Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
Southern African Journal of Critical Care (Online)
versión On-line ISSN 2078-676X
versión impresa ISSN 1562-8264
South. Afr. j. crit. care (Online) vol.39 no.2 Pretoria jul. 2023
http://dx.doi.org/10.7196/SAJCC.2023.v39i2.867
RESEARCH
An analysis of referrals to a level 3 intensive care unit in a resource-limited setting in South Africa
U V JaganathI; K de VasconcellosII, IV; D L SkinnerIII, IV; P D GopalanV, VI
IMB ChB, DA (SA), FCA (SA); Discipline of Anaesthesiology, Inkosi Albert Luthuli Central Hospital, University of KwaZulu-Natal, Durban, South Africa
IIFCS (SA); King Edward VIII Hospital and Department of Anaesthesiology and Critical Care, University of KwaZulu-Natal, Durban, South Africa
IIIFCS (SA); Private practice, Busamed Hillcrest Private Hospital, Durban, South Africa
IVFCS (SA); Discipline of Anaesthesiology and Critical Care, School of Clinical Medicine, College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
VFCA (SA), PhD; King Edward VIII Hospital and Department of Anaesthesiology and Critical Care, University of KwaZulu-Natal, Durban, South Africa
VIFCA (SA), PhD; Discipline of Anaesthesiology and Critical Care, School of Clinical Medicine, College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND: With a shortage of intensive care unit (ICU) beds and rising healthcare costs in resource-limited settings, clinicians need to appropriately triage admissions into ICU to avoid wasteful expenditure and unnecessary bed utilisation
OBJECTIVE: To assess the nature, appropriateness and outcome of referrals to a tertiary centre ICU
METHODS: A retrospective review of ICU consults from September 2016 to February 2017 at King Edward VIII Hospital was performed. The study was approved by the University of KwaZulu-Natal Biomedical Research Ethics Committee (BE291/17). Data pertaining to patients' demographics, referring doctor, diagnosis, comorbidities as well as biochemical and haemodynamic parameters were extracted. This information was then cross-referenced to the outcome of the ICU consultation. Data were descriptively analysed
RESULTS: Five hundred consultations were reviewed over a 6-month period; 52.2% of patients were male and the mean age was 44 years. Junior medical officers referred 164 (32.8%) of the consultations. Although specialist supervision was available in 459 cases, it was only utilised in 339 (73.9%) of these cases. Most referrals were from tertiary (46.8%) or regional (30.4%) hospitals; however, direct referrals from district hospitals and clinics accounted for 20.4% and 1.4% of consultations, respectively. The appropriate referral pathway was not followed in 81 (16.2%) consultations. Forty-five percent of consults were accepted; however, 9.3% of these patients died before arrival in ICU. A total of 151 (30.2%) patients were refused ICU admission, with the majority (57%) of these owing to futility. Patients were unstable at the time of consult in 53.2% of referrals and 34.4% of consults had missing data
CONCLUSION: Critically ill patients are often referred by junior doctors without senior consultation, and directly from low-level healthcare facilities. A large proportion of ICU referrals are deemed futile and, of the patients accepted for admission, almost 1 in 10 dies prior to ICU admission. More emphasis needs to be placed on the training of doctors to appropriately triage and manage critically ill patients and ensure appropriate ICU referral and optimising of patient outcomes
Contribution of the study
There is a paucity of information related to ICU referrals in South Africa. The nature, appropriateness and outcomes of referrals to a tertiary ICU is discussed in this study.
Patients who are critically ill require urgent care in intensive care units (ICUs) to reduce the risk of mortality. In a resource-limited setting with inadequate ICU beds, trained staff and healthcare resources, appropriate triage and immediate admission is challenging. In South Africa (SA), public healthcare spending is currently approximately 13.8% of total government expenditure but, when adjusted for inflation, allocations and spending on the health budget are expected to decrease in coming years.[1] As healthcare costs rise in a low- middle-income country such as SA, there has been an inclination to cut back on expenditure and redirect resources towards preventive and primary healthcare that has resulted in a lack of human and financial resources in critical care infrastructure.[2,3] The demand for critical care continues to increase owing to factors associated with an ageing population, combined with the high burden of human immunodeficiency virus (HIV) disease and trauma.[4] Unfortunately, the demand for critical care outweighs the available resources. A study by Bhagwanjee and Scribante revealed that in SA only 23% of public hospitals have an ICU, with KwaZulu-Natal (KZN) having approximately 100 or less ICU beds.[5] The availability of ICU beds largely influences admission into ICU as, with a bed shortage, clinicians need to appropriately triage patient admissions into such units to avoid wasteful expenditure and unnecessary bed utilisation.[6]
In SA, there are limited data that evaluate the demand placed on critical care units. In addition, data are scarce regarding the characteristics and adequacy of patient referrals to ICUs.[7,8] Therefore, the objective of the present study was to assess the nature, appropriateness and outcome of referrals to a tertiary centre ICU. It is hoped that these data will highlight possible interventions to improve critical care services in a resource-limited setting.
Methods
The research was carried out at King Edward VIII Hospital (KEH) ICU, a 12-bed multidisciplinary ICU in Durban, KwaZulu-Natal, South Africa. This is a closed, intensivist-led ICU, with a nurse-to-patient ratio of 1:1. The ICU serves as a referral ICU for predominantly the eThekwini region but also for the province of KwaZulu-Natal. All referrals are analysed by the critical care team, with the on-call consultant making the final admission decision. A member of the ICU team usually assesses intrahospital referrals physically. A telephonic consultation is mainly used for referrals from outside the hospital. All patients who are discussed within the ICU have a standardised referral proforma completed by the ICU doctor in the unit at the time of the referral.
This was a retrospective review of 500 referral forms of patients referred to the ICU over a 6-month period from September 2016 to February 2017. No referrals were excluded from this study. Biomedical Research Ethics Committee (BE291/17) approval was obtained from the University of KwaZulu-Natal, KEH and the Health Research Committee of the KwaZulu-Natal Department of Health.
Referral data extracted included: the experience of the referring doctor, discussion of the patient with a specialist or another ICU, the outcome of that discussion, the referring discipline, the level of the referring healthcare facility and the reason for referral of the patient to an ICU. A community service medical officer (CSMO) refers to a doctor who has completed their internship and is serving a one-year placement as a junior medical officer prior to full registration as an independent medical practitioner. A grade 1 medical officer (1MO) has 0 - 5 years' experience post registration, a grade 2 medical officer (2MO) has 6 - 10 years' experience post registration, and a grade 3 medical officer (3MO) has >10 years' experience. The levels of referring healthcare facilities refer to state healthcare facilities, except where listed as 'private'. Private healthcare facilities have variable resources but are generally equivalent to a regional or tertiary hospital in the state sector and would be staffed by specialist medical practitioners.
When evaluating the adequacy of a consult, two key metrics were explored. One was whether the necessary data were available during the consult for the ICU team to make an appropriate decision on ICU admission, and the second was whether the patient would have been stable for transfer to the referral ICU if accepted. The adequacy of the data contained on the consult form was assessed by the principal investigator (UVJ) using a standard format analysing clinical data and special investigations. Clinical data were deemed adequate if the basic history and examination areas on the consult proforma had been completed. Special investigations were noted to have been 'done' if the results of these were included in the dedicated areas on the consult proforma, 'not indicated' if the investigation was not necessary for the specific consultation, and 'missing' if the investigation was indicated but the results were not recorded. Any doubts as to the adequacy of clinical data and appropriateness of investigations were resolved by consensus after discussion with a senior intensivist (KdV). No established criteria exist to determine whether a patient is stable for transfer. Patients were deemed unstable for transfer if the patient had any one of the following: a mean arterial pressure (MAP) <65 mmHg, SpO2 <90%, or pH <7.0 on arterial blood gas. These criteria were based on clinical criteria proposed by senior intensivists in the study ICU. While individual patients may have been transferred despite values falling outside the range listed above, these were the initial targets recommended by the unit intensivists.
Patient data that were extracted included: age, gender, working diagnoses, comorbidities, physiological parameters, biochemical parameters and results of radiological and other investigations. The sequential organ failure assessment (SOFA), quick sequential organ failure assessment (qSOFA) and acute physiological and chronic health evaluation (APACHE) II scores were calculated from these data. In the event of missing data, the patient was allocated a score of zero for that respective variable. This was done to under-estimate, as opposed to over-estimate, both the severity of the illness and mortality risk. 'Working hours' were defined as Monday to Friday between 08h00 and 15h59. Any time frame that did not fall within this range was deemed to be 'After hours'.
The referral pathway of the health system in South Africa, and hence referrals to KEH ICU, is tiered, whereby lower-tiered centres, e.g. clinics, first refer to their next higher-tier centre, e.g. district hospitals who then refer to regional centres.[9] Healthcare facilities are expected to refer patients to other facilities that are within their referral area. If the referral did not follow this pathway, it was deemed to be inappropriate.
The outcome of the consultation was classified as accepted, refused or withdrawn. Refused patients were subdivided into three categories, no need (those who were deemed not to require ICU management), futile (where ICU care was deemed to be non-beneficial to that patient owing to the severity of their acute or chronic illness), and no beds (a patient who required ICU but was unable to be accepted owing to a bed or staff shortage). A consult was deemed to be withdrawn when the referring doctor withdrew the request for an ICU bed. The reasons for the referring doctor withdrawing a consultation were grouped as the patient improving and not requiring admission into the ICU, the patient dying before a decision regarding ICU admissions was made, or transfer to another ICU.
The data required for this study were obtained from the referral proforma form and extracted directly onto a Microsoft Excel spreadsheet in chronological order. The consultation forms were assigned a unique identification number that corresponded to the patients' data on the spreadsheet. This procedure was done to ensure no duplication of data occurred and protection of the patients' identity. Re-referrals were treated as a new consultation.
The captured data were analysed using IBM SPSS Statistics for Windows Version 27.0. Categorical variables were described as percentages and compared using the chi-square test or Fisher-Freeman-Halton test, where appropriate. Continuous data were described using median and interquartile range (IQR) as the distribution was generally non-Gaussian. These data were compared using the Mann-Whitney U-test.
Results
A total of 500 referrals were studied over a 6-month period. Demographic and clinical data for these referrals are shown in Table 1. The ages of the referred patients ranged from 9 to 91 years. The most common specific primary diagnoses were pneumonia (14.2%), toxin ingestion (7.6%), cardiac failure (4.8%), renal failure (4.8%) and intraabdominal sepsis (4.6%).
Of the 362 patients referred for ventilatory support, 95.9% were referred for invasive ventilation.
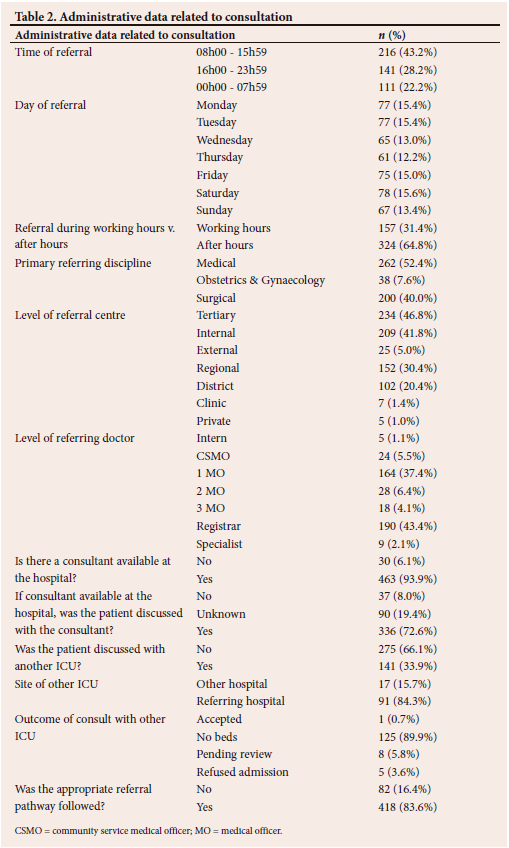
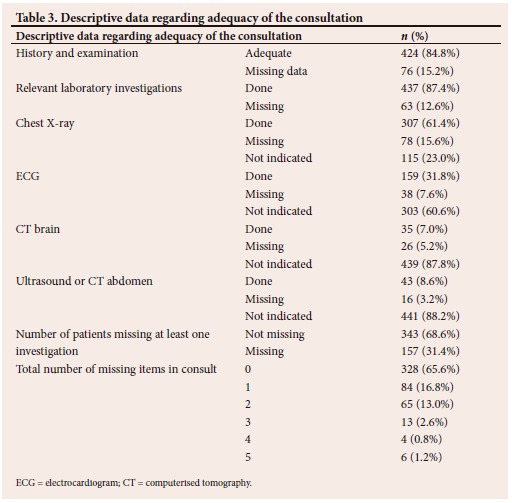
Details of the referral process and pathway are provided in Table 2. The majority of referrals where the appropriate pathway was not followed (n=82) were from regional hospitals (n=52, 63.4%) and district hospitals (n=17, 20.7%) situated outside the referral area of the study hospital. All seven (8.5%) referrals directly from clinics were deemed to be inappropriate. The remainder (n=6, 7.3%) were from tertiary and private hospitals. The adequacy and completeness of the data received for each referral is shown in Table 3.
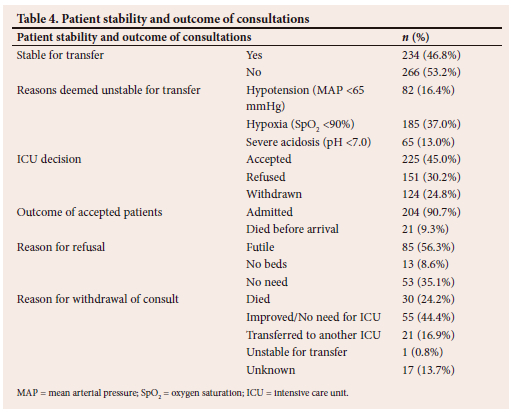
Stability for transfer and the outcomes of the ICU consultations are shown in Table 4. A total of 19.6% of patients were on inotropes at the time of consult, with 40.8% of these patients still hypotensive at the time of consultation.
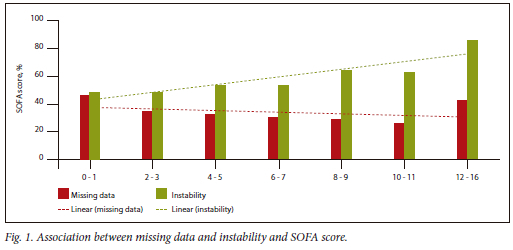
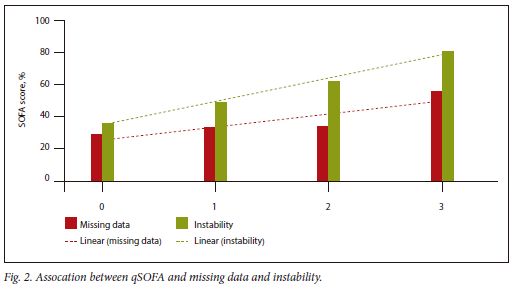
Associations between missing consult data and clinical instability are shown in Table 5. An increased risk of instability was noted in those with either past or current tuberculosis (TB) (68.4% v. 51.2%, p=0.014). When treated as a categorical variable, SOFA remained significantly associated with missing data (p=0.018), with no statically significant association with instability (p=0.575). Fig. 1 illustrates the relationship between SOFA category and missing data and instability. The incidence of missing data tends to decrease with increasing SOFA score, while instability tends to increase with increasing SOFA score. qSOFA was significantly associated with both missing data (p=0.049) and instability (p <0.001). Fig. 2 shows that both missing data and instability tend to increase with increasing qSOFA score.
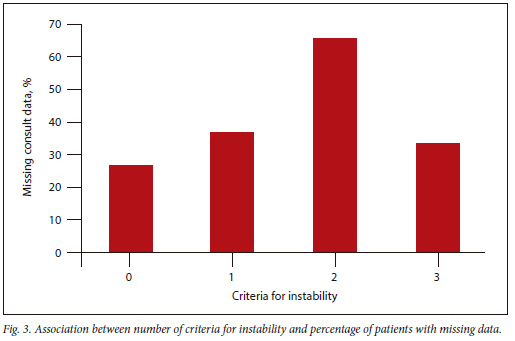
As noted in Table 5, significantly more unstable patients had an investigation missing. There was a significant association between instability at the time of the consult and an increased risk of missing consult data. Furthermore, there was a significant association (p<0.001) between the number of criteria met for instability and the incidence of missing data, as shown in Fig. 3. Data for patients with three criteria for instability are likely to be unreliable as this only included six patients overall.
While there was no statistically significant association between the day of the week on which the consult occurred and missing data (p=0.553) and instability (p=0.052), there was a tendency to increased clinical instability early in the week (Monday and Tuesday) which decreased to a stable, lower level from Thursday to Sunday. When Monday and Tuesday were combined into a single category and compared with Wednesday to Sunday as a single category, this difference became apparent, with an incidence of instability of 64.3% as opposed to 48.4%, respectively (p=0.001).
Discussion
The demographic data for the cohort are noteworthy for its young median age. This is in keeping with data from other ICUs in South Africa and other low-middle-income countries.[2,8,10-14] The spread of primary diagnoses illustrates the triple burden of non-communicable disease, communicable disease and trauma faced by South African ICUs. Although trauma comprised a large proportion of ICU admissions, this is lower than reported in another large South African ICU.[2,10,13] Despite the young median age, the incidence of comorbidities was high at 63.4%. The impact of the HIV epidemic is apparent in this regard, with 24.0% of patients known to be HIV positive, which is in keeping with data from other centres in South Africa.[10,13,14] When comparing our patient cohort with another ICU in the same province, 36.2% of our patients had a qSOFA score >2 v. 60.6% in a study by Khan et al.[10] This trend continued when looking at a study done in Botswana, where their mean APACHE II score was 25 v. 18 in our study.[14] However, when comparing the mean APACHE II score in our study group with high-income countries such as Japan and the USA, no difference was seen, with similar mean APACHE II scores of 18 noted across all three studies.[15,16]
Analysis of the referral pattern data highlights a number of areas where intervention may be appropriate to improve critical care utilisation and outcomes. Referrals to a Level 3 ICU from a clinic should not occur; however, they accounted for 1.4% of ICU referrals in this cohort. Critically ill patients should be triaged to avoid them being managed at, or transported to, clinics that are ill-equipped to deal with such patients. It is also unlikely that patients referred from clinics will have the necessary clinical data and investigations available to make a rational decision on ICU admission, which may likely result in poor utilisation of ICU beds.
The large proportion of referrals from district hospitals (20.4%) is of concern, as these hospitals should be referring patients who are seriously ill or at risk of becoming seriously ill to their regional referral facility prior to the patient requiring ICU. Reasons for this finding may be that patients present late to the district facility when already critically ill, or the medical staff in the district facility do not identify high-risk patients timeously, resulting in up-referrals only once the patient deteriorates and requires critical care.[17] Another reason may be that regional referral facilities, because of their limited resources, have a high threshold for accepting patients from district facilities. Regional facilities appropriately make up the largest proportion of referrals (30.4%). The functioning of ICUs at regional level and the distribution of case severity may be of concern. The Critical Care Society of Southern Africa Guidelines for the Provision of Critical Care Services in South Africa make reference to level 1, 2 and 3 ICUs.[18] Regional hospitals are meant to have level 2 ICUs which should manage critically ill patients requiring support for one or two failing organ systems. The study ICU is a level 3 ICU and should be managing predominantly complex critically ill patients. As 51.8% of patients required only single organ support at referral, it appears that a number of patients who should be managed at lower levels of care are being referred to the level 3 ICU. This may suggest a problem at a regional level where there are too few ICU beds, or that the beds are being used inappropriately. The increased presence of intensivists at regional hospitals may improve the situation.
The high risk of accepted patients from district and regional hospitals dying before arrival in ICU raises concerns about the quality of acute management provided at lower levels of care and the safety of transporting such patients. Increasing critical care education and training for medical, nursing and paramedic staff at these levels may result in better patient outcomes.
The high burden of emergency after-hours consultations has significant implications on staffing and staff wellbeing. While the majority of ICU referrals (56%) are conducted by a senior doctor (MO grade 2 or above), 44% are still conducted by junior doctors. This has potential implications for the quality of the consult and the quality of the resuscitation and transfer of critically ill patients. Even though consultants were available at the hospital in 93.9% of referrals, the consultant's advice was only confirmed to have been sought in 67.2% of the cohort. While this may be due to the advice not being recorded on the consult form, it highlights that consult input is probably not being sought in a large proportion of ICU referrals. This is likely to lead to inappropriate referrals and inadequate optimisation of patients. In 33.9% of referrals, the patient had been discussed with another ICU. While this may be appropriate when the initial ICU has no beds available, the data presented suggest that multiple ICUs are also consulted concurrently. This is inefficient for both the referring doctor and the referral ICUs and speaks to the need for a clearer referral pathway and possibly a province-wide, centrally controlled system of bed allocation. The incorrect referral pathway was used in 16.4% of referrals. This not only creates inefficiencies and burdens on the healthcare system but also puts patients at risk as the inappropriate referral pathway leads to inefficiencies with respect to transport distances and times.[19]
The level of referral centre was significantly associated with the adequacy of the consult data. All referrals from clinics had missing information. This decreased to 36.8% for regional hospital, 27.4% for district hospitals, 12% for external tertiary hospitals and 35.9% for internal referrals. The rate of missing data is considered high, with the ICU team needing to make decisions on ICU admission with incomplete data in approximately a third of patients. This may be due to investigations not being available, or the referring doctor not requesting the investigation. The high rate of missing data from in-patient referrals may be because of a potential bias to more readily accepting a patient from within the hospital, or the physical evaluation of such a patient replacing the need for special investigations in certain circumstances.
The level of the referring doctor is significantly associated with missing data, with specialists showing the highest rate. This may reflect senior doctors relying on clinical information and more focussed investigations, while junior doctors follow a more algorithmic approach, or may reflect poorer quality consults from specialists. The availability of a consultant was, however, associated with a significantly lower risk of missing data.
The appropriate referral pathway was significantly less likely to have been followed in patients with missing data, suggesting either knowledge or system problems being more common in these situations. Patients with missing data were significantly more likely to have central nervous system (CNS) dysfunction, which is likely due to lack of availability of computed tomography (CT) scanners in district and some regional hospitals. In general, patients with missing data tended to have fewer comorbidities and lower severity of illness scores but were more likely to be unstable at the time of consult. The latter finding likely reflects the perception that unstable patients need to be referred to ICU immediately, and therefore investigations are not performed. This misperception should be addressed with a focus on attempts at stabilisation prior to ICU referral.
Patient clinical stability was related to the level of the referring institution. The trend of in-hospital patients being more unstable than patients from other tertiary centres is in keeping with international literature.[20] A possible reason may be a longer stabilisation period for external patients to mitigate risks before interhospital transfer.[19] Patients referred for inotropic support were significantly more likely to be unstable, with many on inotropic support yet hypotensive at the time of consult. This may necessitate education and training in more effective inotrope usage. qSOFA is significantly associated with increased risk of instability and may be a useful tool for non-ICU doctors to triage their patients. [21]
The majority of consults for ICU admission occurred after hours and is in keeping with other studies. [11,16,22] The greater instability of patients referred on Mondays and Tuesdays v. the remainder of the week is interesting. This may reflect a differential between staff and care over weekends and an increased referral on Monday and Tuesday of patients who had deteriorated over the weekend, but needs further investigation.
Study limitations
This was a retrospective, single-centre study, which may lead to bias and limit external validity. However, as a large referral unit for the second most populous province in South Africa, the study site may be reflective of critical care services in many areas of the country and other resource-limited settings. The ICU referral forms were filled in by any of the doctors in the ICU on the day. As doctors were of varying levels of experience, this may have resulted in bias when completing the referral form. Any missing information on the consult form was assumed to have been not available at the time of the consultation. This may not have been the case as the receiving doctor may have omitted the required information. The approach to missing data for the severity of illness scores may have resulted in a bias to reporting lower severity of illness scores. However, this was applied consistently and was deemed to be better than potentially falsely inflating severity of illness scores. While there are instances where deviating from the referral pathway may be necessary, it was not possible to assess this systematically from the consultation forms and thus we may have overestimated the number of inappropriate referrals.
Conclusion
In South Africa, the demand for intensive care services in state facilities exceeds the supply. As a scarce resource, appropriate referral is essential to ensure distributive justice and better outcomes for patients. This study describes the nature of cases referred to a single centre and that appropriate senior support may not be properly utilised or available. Patients referred for ICU care are often too unstable to transport and have missing data that are necessary to make an appropriate decision on ICU admission. More emphasis needs to be placed on the training of doctors to appropriately assess and stabilise critically ill patients. There are numerous factors that influence referral patterns, and more studies are required to identify factors that may improve resource utilisation and distribution.
Declaration. None.
Acknowledgements. None.
Author contributions. UVJ conceived the idea, collected and analysed the data and wrote the article (with proofreading and corrections by KDV, DLS and PDG). KDV contributed to the development of the study design, analysed the data and formulated the tables.
Funding. None.
Conflicts of interest. None.
References
1. Treasury RoSAN. Budget Review. In: Treasury N, editor. Online; 2023. p. 58. ISBN: 978-0-621-508338 (accessed 26 February 2023). https://www.treasury.gov.za/documents/national%20budget/2023/review/FullBRpdf [ Links ]
2. Mathivha LR. ICUs worldwide: An overview of critical care medicine in South Africa. Crit Care 2002,6(1):22. https://doi.org/10.1186/cc1449 [ Links ]
3. Blecher M, Davén J, Kollipara A, Maharaj Y, Mansvelder A, Gaarekwe O. Health spending at a time of low economic growth and fiscal constraint. S Afr Health Rev 2017,2017(1):25-39. [ Links ]
4. Cohen RI, Eichorn A, Silver AJMa. Admission decisions to a medical intensive care unit are based on functional status rather than severity of illness. A single center experience. Minerva Anestesiologica 2012;78(11):1226-1233. [ Links ]
5. Bhagwanjee S, Scribante JJ. National audit of critical care resources in South Africa-unit and bed distribution. S Afr Med J 2007;97(12):1311-1314. https://doi.org/10.7196/SAMJ.555. [ Links ]
6. Murthy S, Wunsch HJC. Clinical review: International comparisons in critical care-lessons learned. Critical Care 2012;16(2):218. http://doi.org/10.1186/cc11140 [ Links ]
7. Gopalan P, De Vasconcellos K. Factors influencing decisions to admit or refuse patients entry to a South African tertiary intensive care unit. S Afr Med J 2019-,109(9):645-651. http://.doi.org/10.7196/samj.2019.v109i9.13678 [ Links ]
8. Gordon K, Allorto N, Wise RJ. Analysis of referrals and triage patterns in a South African metropolitan adult intensive care service. S Afr Med J 2015,105(6):491-495. http://doi.org/10.7196/samj.9007 [ Links ]
9. Health K-NDo. Referral System: Levels of Health Care. 4 January 2022 (accessed 15 May 2022). http://www.kznhealth.gov.za/Referral-system.htm [ Links ]
10. Khan S, Wise R, Savarimuthu SM, Anesi GL. Association between pre-intensive care unit (ICU) hospital length of stay and ICU outcomes in a resource-limited setting. Southern Afr J Crit Care (Online) 2021;37:98-103. https://doi.org/10.7196/SAJCC.2021.v37i3.500 [ Links ]
11. Prin M, Ji R, Kadyaudzu C, Li G, Charles A. Associations of day of week and time of day of ICU admission with hospital mortality in Malawi. Tropical Doctor 2020,50(4):303-311. https://doi.org/10.1177/0049475520936011 [ Links ]
12. Hurri H, Scribante J, Perrie H, Chetty S. Profile of ICU bed requests at Helen Joseph Hospital. Wits J Clin Med 2020,2(1):31-36. https://doi.org/10.18772/26180197.2020.v2n1a5 [ Links ]
13. Singh M, Maharaj R, Allorto N, Wise R. Profile of referrals to an intensive care unit from a regional hospital emergency centre in KwaZulu-Natal. Afr J Emerg Med 2021,11(4):471-476. https://doi.org/10.1016/j.afjem.2021.07.006 [ Links ]
14. Milan AO, Cox M, Molebatsi K. Results from the first audit of an intensive care unit in Botswana. Southern Afr J Crit Care 2020,36(1):23-27. https://doi.org/10.7196/sajcc.2020.v36i1.395 [ Links ]
15. Namikata Y, Matsuoka Y, Ito J, et al. Association between ICU admission during off-hours and in-hospital mortality: A multicenter registry in Japan. J Intensive Care 2022,10(1):41. https://doi.org/10.1186/s40560-022-00634-3 [ Links ]
16. Orsini J, Rajayer S, Ahmad N, et al. Effects of time and day of admission on the outcome of critically ill patients admitted to ICU. J Community Hosp Intern Med Perspect 2016,6(6):33478. https://doi.org/10.3402/jchimp.v6.33478 [ Links ]
17. Engdahl Mtango S, Lugazia E, Baker U, Johansson Y, Baker T. Referral and admission to intensive care: A qualitative study of doctors' practices in a Tanzanian university hospital. PLoS One 2019,14(10):e0224355. https://doi.org/10.1371/journal.pone.0224355 [ Links ]
18. Joynt GM, Gopalan DP, Argent AA, et al. The Critical Care Society of Southern Africa Consensus Statement on ICU Triage and Rationing (ConICTri). S Afr Med J 2019,109(8b):613-629. https://doi.org/10.7196%2fsajcc.2019.v35i1b.383 [ Links ]
19. Scribante J, Bhagwanjee S. National audit of critical care resources in South Africa: Transfer of critically ill patients. S Afr Med J 2007,97(12 Pt 3):1323-1326. https://doi.org/10.7196/SAMJ.556 [ Links ]
20. Blakeman TC, Branson RD. Inter- and intra-hospital transport of the critically ill. Respir Care 2013,58(6):1008-1023. https://doi.org/10.4187/respcare.02404 [ Links ]
21. Savarimuthu SM, Cairns C, Allorto NL, et al. qSOFA as a predictor of ICU outcomes in a resource-limited setting in KwaZulu-Natal Province, South Africa. South Afr J Crit Care 2020,36(2):92-95. http://doi.org/10.7196/sajcc.2020.v36i2.433 [ Links ]
22. Brunot V, Landreau L, Corne P, et al. Mortality associated with night and weekend admissions to ICU with on-site intensivist coverage: Results of a nine-year cohort study (2006-2014). PLoS One 2016,11(12):e0168548. https://doi.org/10.1371/journal.pone.0168548 [ Links ]
 Correspondence:
Correspondence:
U V Jaganath
ushirjaganath@gmail.com
Accepted 28 May 2023














