year-old woman presented to a private neurologist with complaints of interscapular pain and paraesthesia in her right hand. The diagnosis of a C8 sensory radiculopathy was made. A right-sided thyroid mass was noted clinically. Financial restrictions dictated follow-up at a government tertiary institution by the Departments of General Surgery and Neurosurgery where a fine needle aspiration (FNAB) of the thyroid mass was performed. At this time the patient had a normal neurological status.
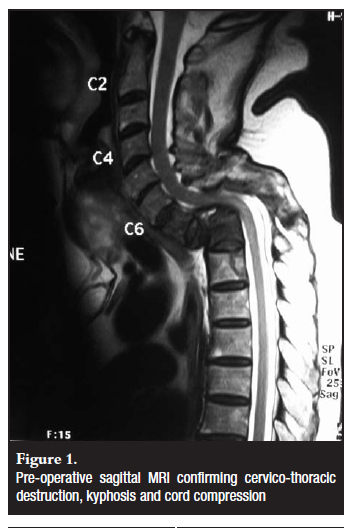
Two weeks later she deteriorated neurologically and was unable to ambulate. A MRI scan revealed a kyphotic deformity and destruction of the C7 and T1 vertebrae (Figure 1). The thyroid was homogenously enlarged and adjacent to the affected C7 and T1 vertebrae. The FNAB cytology reported atypical follicular cells and the diagnosis of 'suspected follicular thyroid carcinoma with metastatic disease' made. The patient was admitted and a multidisciplinary review followed based on a working diagnosis of metastatic thyroid carcinoma.
At this point she could stand but was unable to walk. There was no clear sensory level. She had increased tone in her lower limbs but normal tone and power in her upper limbs. In both lower limbs hip extension and knee extension was 4/5 with ankle plantarflexion 2/5. Ankle dorsiflexion, knee and hip flexion were all 1/5. She was hyper-reflexic in her lower limbs with bilateral persistent clonus and Babinski responses. No Hoffman's responses could be detected. She had intact bladder and bowel function.
A bone scan revealed increased uptake in the vertebral bodies as seen on the MRI with a further small focus of increased uptake in her skull in the left parietal area. She was euthyroid. In consultation with the Department of Oncology it was decided that the tumour and metastatic disease could be successfully treated but a debulking of the mass would make it more effective. The patient was referred to the spinal surgery unit at another hospital for further management.
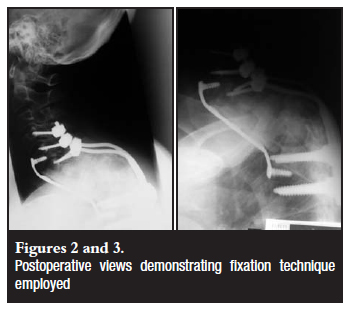
Due to her clinical deterioration a second MRI scan was done revealing further collapse and deformity of her cervico-thoracic spine.1,2 The decision was made to decompress and fuse the spine in situ with a thyroidectomy at the same sitting. The cervico-thoracic spine was exposed via a posterior approach. It was fixed with lateral mass fixation of C4-C6 and pedicular fixation of T4 and T5. Laminectomies of C6-T3 were performed. The patient was turned and a thyroidectomy performed by the general surgeons. A left inverted breast nipple was noted. The patient had attributed this to a history of ductitis 30 years ago on pre-operative enquiry but the general surgeons decided to perform a biopsy of the retro-areolar breast tissue. Through the thyroid bed, C7-T3 corpectomies were performed and the spinal cord decompressed. A fibula allograft was placed and supported with an anterior locking plate between C6 and T4 (Figure 2 and 3).3
Her postoperative course was uneventful and she showed a steady increase in power in her lower limbs. Her histological reports of the thyroid revealed a benign follicular adenoma despite the previous malignant cytology. The breast biopsy revealed a diagnosis of invasive breast ductal carcinoma and the vertebral bodies resected demonstrated metastatic breast ductal carcinoma.
She was referred to oncology. The tumour responded well to hormone therapy. At her 6-month postoperative follow-up she was walking without support and had regained full power in her legs.
Discussion
Follicular thyroid cancer presents as a slow-growing thyroid nodule or occasionally with local symptoms. They have a 10-year survival rate of 80-95% but with the presence of distal metastases it decreases to 40%.1 More than 80% of skeletal metastases from follicular thyroid carcinoma occur in the axial skeleton where marrow blood flow is high (vertebrae, hips, ribs). Approximately 25% of these tumours have extra-thyroid invasion at the time of diagnosis.1
It is not possible to distinguish whether a patient has malignant thyroid cancer on clinical assessment in the absence of metastatic disease. The most common next investigation is fine needle aspiration (FNAB). It is a safe, useful and cheap tool in the diagnosis of thyroid pathology.
The diagnostic sensitivity is known to be approximately 80% but has been reported as low as 66% in some studies.2 Thus the use of FNAB in a palpable thyroid nodule could misdiagnose up to a third of malignancies. FNAB will diagnose follicular cells, but because it only evaluates cellular features it cannot comment on whether a tumour is benign or malignant. FNAB positive for follicular cells only have a 20% malignancy rate.3 The definitive step in finalising the diagnosis is surgical resection of the lesion and vascular and capsular invasion is histologically evaluated.
With regard to the spine metastasis management, the decision to decompress and stabilise the rapidly progressive deformity with a compromised thoracic spinal cord was based on the premise of a treatable condition with a good prognosis. This was based on a single fine needle biopsy with no definitive histological confirmation. The location of the thyroid mass adjacent to the affected vertebrae erroneously confirmed the treating surgeon's belief that they were related. The suspicious area of the breast was attributed to a ductitis 30 years ago as volunteered by the patient. Due to the suggested chronicity of the breast lesion, no suspicion was raised. With the average survival rate of breast carcinoma with metastases being around 17-20 months the decision for surgical intervention would not have been influenced by the subsequently correct initial diagnosis.
Conclusion
This case identifies the need for adequate specimen when performing a biopsy. The limits of fine needle biopsy must be recognised. Involvement of the cervico-thoracic junction should be recognised as an unstable area with early aggressive surgical intervention necessary to stabilise and prevent deformity and associated neural compression.
Finally, local metastatic tissue should always be sent for histological assessment.
References
1. Muresan MM, Olivier P, Lecle`re J, et al. Bone metastases from differentiated thyroid carcinoma. Endocrine-Related Cancer 2008;15:37-49. [ Links ]
2. Tee YY, Lowe AJ, Brand CA, et al. Fine-needle aspiration may miss a third of all malignancy in palpable thyroid nodules: a comprehensive literature review. Ann Surg 2007 Nov;246(5):714-20. [ Links ]
3. Cameron J. Thyroid cancer. In: Current Surgical Therapy, Ninth edition. Mosby Elsevier p614. [ Links ]
 Reprint requests:
Reprint requests:
Prof Robert Dunn
Tel: (021) 404-5387, Fax: (021) 404-5389
Email: info@spinesurgery.co.za
No commercial benefits were or will be derived from this paper.














