Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.9 n.1 Centurion Jan. 2010
CLINICAL ARTICLE
Arthroscopic treatment of calcifying tendonitis of the shoulder: deposit removal and intra-articular lavage
A RawootI; J de BeerII
IMBChB, Department of Orthopaedic Surgery, University of Stellenbosch
IIMBChB, MMed (Orth), Cape Shoulder Institute, Panorama, South Africa
ABSTRACT
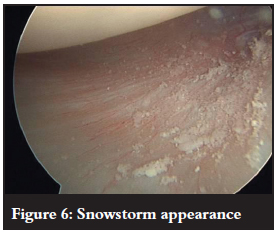
The optimal treatment of calcifying tendonitis is still controversial and several techniques exist. In this article we describe the arthroscopic operative technique for removal of calcific deposits as well intra-articular lavage. We hypothesised that the removal of these calcium particles from the intra-articular space, usually seen arthroscopically as a 'snowstorm' appearance, would result in a reduction in the incidence of post-procedure frozen shoulder. A retrospective analysis of 93 patients confirmed this.
Introduction
In patients with severe disabling symptoms that have persisted for more than 6 months and are resistant to conservative treatment, surgery is indicated.1 The first case of operative removal of calcific deposit was carried out by Harrington and Codman in 1902. Since then, favourable results have been reported by numerous authors with a subjective improvement of 82%, and 71% achieving excellent objective results following open excision of the calcium deposit via a deltoid split approach combined with an acromioplasty.2 Similarly, good results were reported by Rochwerger et al. who found that the Constant score improved from 52 to 89 after a mean follow-up of 23 months following open removal of calcium and acromioplasty.3 With advances in technology, these superior results have also been reproduced arthroscopically.4
Operative technique
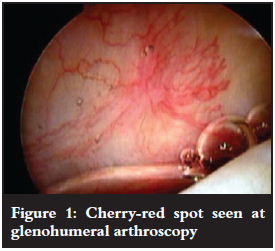
Shoulder arthroscopy is performed under combined nerve block and general anaesthesia with the patient positioned in the beach chair position. Standard posterior and lateral portholes are used. A diagnostic glenohumeral arthroscopy is performed first. Look for the cherry-red spot that may sometimes be seen on the undersurface of the cuff tendon5 (Figure 1). This may be used as a rough guide to the location of the deposit. A spinal needle is passed through the spot to confirm the presence of calcium (Figure 2). The needle is left in situ to mark the location of the calcium. Secondly, a diagnostic bursoscopy is performed. If a needle was placed through the cuff it can now be used to locate the position of the calcium in the rotator cuff tendon (Figure 3). Superficial lesions are easily detected. Deep lesions, however, may need a thorough bursectomy, and/or intra-operative radiological imaging (image intensifier, ultrasonography).


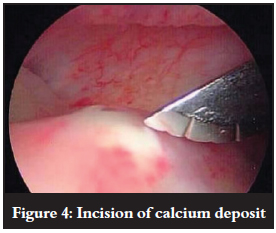
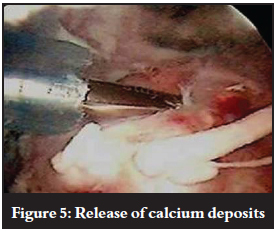
The deposit is incised along the length of the muscle fibres (Figure 4). Calcium can be either milked out or curetted out of the tendon (Figure 5). When the calcium is of a hard chalky texture, the arthroscopic rotating blade can be used to decompress the deposit, creating a typical snowstorm appearance. Some calcium particles may enter the glenohumeral joint space through perforations in the cuff tendon.
Intra-articular lavage: The calcium wash-out hypothesis
After calcium removal/excision from the tendon, the arthroscope is reintroduced into the glenohumeral space to detect any intra-articular 'leakage' of calcium crystals from the subacromial space which may have occurred during the removal from the tendon in the subacromial space. This is usually seen as having a 'snowstorm' appearance (Figure 6). Deposits may also be found in the axillary-pouch region. We hypothesised that removal of these calcium particles from the intra-articular space would result in a reduction in the incidence of post-procedure frozen shoulder.
Retrospective analysis
We reviewed the clinical notes of patients who had arthroscopic removal of calcium during the years of 2001 (prepost-procedure washout) and 2003 (post-procedure washout). There were 48 patients in 2001 and 45 in 2003. Pre-operative diagnosis of calcifying tendinitis was made from X-ray and ultrasonography, with size, site and appearance recorded. Surgery was carried out in the beach chair position under combined nerve block and general anaesthesia. In a number of cases the calcium deposit was marked by an overlying hyperaemic area of tendon. We described this as the 'cherry spot', as seen in Figures 1 and 2.
Methods used in cases where the deposit was difficult to locate included dropping the inflow pressure in the subacromial space, probing the tendon with a spinal needle, and marking the deposit using the image intensifier. Image intensifier was also used post procedure to assess if the calcium had been completely removed. The defects left in the tendon were evaluated according to size, and if necessary repaired with either side-to-side sutures or anchor fixation. Acromioplasty was performed depending on the assessment of the subacromial space and coraco-acromial ligament - it was rarely deemed to be necessary to add a decompression of the subacromial space.
The postoperative clinical notes were reviewed for documentation of postoperative frozen shoulder. For statistical analysis, the Chi-square test was used to determine if dependencies between variables existed. A 5% significance level (p<0.05) was used as a guideline for determining significant dependencies.
Results
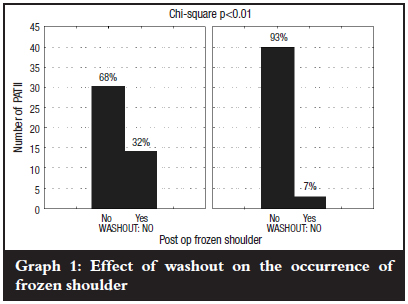
Graph 1 shows a significant dependence (p<0.01) between washout and the occurrence of frozen shoulder. For the patients where no washout was done, 32% developed postoperative frozen shoulder, whereas in the patients who had washout, only 7% developed postoperative frozen shoulder. The diagnosis of a frozen shoulder is a clinical diagnosis. There were no significant differences between the two groups with regard to age, sex, arm dominance, and prevalence of diabetes.
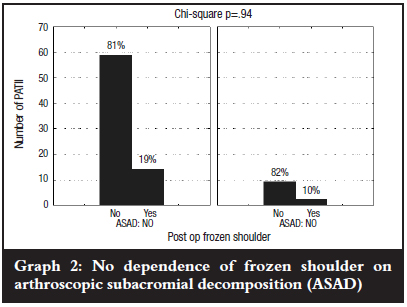
The incidence of frozen shoulder was not affected by sex, diabetes, acromioplasty, size of defect, or whether the defect required repair post calcium removal. We found that there was a significant increase (p<0.01) in the incidence of frozen shoulder in those requiring intra-operative imaging to locate the deposit (Graphs 2 and 3). We postulated that in cases requiring imaging for location, the calcium may lie deeper within the tendon and therefore be more likely to be dispersed into the joint during removal.

Conclusion
Arthroscopic removal of calcium deposits in the rotator cuff is a well-recognised treatment method for calcifying tendonitis. We found, as has been described previously in a number of studies, that a significant number of patients developed frozen shoulder postoperatively.6,7,8 We attribute this to the calcium being inadvertently distributed into the glenohumeral joint during subacromial calcium deposit location with needling and subsequent tendon incision and curettage. On reintroducing the arthroscope into the joint post procedure, we have captured the 'snowstorm' appearance of the intra-articular calcium, with crystals lying in the axillary pouch .The importance of this iatrogenic effect is supported by the significant decrease in frozen shoulder since the change in our practice to include joint washout.
References
1. Rotini R, et al. Algorithm for the treatment of calcific tendinitis in the rotator cuff: indications for arthroscopy and results in our experience. Chir Organi Mov 2005;90(2):105-12. [ Links ]
2. Gazielly DF, Bruyere G, Gleyze PTT. Open acromioplasty with excision of calcium deposits and tendon suture. The cuff. Paris: Elsevier;1997. pp. 172-5. [ Links ]
3. Rochwerger A, et al. Surgical management of calcific tendinitis of the shoulder: an analysis of 26 cases. Clin Rheumatol 1999;18(4):313-6. [ Links ]
4. Costouros JG, et al. Arthroscopic management of calcific tendonitis of the shoulder. Presented at the American Academy of Orthopaedic Surgeons annual meeting, 2006. p. 695. [ Links ]
5. Lam F, Bhatia DN, De Beer J et al, Modern management of calcifying tendonitis of the shoulder. Current Orthopaedics, 2006. [ Links ]
6. Kempf JF, Bonnomet F, Nerisson D et al. Arthroscopic isolated excision of the rotator cuff calcium deposit. In: Gazielly DF, Gleyze P, Thomas T, eds. The Cuff. Paris: Elsevier; 1997; 164-8. [ Links ]
7. Uthoff HK. Anatomopathology of calcifying tendinitis of the cuff. In: Gazielly DF, Gleyze P, Thomas T, eds. The Cuff. Paris: Elsevier; 1997; 144-7. [ Links ]
8. Molé D, Gonzalvez M, Roche O, Scarlat M. Introduction to calcifying tendinitis, eds. The Cuff. Paris: Elsevier; 1997; 141-3. [ Links ]
 Reprint requests:
Reprint requests:
Dr A Rawoot
PO Box 19063 7505 Tygerberg South Africa
E-mail: a_arawoot@yahoo.com
No benefits of any form have been received from a commercial party related directly or indirectly to the subject of this article.














