Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SA Orthopaedic Journal
On-line version ISSN 2309-8309
Print version ISSN 1681-150X
SA orthop. j. vol.9 n.1 Centurion Jan. 2010
CLINICAL ARTICLE
MMTM AllyI; CC VisserII
IMBChB, FCP Rheumatologist, Department of Internal Medicine, Head: Division of Rheumatology, University of Pretoria and Steve Biko Academic Hospital
IIMBChB, Rheumatologist, Department of Orthopaedics, Pain Clinic, Steve Biko Academic Hospital
ABSTRACT
RA is a chronic inflammatory disease resulting in severe morbidity and premature mortality. This review explores in a series of two articles, the current developments in the pathogenesis, diagnosis, monitoring and management of patients with RA. The diagnosis of early as well as established disease is discussed, including the diagnostic criteria. Particular emphasis is placed on the pitfalls and benefits of early diagnosis and early intervention.
Prevention and limitation of comorbidity from the disease is highly important. This can be achieved following a paradigm shift in RA management. The emphasis is now on early introduction of disease-modifying anti-rheumatic drugs, including timely use of highly efficacious pharmacological innovations. Side effects, including peri-operative implications of pharmacological therapy, are discussed.
Current therapeutic strategy to manage this disease should also be applied in resource-poor settings and developing countries. These therapies are cost effective if used early and judiciously, giving hope to many patients with RA.
Part I Review of the pathogenesis, clinical features, utility of special investigations and measures of disease activity in patients with rheumatoid arthritis
Introduction
Rheumatoid arthritis (RA) is the commonest type of inflammatory arthritis and often has a progressive and destructive course. RA not only significantly affects function and quality of life, but is also associated with significant comorbidity and premature death. With the revolutionary advances in the development of new and more effective therapies, it is now possible to dramatically alter the course of the disease, especially when treatment is started early. This review focuses on the diagnosis of early RA, assessment of disease activity, and principles of management.
Rheumatoid arthritis in the developing world
A major problem in developing countries is a significant delay in the diagnosis of RA and the initiation of appropriate treatment. This delay leads to a poor outcome and the loss of working ability. For instance, in manual labourers, most patients are unable to work within two years of disease onset with devastating social consequences.1,2 There is limited data available on the epidemiology of RA in South Africa. A recent review of data from developing countries suggests a prevalence of approximately 1%, which is similar to that seen in developed countries.1,3
RA is also associated with an increased risk of infection, related to both the disease and to immunosuppressive therapy. Of particular concern in developing countries are viral hepatitis, HIV and tuberculosis.
Pathogenesis of rheumatoid arthritis
In recent years tremendous advances have been made in the understanding of human immune and inflammatory responses in the pathogenesis of RA. However, despite concerted research efforts, the triggering factor for RA still remains an elusive mystery.
Genetic factors certainly have a role to play in the pathogenesis of RA. The 'shared epitope' is a common sequence of amino acids on the HLA-DR4 antigen seen in the vast majority of patients with RA.4 Certain antigen subtypes have been associated with more aggressive disease while other subtypes confer a protective effect.4-6
The innate immune system, responsible for the initial non-specific response to foreign antigens, seems to be involved early in RA.7,8 The antigens which trigger the innate immune system response have not yet been identified, but probably resemble or mimic synovial tissue antigens. Antigen stimulation leads to a cascade of events in a genetically predisposed individual in the presence of certain hormonal and environmental factors. Thereafter, the adaptive immune system (antigen-specific immune responses) launches a sustained and specific attack on synovial tissue, which is now perceived as 'foreign'.
The immune response leads to the characteristic histological features of RA. This is characterised by synovial proliferation, new blood vessel formation and infiltration of the synovium by T-cells, B-cells, macrophages and fibroblasts. This process is eventually followed by local joint destruction.9
The inflammatory infiltrate secretes numerous cytokines, of which TNF-α, IL-1 and IL-6 are the pivotal cytokines in the pathogenesis of RA. Cytokines are glycoproteins that act via cell surface receptors to regulate cellular function by either promotion or suppression of inflammation. This balance between pro-inflammatory versus anti-inflammatory cytokines is disturbed in RA. Cytokines are also responsible for local and systemic effects seen in RA. TNF-α plays an important role in synovial proliferation and activation of osteoclasts resulting in erosive joint destruction and functional impairment.9 The systemic effects include not only extra-aerticular disease but accelerated atheroscelerosis and consequent increased cardiovascular morbidity and mortality.
Cytokines such as TNF-α, IL-1 and IL-6 have become important targets in the management of RA. Other new treatment modalities target B-cell depletion and inhibition of T-cell stimulation.10,11 There may possibly be a role for bisphosphonates to prevent erosive disease by inhibiting osteoclastic activity.10
Clinical diagnosis
Early rheumatoid arthritis
Early diagnosis and treatment of RA is of paramount importance. The window of opportunity to halt or retard the inflammatory process is the first two to three years. Studies have shown that the rate of radiographic progression is the fastest during this window period, with early intervention significantly altering the course of the disease and the degree of joint destruction in later years.12-14 In clinical trials, early RA is often defined as a disease duration of less than two years, but more recent studies have been using one year or even six months as a cut-off point.
Presenting symptoms are usually insidious, with arthritis developing over weeks to months, although an acute onset is seen in up to 15% of patients. Non-specific constitutional symptoms such as fatigue and malaise rather than arthritis, predominate in some patients. Less commonly, extra-articular manifestations such as scleritis, sicca syndrome (dry eyes and dry mouth) and rheumatoid nodules are found, reflecting more aggressive disease.
The presence of four or more of the American College of Rheumatology (ACR) classification criteria is often used to diagnose RA.15 These criteria include clinical, serological and radiological features:
• Morning stiffness for > 1 hour
• Arthritis of > 3 joint areas
• Arthritis of wrist/metacarpal phalangeal/proximal interphalangeal joints
• Symmetric arthritis
• Rheumatoid nodules
• Serum rheumatoid factor (IgM)
• Radiographic changes: peri-articular osteopaenia, marginal erosions
New criteria currently under review
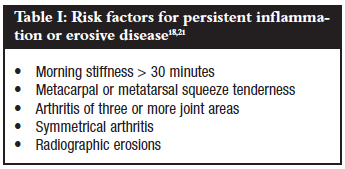
Newer diagnostic methods such as magnetic resonance imaging (MRI), ultrasound and the cyclic citrullinated peptide (CCP) antibody tests have become available increasing the sensitivity and specificity of diagnosing RA, especially in early disease.15-20 It is important to look for features that would suggest persistent inflammation or erosive disease (Table I).
Synovitis may be subtle, with only mild joint swelling, a soft 'doughy' feel and tenderness along the joint line. It commonly involves the wrist, metacarpophalangeal (MCP), proximal interphalangeal (PIP), knee and metatarsophalangeal (MTP) joints. Clinicians should be aware that initially the joint involvement can be asymmetrical.
Other possible differentials in the diagnosis of patients with early arthritis need to be considered. Features such as Raynaud's phenomenon, malar rash, photosensitivity, oral ulceration, alopecia and dysphagia may suggest an underlying connective tissue disorder.
Established rheumatoid arthritis
With progressive disease, typical articular and extra-articular manifestations develop.
Articular manifestations
The articular deformities result as a consequence of both the synovitis, as well as bony, ligament and tendon pathology. These deformities are especially distinctive in the hands and feet.
Upper limb
• The hand: Involvement predominantly involves the MCP and PIP joints, resulting in the classical rheumatoid swan-neck deformities, boutonniere deformities or Z-deformities of the thumb. Palmar subluxation and ulnar deviation of the fingers occur at the MCP joints. If the finger deformities are reducible, the possibility of systemic lupus erythematosus should be considered.
Severe erosive disease and resorptive changes of the phalanges result in the telescoping digits seen in arthritis mutilans. With more aggressive treatments, arthritis mutilans is now seen far less frequently.
Tendon ruptures may be caused by pressure or friction over bony prominences, or by weakening of the tendon due to tenosynovitis. Triggering of fingers may be related to either tenosynovial fibrinous thickening or to nodule formation within the tendon.
Radial deviation and palmar subluxation are characteristic features in the wrist. The presence of a ballottable ulnar styloid prominence is known as the 'piano key sign', an important risk factor for extensor tendon rupture.15• Elbow: Involvement results in limitation of extension, pronation and supination. Olecranon bursitis may occur, but this can also occur with gout, trauma or infections.
• Shoulder and acromioclavicular joint: These joints are commonly involved in RA. Bursal involvement may cause impingement of the rotator cuff and could contribute to the typical resorption of the distal clavicle. Rotator cuff tendinitis or tears can eventually lead to rotator cuff arthropathy.
Lower limb
• Hip: This joint is less frequently involved, and is classically associated with axial migration of the femoral head. This can be complicated by protrusio acetabuli.
• Knees: The knees are commonly involved in RA. Progressive disease often results in fixed flexion deformities, varus or valgus angulation. Synovial or Baker's cysts may also develop. If these cysts rupture, they can cause severe pain and swelling of the calf and resemble a deep venous thrombosis.
• Ankle and foot: Involvement of the ankle is less common than hindfoot and midfoot arthritis, which often leads to pronation and valgus deformity of the hindfoot.22 Classical forefoot changes include hallux valgus, lateral deviation and upward subluxation of the second to fifth toes. MTP subluxation leads to painful pressure areas over the metatarsal heads and may be complicated by protrusion of the metatarsal heads through the plantar skin.
Other
• Cervical spine: Involvement is often asymptomatic and should be suspected in all patients with erosive disease in the hands, as this correlates with cervical involvement. Rarely patients may present with features of vertebro-basilar insufficiency related to increased tortuosity of the vertebral arteries. Tilting of the head to one side may occur and is a result of collapse of the lateral mass of C1. Basilar invagination and C1-C2 subluxation are serious complications that could result in severe cord impingement or sudden death.23
• Cricoarytenoid joint: Involvement is seen in 30% of patients and usually presents with hoarseness or local discomfort. Very rarely it may be associated with respiratory symptoms.
• Temporomandibular joint: Radiological involvement is seen in almost 80% of patients with RA and is clinically involved in approximately 50% of patients.
• Ossicles in the ear: Erosive disease and shortening of the ossicles may result in conductive hearing loss
• Sternoclavicular and manubriosternal joints: These joints are commonly involved but often asymptomatic.
Extra-articular manifestations
Extra-articular manifestations are associated with a poorer prognosis. Nodules typically occur over the extensor areas of the forearm but could also be seen in other areas such as the ischial and sacral prominences, finger joints, Achilles tendon and the occipital region. Nodules may also occur in the larynx, heart, lungs and sclera. Interestingly, although methotrexate is used to treat RA, it may cause rapid development and growth of nodules that affect the digits in particular.24,25
Ocular involvement occurs mostly secondary to Sjögren's syndrome and presents with dry eyes and mouth. Episcleritis is usually noninflammatory; it manifests as patchy scleromalacia, with scleromalacia perforans a rare complication.
Pleural effusion is the most common lung manifestation, with an exudative effusion typically low in glucose. Interstitial lung disease is seen in a third of patients but may also be a complication of therapy. In patients with occupational exposure to coal mining, development of pulmonary nodulosis is known as 'Caplan's syndrome'.
Anaemia related to chronic disease is common in patients with active disease. Iron deficiency anaemia may result from gastrointestinal bleeding related to nonsteroidal anti-inflammatory drugs (NSAIDs). The presence of leg ulcers, splenomegaly or leucopaenia may signify Felty's syndrome. This is seen in about 1% of patients and is characterised by severe articular and extra-articular involvement.
Structural cardiac disease is not common. However, RA is associated with a significantly increased risk for cardiovascular morbidity and mortality, similar to that seen in type 2 diabetes. Inflammation is now considered an important independent risk factor for atherosclerosis, with studies in RA showing a significant relationship between CRP and cardiovascular disease.26-29 This risk for accelerated atherosclerosis emphasises the need to manage the whole patient, to look for traditional risk factors of cardiovascular disease, and also to control the inflammatory process.
RA patients are at increased risk of malignancy, with a two- to three-fold increase in susceptibility to develop lymphomas.30 With the advent of newer therapies, particularly TNF-α blockers, theoretical concerns were raised that this risk would increase but these concerns have not been validated to date. Atypical presentations or onset in the elderly could be a paraneoplastic manifestation of an underlying malignancy.31,32
Special investigations
General
Acute-phase markers like the erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) may be normal in early RA. If the CRP is elevated together with anaemia this usually signifies a poorer prognosis.
Antibodies
Rheumatoid factor (RF)
As RA is an autoimmune disease, the presence of circulating antibodies may assist with the diagnosis. RF is an antibody against the Fc component of immunoglobulins. Its presence is associated with a poorer prognosis.16,17 RF is not essential for the diagnosis of RA, as around 40% of patients test negative in early disease. About 20% of patients remain negative throughout the course of their disease.
There are numerous chronic infective and inflammatory causes of false positive results. There is no need to repeat the test once positive, as it has no role in the monitoring of disease activity.
Cyclic Citrullinated Peptide Antibodies (CCP)
The recent identification of an antibody to a chemically altered synovial protein (a process called citrullination) has increased the sensitivity and specificity of diagnosing RA, especially if used in combination with the rheumatoid factor. This antibody has been implicated in the possible aetiology of RA, especially in smokers. Smoking in patients with the HLA-DR4 antigen seems to act as an important risk factor for citrullination of synovial protein, thus resulting in anti-CCP antibodies. These antibodies have been found in patients preceding the onset of RA and may have a predictive role. As with RF, the presence of CCP antibodies has been shown to be associated with a poorer prognosis.16,17
The presence of both RF and CCP have a specificity of >98% for the diagnosis of RA.
Imaging
X-rays
Plain X-rays are usually normal in early disease, but can be useful if characteristic marginal erosions are seen, sometimes as early as three months after the onset of disease (only 10% of patients). Most patients (70%) develop erosive disease within three years, most commonly in the feet. Positive RF and baseline radiographic score are the best predictors of radiographic progression. Juxta-articular osteopaenia, often regarded as an early feature of RA, has been shown to be unreliable in longitudinal studies involving multiple centres. Numerous different scoring systems exist, with the Larson and Sharp scores used in most clinical trials.33
Musculoskeletal ultrasound
Musculoskeletal ultrasound allows for real-time evaluation of joints and has become a useful extension of the clinical examination. Synovitis and effusions are readily seen and Doppler ultrasound measurement of vascular flow can be used to assess severity of the inflammation and to monitor treatment response.19 Erosions can be detected earlier on ultrasound than on plain X-rays but this modality is very operator-dependent.
Magnetic resonance imaging
Magnetic resonance imaging (MRI) is more expensive and not as readily available as ultrasound. Extremity MRI units will make musculoskeletal MRI more accessible in future. MRI provides an objective and sensitive tool to detect synovitis, effusions, erosions and bone marrow inflammatory changes consistent with RA.19,20
Measures of disease activity and damage
Various clinical, serological and imaging measures are used to get a full picture of RA disease activity. These are combined in various validated composite scores used in clinical trials to monitor response to treatment. In daily clinical practice the Health Assessment Questionnaire and Simplified Disease Activity Index are often used.34
Health Assessment Questionnaire (HAQ)35
This validated score of the patient's self-reported ability to perform a range of activities of daily living is scored on a scale of 0 to 3:
• 0 = no difficulty
• 1 = some difficulty
• 2 = much difficulty
• 3 = unable to do
The questionnaire is divided into eight categories. Only the maximum score in each category is used, with the final score being the average of these scores. The HAQ has been shown to predict function, work ability, cost of treatment and likelihood of joint replacement surgery.35
The final functional limitation represented in the HAQ is due to a combination of inflammatory disease activity and irreversible joint damage. Improvements in the HAQ are predominantly due to a decrease in inflammatory activity. The irreversible component correlates with disease duration and radiographic changes.32
Simplified Disease Activity Index (SDAI)
This is a composite score calculated by the summation of the number of swollen and tender joints (assessing shoulders, elbows, wrists, MCP joints, PIP joints and knees), the patient and physician assessments of disease activity (on a visual analogue scale of 10 cm) and the CRP (in mg/dl).36 The SDAI has been shown to correlate with disease activity, with the following cut-offs:
• < 3.3 = remission
• < 11 = mild disease activity
• < 26 = moderate disease activity
With the availability of biologic therapies it has become important to include these measures in routine clinical practice. This helps to identify the subset of patients who may benefit from more aggressive treatment, but also ensures that the expensive biologic therapies are not inappropriately used.
References
1. Mody GM, Cardiel MH. Challenges in the management of rheumatoid arthritis in developing countries. Best Practice & Research Clin Rheumatol 2008;22(4):621-41. [ Links ]
2. Benitha R, Tikly M. Functional disability and health-related quality of life in South Africans with rheumatoid arthritis and systemic lupus erythematosus. Clin Rheumatol 2007;26:24-9. [ Links ]
3. Adebajo AO, Reid DM. The pattern of rheumatoid arthritis in West Africa and comparison with a cohort of British patients. Q J Med 1991;80(292):633-40. [ Links ]
4. Ling S, Pi X, Holoshitz J. The rheumatoid arthritis shared epitope triggers innate immune signaling via cell surface calreticulun. The Journal of Immunology 2007;179:6359-67. [ Links ]
5. Gonzalez-Gay MA, Garcia-Porrua C, Hajeer AH. Influence of human leukocyte antigen-DRB1 on the susceptibility and severity of rheumatoid arthritis. Semin Arthritis Rheum June 2002;31(6):355-60. [ Links ]
6. Feitsma AL, AHM van der Helm-van Mil, Huizinga TWJ, De Vries RRP, Toes EM. Protection against rheumatoid arthritis by HLA: nature and nurture. Ann Rheum Dis 2008;67:iii61-iii63. [ Links ]
7. Ling S, Pi X, Holoshitz J. The rheumatoid arthritis shared epitope triggers innate immune signaling via cell surface calreticulun. The Journal of Immunology 2007;179:6359-67. [ Links ]
8. Marshak-Rothstein A, Busconi L, Rifkin IR, Viglianti GA. The stimulation of Toll-like receptors by nuclear antigens: a link between apoptosis and autoimmunity. Rheum Dis Clin N Am 2004;30:599-74. [ Links ]
9. Lorenzo M. Rheumatoid arthritis. Foot Ankle Clin N Am 2007;12:525-37. [ Links ]
10. Smolen JS, Gunter S. Therapeutic strategies for rheumatoid arthritis. Nature Reviews Drug Discovery 2. 2003;473-88. [ Links ]
11. Keystone EC. B-cells in rheumatoid arthritis: from hypothesis to the clinic. Rheumatology 2005;44 (Suppl 2):ii8-ii12. [ Links ]
12. Eberhardt KB, Rydgren LC, Pettersson H, Wollheim FA. Early rheumatoid arthritis - onset, course, and outcome over 2 years. Rheumatol Int 1990;10(4):135-42. [ Links ]
13. O'Dell JR. Treating rheumatoid arthritis early: a window of opportunity? Arthritis Rheum 2002;46(2):283-5. [ Links ]
14. Breedveld, Kalden JR. Appropriate and effective management of rheumatoid arthritis. Ann Rheum Dis 2004;63:627-33. [ Links ]
15. Khurana R, Berney SM. Clinical aspects of rheumatoid arthritis. Pathophysiology 2005;12:153-65. [ Links ]
16. Van Paassen P, Damoiseaux J, Cohen Tervaert JW. Laboratory assessment in musculoskeletal disorders. Best Practice & Research Clinical Rheumatology 2003;17(3):475-94. [ Links ]
17. Lane SK, Gravel JW, jr. Clinical utility of common serum rheumatologic tests. Am Fam Physician 2002;65:1073-80. [ Links ]
18. Visser H, le Cessie S, Vos K, Breedveld FC, Hazes JMW. How to diagnose rheumatoid arthritis early. Arthritis & Rheumatism Feb 2002;46(2):357-65. [ Links ]
19. Tehranzadeh J, Ashikyan O, Dascalos J. Advanced imaging of early rheumatoid arthritis. Radiol Clin N Am 2004;42:89-107. [ Links ]
20. Ostergaard M, Ejbjerg B, Szkudlarek M. Imaging in early rheumatoid arthritis: roles of magnetic resonance imaging, ultrasonography, conventional radiography and computed tomography. Best Practice & Research Clinical Rheumatology 2005;19(1):91-116. [ Links ]
21. Raissouni N, Gossec L, Ayral X, Dougados M. New concepts in the diagnosis and treatment of recent-onset polyarthritis. Joint Bone Spine 2005;72:119-23. [ Links ]
22. Bare AA, Haddad SL. Tenosynovitis of the posterior tibial tendon. Foot and Ankle Clinics March 2001;1:37-47. [ Links ]
23. Narváez JA, Naráez J, Serrallonga M, et al. Cervical spine involvement in rheumatoid arthritis: correlation between neurological manifestations and magnetic resonance imaging findings. Rheumatol 2008;47:1814-9. [ Links ]
24. Maldonado I, Eid H, Rodriguez GR, et al. Rheumatoid nodulosis. Is it a different subset of rheumatoid arthritis? J Clin Rheumatol 2003;9:296-305. [ Links ]
25. Evangelisto A. A diagnostic dilemma. J Clin Rheumatol 2003;9:287-90. [ Links ]
26. Abou-Raya A, Abou-Raya S. Inflammation: A pivotal link between autoimmune diseases and atherosclerosis. Autoimmunity Reviews 2007;5:331-7. [ Links ]
27. Sitia S, Atzeni F, Sarzi-Puttini P, et al. Cardiovascular involvement in systemic autoimmune diseases. Autoimmunity Reviews 2009;8:281-6. [ Links ]
28. Galarraga B, Khan F, Kumar P, et al. C-reactive protein: the underlying cause of microvascular dysfunction in rheumatoid arthritis. Rheumatol 2008;47:1780-4. [ Links ]
29. Poole CD, Conway P, Currie CJ. An evaluation of the association between C-reactive protein, the change in C-reactive protein over one year, and all-cause mortality in chronic immune-mediated inflammatory disease managed in UK general practice. Rheumatol 2009;48:78-82. [ Links ]
30. Chakravarty EF, Genovese MC. Associations between rheumatoid arthritis and malignancy. Rheum Dis Clin N Am 2004;30:271-84. [ Links ]
31. Naschitz JE. Rheumatic syndromes: clues to occult neoplasia. Curr Opin Rheumatol 2001;13:62-6. [ Links ]
32. Abu-Shakra M, Buskila D, Ebrenfeld M. et al. Paraneoplastic Rheumatologic Syndromes. Ann Rheum Dis 2001;60(5):433-41. [ Links ]
33. Boonen A, van der Heijde D. Conventional X-ray in early arthritis. Rheum Dis Clin N Am 2005;31:681-98. [ Links ]
34. Aletaha D, Smolen J, Ward MM. Measuring function in rheumatoid arthritis: Identifying reversible and irreversible components. Arthritis Rheum 2006;54:2784. [ Links ]
35. Alethah D, Smolen JS. The definition and measurement of disease modification in inflammatory rheumatic diseases. Rheum Dis Clin N Am 2006;32:9-44. [ Links ]
36. Guillemin F. Assessment of disease activity. Best Practice & Research Clinical Rheumatol 2003;17(3):415-26. [ Links ]
 Reprint requests:
Reprint requests:
Prof MMTM Ally
University of Pretoria & Pretoria Academic Hospital Faculty of Health Sciences School of Medicine Department of Internal Medicine Head: Division of Rheumatology
PO Box 667 Pretoria, South Africa 0001
Tel: 27 (0)12 354-2112 Fax: 27 (0)12 354-4168
Email: tar@up.ac.za
No benefits of any form have been received from a commercial party related directly or indirectly to the subject of this article. The content of this article is the sole work of the authors.















