Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.9 n.1 Centurion Jan. 2010
CASE REPORT AND REVIEW OF THE LITERATURE
Traumatic dislocation of the hip joint in children
GB Firth I; AD MazibukoII; M MunirIII
IMBBCh, FCS(SA)(Orth), MMed(Orth), Orthopaedic Consultant, Division of Orthopaedic Surgery, Chris Hani Baragwanath Hospital, University of the Witwatersrand, Johannesburg
IIBSc, MBBCh Orthopaedic, Registrar, Division of Orthopaedic Surgery, Chris Hani Baragwanath Hospital, University of the Witwatersrand, Johannesburg
IIIMD, Orthopaedic Consultant, Division of Orthopaedic Surgery, Chris Hani Baragwanath Hospital, University of the Witwatersrand, Johannesburg
ABSTRACT
Two cases of acute traumatic dislocation of the hip joint are reported. This is a rare injury and the literature on this subject is limited to either case reports or combined multicentre studies. The aim is to report on two cases of acute dislocation of the hip joint treated by us and to review the literature on this injury.
Introduction
Traumatic hip dislocation in children has a bimodal distribution. The first age group is between 2 and 5 years of age owing to joint laxity and soft cartilage. The second age group is between 11 and 15 years of age owing to athletic injuries and road traffic accidents. Posterior dislocations occur ten times more commonly than anterior dislocations. Sciatic and femoral nerve injuries and associated femoral shaft fractures must be ruled out. Fracture fragments are best seen on plain radiographs after reduction. Computer tomography (CT) or magnetic resonance imaging (MRI) scans are useful to rule out soft tissue interposition, intra-articular fragments or associated acetabular or femoral head fractures.1
Case 1
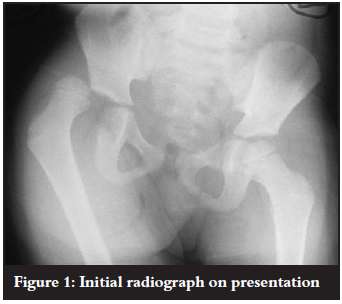
A 4-year-old boy was referred to our casualty department from a regional hospital with blunt trauma to the abdomen and a right hip dislocation following a pedestrian vehicle accident. The child was assessed and treated according to the Advanced Trauma Life Support protocol. Physical examination revealed an acute abdomen and a posterior dislocation of the right hip joint. The sciatic nerve was intact. The dislocation was confirmed by radiographs of the joint (Figure 1).
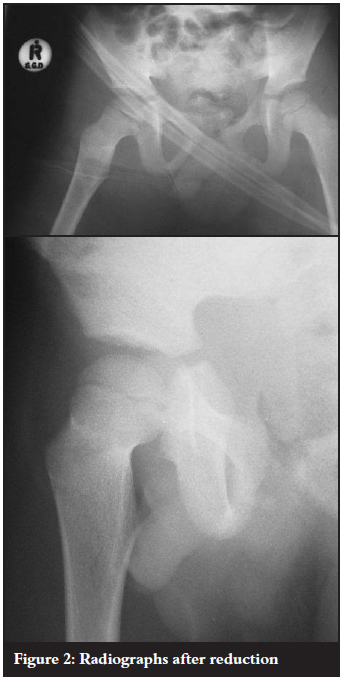
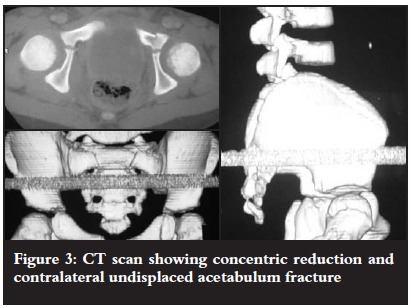
The hip joint was reduced under sedation and analgesia (Figure 2) and treated by skin traction for three weeks. CT scan was done to confirm a concentric reduction and to exclude intra-articular fractures or fragments. A contralateral undisplaced fracture of the acetabulum was discovered on CT scan and also treated with bed rest (Figure 3). The abdominal injury was managed surgically for a sealed perforation of the small bowel which required a relook laparotomy before full recovery.
After three weeks in skin traction, the hip joint was painless and reasonably mobile. The patient was allowed to weight bear.
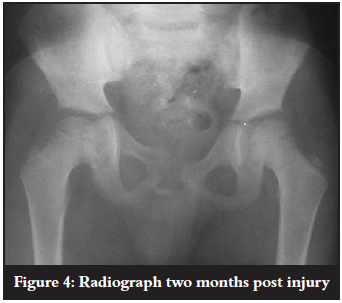
The patient was seen at our clinic two months after discharge. He was mobilising without support but had a mild antalgic gait. On examination the hip flexed to 140º, abducted to 70º, internally rotated to 40º and externally rotated to 50º. Anteroposterior (AP) pelvic radiograph showed concentric reduction with no complications (Figure 4).
Case 2
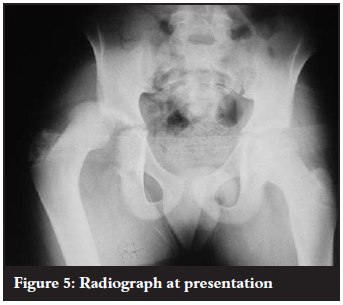
An 11-year-old boy was brought to our casualty department by paramedics following a pedestrian vehicle accident. The child was assessed and treated according to the Advanced Trauma Life Support protocol. He had an isolated injury to his right hip and abrasions on the lower back. The hip was flexed, internally rotated and adducted. The sciatic nerve was intact. Radiographs confirmed a posterior dislocation of the right hip joint (Figure 5).
The hip was reduced in theatre under general anaesthesia followed by skin traction for three weeks. Post-reduction radiographs demonstrated a reduced hip and no other fractures (Figure 6).
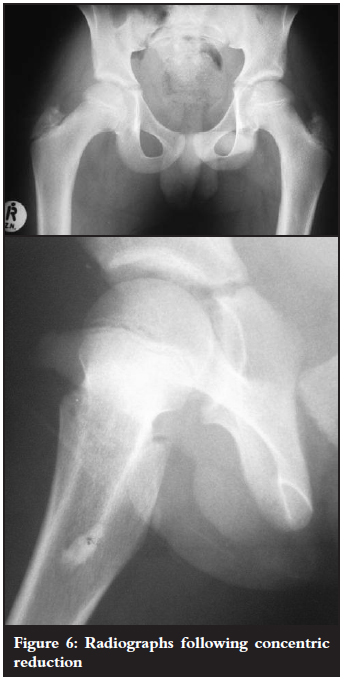
On discharge, physical examination revealed a painless full range of motion. He was discharged with a view to follow-up in our outpatient clinic but did not return for review.
Discussion
Our two patients fall into each of the described bimodal age group peaks and were both involved in road traffic accidents. Both of our cases were posterior dislocations, presenting with hip flexion, adduction and internal rotation.
In an attempt to classify these injuries, Thompson and Epstein reviewed the literature and included adults and children, resulting in their well-known classification. Only 17 of their cases (8%) were younger than 15 years of age, making the classification less applicable to children.2 Currently traumatic hip dislocations in children are classified descriptively, according to direction of dislocation and associated hip fractures.1
Treatment always involves emergency reduction to reduce the risk of complications. Closed reduction is usually performed. Open reduction is reserved for failed closed reduction, sciatic nerve compromise where incarceration in the joint is suspected or soft tissue interposition resulting in a non-concentric reduction. Open reduction may also be needed for the management of associated acetabulum or femoral head fractures. Concentric reduction on radiographs is critical. Post-reduction traction should be applied for a period of one to six weeks before weight bearing is allowed.3-5
Complications related to traumatic hip dislocations can be classified into early or late. Sciatic nerve injury may result in up to 13% of cases following traumatic posterior hip dislocation. Femoral nerve palsy must be excluded in anterior dislocations.1 Associated fractures have been shown to result in a poorer outcome. A Japanese review on the topic found that fewer than 5% of hip dislocations were associated with a femur fracture.6 Separation of the epiphysis may also result in avascular necrosis (AVN). A French study reviewed five cases of hip dislocation with associated separation of the capital epiphysis. All of these cases resulted in AVN following open reduction and screw fixation.7 The incidence of overall AVN ranges from 3% to 10% and is related to the severity of trauma and time to reduction. Chondrolysis is another potential but rare complication following hip dislocation.1 Degenerative joint disease is more prevalent if a concentric reduction is not achieved as shown by Glass et al.3 Soft tissue interposition with late arthrosis is a preventable problem, unlike many of the other complications, which are the result of the injury itself and out of the control of the treating surgeon.
A review of 47 traumatic hip dislocations was performed in Manchester, England. This review included all simple posterior dislocations with no associated fractures. The mean age was 12 years and patients were followed up for a mean of 28 months. Fourteen patients suffered complications (30%) which included AVN in four, degenerative joint changes in three, premature physeal closure in one and femoral head overgrowth in six. They demonstrated that early weight bearing, four weeks after reduction, was harmless.3
The largest published series is a multicentre study from The Scientific Research Committee of the Pennsylvania Orthopaedic Society. They reviewed 165 patients with dislocated hips. The majority (154) were treated with closed reduction. They found a 10% incidence of AVN which was associated with a delay in reduction (>24 hours) or severe trauma. Poor radiographic results at skeletal maturity were associated with fractures about the hip joint, delay in reduction or AVN. The period of traction and non-weight bearing following reduction varied from one to six weeks.4
Thirty-three children with traumatic hip dislocations were reviewed from Toronto, Canada. Nineteen were reviewed at a mean of 10 years post injury. Associated injuries were seen in ten patients but none had associated hip fractures. Nine patients developed complications. The commonest complication was soft tissue interposition in five cases, resulting in the need for posterior open reduction in four of them. One child developed AVN and one child had a recurrent hip dislocation. The clinical outcome was good in 84% of cases. Forty-seven per cent of the cases resulted in coxa magna but there was no correlation between clinical outcome and coxa magna.5
Our two cases emphasise the importance of early reduction and careful assessment with X-ray or CT scan after reduction to exclude fractures around the hip and to ensure a concentric reduction. Long-term follow-up is essential to exclude the complications described above.
Conclusions
Traumatic hip dislocations in children are rare. Associated injuries must be ruled out. Urgent concentric reduction must be achieved for optimal results. Plain radiographs remain an important tool especially in the public hospital sector, but CT (or MRI) scanning is probably always indicated. A period of three weeks with skin traction following reduction is supported in the literature, although this is controversial and not always practical or necessary. Associated fractures of the acetabulum and femoral head must be excluded and treated appropriately. Long-term follow-up is required to exclude the development of AVN, degenerative joint disease and chondrolysis.
References
1. Blasier RD, Hughes LO. Fractures and traumatic dislocations of the hip in children. Rockwood and Wilkin's Fractures in Children. Lippincott Williams and Wilkins; Sixth Edition; 2006:879-891. [ Links ]
2. Thompson VP, Epstein HC. Traumatic dislocation of the hip: A survey of 204 cases covering a period of 21 years. J Bone Joint Surg [Am] 1951;33-A:746-792. [ Links ]
3. Glass A, Powell HDW. Traumatic dislocation of the hip in children. An analysis of forty seven patients. J Bone Joint Surg [Br] 1961;43-B:29-37. [ Links ]
4. Traumatic dislocation of the hip joint in children: Final report. The Scientific Research Committee of the Pennsylvania Orthopaedic Society. J Bone Joint Surg [Am] 1968;50-A:79-88. [ Links ]
5. Offierski CM. Traumatic dislocation of the hip in children. J Bone Joint Surg [Br] 1981;63-B:194-197. [ Links ]
6. Yamamoto K, Ko M, Masaoka T, Shishido T, Imakiire A. Traumatic anterior dislocation of the hip associated with ipsilateral femoral shaft fracture in a child: A case report. Journal of Orthopaedic Surgery (Hong Kong) 2004;12(1):126-132. [ Links ]
7. Odent T, Glorion C, Pannier S, Bronfen C, Langlais J, Pouliquen JC. Traumatic dislocation of the hip with separation of the capital epiphysis. 5 Adolescent patients with 3-9 years of follow up. Acta Orthop Scand 2003;74(1):49-52. [ Links ]
 Reprint requests:
Reprint requests:
Dr GB Firth
Dept of Orthopaedics Wits Medical School
Tel: (011) 717-2538 Fax: (011) 717-2551
Email: greg.firth@gmail.com














