Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.9 n.1 Centurion Jan. 2010
CASE REPORT AND REVIEW OF THE LITERATURE
Bilateral sternoclavicular synovial cysts in juvenile idiopathic arthritis
F JosephI; S AhmadII; AD DehnaviIII; F IsmailIV
IMBChB, Department of Radiology, University of Pretoria, and Steve Biko Academic Hospital
IIMBBS, FCRad Diag(SA), Department of Radiology, University of Pretoria, and Steve Biko Academic Hospital
IIIMBChB, Department of Radiology, University of Pretoria, and Steve Biko Academic Hospital
IVMBChB, FCRad Diag(SA), MMed Rad, Department of Radiology, University of Pretoria, and Steve Biko Academic Hospital
ABSTRACT
Juvenile idiopathic arthritis (JIA) is an inflammatory disorder of connective tissue. Joint pain or tenderness, and swelling affecting one or more joints for at least six weeks, in patients under the age of 16 years, are diagnostic of JIA. Involvement of the juxta-articular structures is less common in JIA compared to adult rheumatoid arthritis. We present a case of JIA with bilateral sternoclavicular synovial cysts.
Introduction
Juvenile idiopathic arthritis (JIA) is an inflammatory disorder of the connective tissues. Joint pain or tenderness, and swelling affecting one or more joints for at least six weeks, in patients under the age of 16 years, are diagnostic of JIA.
There are three major onset subtypes:
1. Pauci-articular onset: four or fewer joints involved. This is the most common form, with 50% of cases presenting in this manner.
2. Poly-articular onset: five or more joints affected. This comprises 40% of the whole group.
3. Systemic onset: defined as arthritis associated with daily temperature spikes to 39.5 ºC for at least two weeks, with or without a typical rash. It comprises 10% of the whole group.
Synovium is the soft tissue lining the spaces of diarthrodial joints, tendon sheaths, and bursae. These spaces contain small amounts of fluid. There is increased vascular permeability with inflammatory oedema of the synovial tissue. Joint effusions arise as a consequence of overspill of the synovial oedema.
Case report
A 12-year-old boy, known to have had JIA from the age of three years, presented with two swellings on the anterior chest wall adjacent to the sternum, which had developed gradually over the previous few months.
His treatment for JIA over the years had not been optimal owing to multiple factors, and he had already developed severe deformities in the hands and fingers.
These swellings were investigated while the patient was hospitalised for a pathological left femur fracture caused by underlying osteopaenic bone.
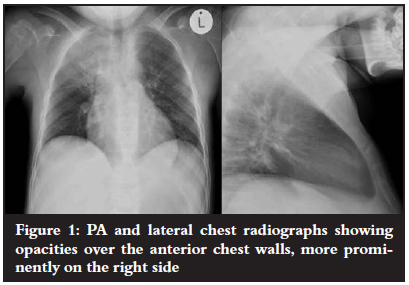
Plain radiographs demonstrated opacities over the anterior chest walls, more prominently on the right side (Figure 1).
CT demonstrated well-defined low density cystic masses adjacent to both sterno-clavicular joints, as well as irregularity of the joint margins (Figure 2).

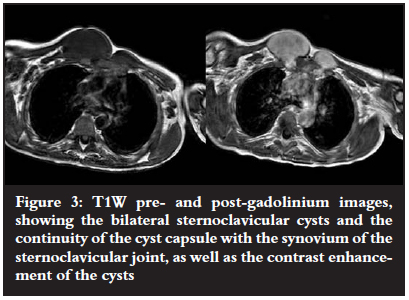
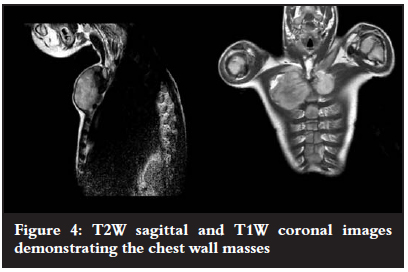
MRI demonstrated continuation of the cyst capsule with the joint synovium, as well as post-contrast enhancement of the cystic masses. This was diagnostic of synovial herniation cysts of the sterno-clavicular joints (Figures 3 and 4).
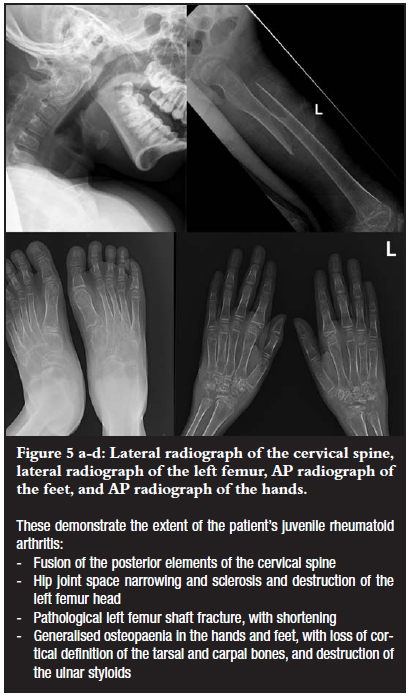
Underlying JIA changes were also evident in the cervical spine, hands and feet, and left hip joint (Figure 5 a-d).
Discussion
Synovial cysts are fluid-filled spaces lined by synovial membrane. They are a continuation or herniation of synovial tissue through the joint capsule.1
The first synovial cyst was reported by Adams in 1840, involving a knee joint cyst extending into the popliteal space.2 The English surgeon, W Baker, reported on synovial cysts in 1877, and hence, popliteal cysts are commonly called Baker cysts.3 Previous reports have shown synovial cysts involving the knees, shoulders, and wrists.4 Other locations include the elbows, ankles, hips and apophyseal joints of the spine.
Sternoclavicular and manubriosternal joints possess synovial and cartilage portions, and are more commonly affected in JIA than is appreciated.5
The synovium in rheumatoid arthritis (RA) is marked by expansion of the cell population of the intimal lining and massive infiltration of the sublining by T-cells, macrophages and B-cells.5
As synovial proliferation progresses, a pannus of granulation tissue forms, which encroaches on, undermines and destroys first articular cartilage, and then bone, thereby accounting for the radiological features of narrowing of joint spaces and para-articular erosions.
The volume of synovial fluid in affected joints is increased in JIA, with viscosity being decreased mainly because of reduced concentrations of hyaluronic acid.
Synovial fluid contains various inflammatory cells, including neutrophils, plasma cells, dendritic cells and a high proportion of T-cells expressing markers of activation. These cells are most likely to extravasate from inflamed synovial lining. Mediators of inflammation such as cytokines and cleavage products of the complement system are also abundant.5
It has been claimed that accumulation of synovial fluid increases intra-articular pressure, forcing the fluid out through valvular structures or through areas of least resistance created by the inflammatory process on the joint wall.
It has also been suggested that this is a possible protective mechanism for decompression of a diseased joint .4,6
Enlargement of a bursa communicating with the joint can also result in a synovial cyst.4
Any inflammatory, degenerative or traumatic condition that produces an effusion may contribute to the development of a synovial joint cyst.4 Hence, synovial cysts have also been described in association with other conditions including idiopathic arthritis, trauma, osteo-arthritis, gout, Sjögren's syndrome, tuberculosis, septic arthritis and systemic lupus erythematosis.7
The complications of synovial cysts include compression of adjacent neuro-vascular structures. Popliteal cysts may compromise arterial supply causing intermittent claudication. The cyst may mimic a tumour, adenopathy or haematoma.. The bladder may be compressed by a hip synovial cyst with resultant dysuria and frequency. The cyst may also be large enough to limit joint movement. In rare cases a cutaneous-joint fistula may occur.4,7
Conclusion
Synovial cysts arising from the sternoclavicular joints are a rare occurrence. In this case, in addition to the destruction of the left hip joint, the sternoclavicular joints also show rheumatic inflammatory involvement. Although synovial cysts may form from any inflamed joint, the most typical location is the popliteal fossa. However, atypical locations must also be borne in mind in the diagnostic work-up of peri-articular masses.
References
1. Davies AM, Grainger A. Techniques and imaging of soft tissues. In: Adam A, Dixon AK. Grainger and Allison's Diagnostic Radiology. 5th Edition. Elsevier Ltd 2008;969. [ Links ]
2. Adams M. Chronic rheumatic arthritis of the knee joint. Dublin J Med Sci 1840; 17:520-2. [ Links ]
3. Baker WM. Formation of synovial cysts in the leg in connection with disease of the knee joint. St Bartholomew's Hosp Rep 1877;13:245-61. [ Links ]
4. Burt TB, MacCarter DK, Gelman MI, et al. Clinical manifestations of synovial cysts. West J Med Aug 1980;133:99-104. [ Links ]
5. Hochberg MC, Silman AJ, Smolen JS, et al. Rheumatology. Volume 1. 3rd Ed. Mosby. 2003; 227-1:953-74. [ Links ]
6. Bamzai A, Krieger M, Kretschmer R.R. Synovial cysts in juvenile idiopathic arthritis. Annals of the Rheumatic Diseases 1978;37:101-3. [ Links ]
7. Fedullo LM, Akbar B, Moyer RA, et al. Giant synovial cysts. Skeletal Radiology 1984;12:90-6. [ Links ]
 Reprint requests:
Reprint requests:
Dr F Joseph
Department of Radiology, University of Pretoria Steve Biko Academic Hospital, Level 5, Bridge E Private Bag X 169 Pretoria, 0001
Tel: (012) 354-2406 Fax: (012) 354-2771
e-mail: febin_jsph@yahoo.co
No benefits of any form have been received from a commercial party related directly or indirectly to the subject of this article.














