Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
Southern African Journal of Critical Care (Online)
versão On-line ISSN 2078-676X
versão impressa ISSN 1562-8264
South. Afr. j. crit. care (Online) vol.39 no.1 Pretoria Mar. 2023
http://dx.doi.org/10.7196/SAJCC.2023.v39i1.559
RESEARCH
Healthcare professionals' perception of knowledge and implementation of Patient Safety Incident reporting and learning guidelines in specialised care units, KwaZulu-Natal
T M H GqaleniI; S W MkhizeII
IMN (SA), RN (SA); School of Nursing and Public Health, University of KwaZulu-Natal, Durban, South Africa
IIPhD, MBA, RN (SA); School of Nursing and Public Health, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND: Despite the implementation of intervention strategies, incidents in specialised care units remain high and are of serious concern, worldwide
OBJECTIVE: To assess the healthcare professionals' perception of knowledge and implementation of patient safety incident (PSI) reporting and learning guidelines in specialised care units of three selected public hospitals in KwaZulu-Natal, South Africa
METHODS: The study used a descriptive, cross-sectional survey design. A purposive sample targeted 237 healthcare professionals. An online structured questionnaire collected the data. Descriptive and inferential statistics were used to analyse data
RESULTS: A total of 181 questionnaires were returned, yielding a response rate of 76%. Notably, 83% of respondents had high-perceived knowledge of the PSI reporting and learning guidelines, while 98% had low perceptions of their implementation. The current unit (p=0.002) and shift of the day (p=0.008) were factors associated with the perception of good knowledge of PSI reporting and learning guidelines, as indicated by a p-value <0.05. The respondents' age (p=0.05), current unit (p=0.015), and shift of the day (p=0.000) were significantly associated with the perception of poor implementation of the PSI reporting and learning guidelines
CONCLUSION: The respondents demonstrated a good perception of knowledge of PSI reporting and learning guidelines; however, the perception of the implementation was poor. Therefore, a revised implementation strategy coupled with periodical in-service training for healthcare professionals is recommended, to foster and facilitate effective adherence to PSI reporting and learning guidelines
Keywords: Patient safety, incidents, guidelines, implementation, critical care, healthcare professionals.
Despite the implementation of patient safety strategies, patient safety incidents (PSIs) in specialised care units remain high and are of serious concern worldwide.[1,2] According to the World Health Organization (WHO) in 2017, globally, the healthcare system still demonstrates unacceptably high rates of PSIs and preventable deaths.[1,3] In response to curbing the high rate of PSIs, a global effort was made by the WHO member states to develop patient safety strategies, relevant to their nations, to create a safer environment in the healthcare system.[4] The aim of these patient safety guidelines was to guide clinicians to implement evidence-based decisions and improve clinical outcomes. Organisations and movements have been created to focus on patient safety; however, this is not the case in developing countries.[5] Clarity, consistency, and standardisation in patient safety need to be developed.[5]
In South Africa (SA), the implementation of PSI reporting and learning systems guidelines, as recommended by the KwaZulu-Natal Department of Health (KZN DoH) in line with the National Department of Health (NDoH), has provided no clear improvement in the reduction of PSIs. [6] SA hospitals face various challenges, which include a lack of patient safety guidelines implementation.[6] Abraham et al. revealed that current documentation and guidelines relating to patient safety were well known and established within the hospital, but full implementation of these guidelines was lacking.[7]
Incorporating guidelines into critical care practice is recognised as a crucial requirement for the optimal care of critically ill patients; [8] however, implementation of guidelines is often insufficient, resulting in frequent poor adherence in specialised critical care units (SCUs).[9,10] In this study, SCUs include critical care and high care units that care for unstable patients with acute, life-threatening illnesses or injuries and involve multiple skills and specialties. Poor knowledge of patient safety and healthcare professionals' inadequate level of education may contribute to the lack of improvement in patient safety.[11,12] Adequately prepared healthcare professionals with knowledge, attitudes, and skills are necessary to improve patient safety.[3,13] Working experience, information on patient safety during initial education, and information on patient safety during continuing education have been significantly associated with patient safety.[3] There is limited research on healthcare professionals' perception of knowledge and the implementation of PSI reporting and learning guidelines. This study aimed to assess the perception of knowledge and implementation of PSI reporting and learning guidelines by healthcare professionals in SCUs of KZN Province.
Methods
Study design
A descriptive, cross-sectional survey, which was part of the larger mixed-method design, collected quantitative data from the healthcare professionals working in the specialised care units.
Study setting
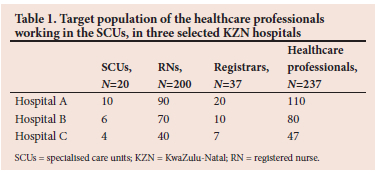
The study took place in SCUs of three selected public hospitals in two districts of KZN. Two hospitals (A and C), situated in the eThekwini district, provide both secondary, and tertiary services, and the third tertiary hospital (B) is in the uMgungundlovu district. These districts were chosen because they are the largest in the province, with the most state-owned hospitals equipped with different categories of SCUs, admitting miscellaneous patient profiles, and therefore provided a more comprehensive field for the research project. The selected hospitals treated patients from both urban and rural areas. Twenty SCUs participated in the study, consisting of both critical care units (CCUs) and high care units, as illustrated in Table 1.
Population, sample and sampling
The researcher used a purposive sampling strategy to select specialist critical care nurses and registrars working in the SCUs. Critical care nurses undergo a critical-care training course or orientation that includes essential information on the care of critically ill patients. [14] The registrars are qualified medical doctors receiving advanced training in a specialist field of medicine to become a consultant in that specialty.[15] All the healthcare professionals with >1 year's experience working in the SCUs, day and night duty, and willing to participate met the inclusion criteria. The target population comprised 762 healthcare professionals working in the SCUs, who were involved in the implementation of PSI reporting and learning guidelines in the selected SCUs. For power analysis, and with the help of the statistician, a Raosoft Sample Size Calculator (2004) (Raosoft Inc., USA) assisted in recommending the minimum size of the sample to yield sufficiently valid results. Using the Raosoft parameters of margin error of 5%, the confidence level of 95%, the population size of 762, and the response distribution of 50%, the recommended sample size was 237.
Research tool
The researcher adapted the SA National Guidelines for Patient Safety Incident Reporting and Learning[1] to suit the purpose of the study, as to the researcher's knowledge, no previous studies had researched the topic at the time the study was conducted. Section A underwent modification to include the different types of CCUs, for example, medical CCU, as well as the work shift the healthcare professionals were working. Section B and C items, on the perception of knowledge and implementation of PSI reporting and learning guidelines, were modified to specifically suit the SCUs. The adapted questionnaire consisted of three sections.
Section A - Demographics of the respondents, included five items.
Section B - Healthcare professionals' perception of knowledge of the PSI reporting and learning guidelines, included six items. Responses were rated on a Likert scale from strongly disagree (1) to strongly agree (5), with a higher score associated with good perception of knowledge of PSI reporting and learning guidelines.[16] The overall level of perception of knowledge of the PSI reporting and learning guidelines was categorised as follows: 80 - 100% as good knowledge, 60 - 79% as moderate, and <60% as poor knowledge.
Section C - Healthcare professionals' perception of the implementation of PSI reporting and learning guidelines was assessed on 12 items. Similarly, responses were rated on a Likert scale from strongly disagree (1) to strongly agree (5), with a higher score associated with positive perception of the implementation of PSI reporting and learning guidelines. The categorisation of the overall level of perception of the implementation of the PSI reporting and learning guidelines was as follows: 80 - 100% as positive perception and <80% as negative perception.
Validity and reliability
The adapted instrument was sent to three clinical and three academic experts, who reviewed the content and confirmed it as adequate. The experts had a critical care specialty, and a depth of knowledge and skill in implementing PSI guidelines in SCUs, with working experience of more than 10 years. The items of the research instrument were aligned with the objectives of the study to ensure content validity. The instrument was pretested on a sample of five healthcare professionals working in the SCUs of the research setting. The purpose of pre-testing was to ensure the questions were clear and easily understandable for the respondents. Their responses were consistent and no ambiguity was identified during the pretest, indicating the instrument was reliable. The collected data during pretesting was not included in the final analysis. Cronbach's alpha coefficient for the current research tool was 0.9, meaning the instrument was an excellent measure of the variables under study, as indicated by George and Mallery.[17]
Data collection process
The study was conducted through an online survey, following the COVID-19 protocols, collecting quantitative data over a period of 3 months, from March to May 2021. After obtaining ethical clearance, the researcher sought permission from the relevant selected gatekeepers before data collection. The researcher created a link and emailed the questionnaires to the respondents, or posted them on the organisation's intranet. The respondents had to click on the link, only linked to the researcher's email address; thus the researcher had access to the response instantly.
Ethical considerations
The University of KwaZulu-Natal's Human Science Research Ethics Committee (ref. no. HSSREC/00001651/2020) and the Department of Health (NHRD ref. no. Kz_202010_0240) granted ethical clearance before data collection. The online questionnaire consisted of an information sheet explaining the study, and the respondents had the option of giving consent before they proceeded to fill in the questionnaire. Anonymity of the respondents' responses was ensured as the researcher used online means of data collection and did not see the respondents physically. Confidentiality was ensured by assuring the respondents that their responses were not going to be divulged without their permission. Codes were assigned to each questionnaire so that it was not possible to associate the questionnaire with the respondent. Additionally, an electronic password that only allowed the researcher access was created.
Data analysis
The researcher entered the data onto an Excel spreadsheet (Microsoft, USA), and cleaned and coded it before it was transferred to SPSS 27 (IBM, USA). Descriptive statistics described the demographic characteristics, perceived knowledge, and implementation of the PSI reporting and learning guidelines. Results were presented as frequencies and percentages. With a p-value set at 0.05, inferential statistics of the X2 test established an association between demographic characteristics and perceived knowledge and implementation of the PSI reporting and learning guidelines. Pearson correlation coefficient (r) examined the relationship between perceived knowledge and implementation in terms of magnitude, strength, and direction.
Results
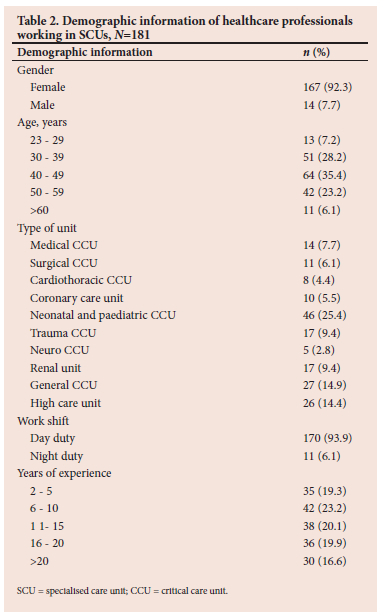
Of the 237 questionnaires distributed, 181 were returned, yielding a response rate of 76%. According to Nulty,[18] a response rate of more than 73% is considered good. Registered nurses (RNs) (n=170) and registrars (n=11) completed and returned the online questionnaires.
Demographic profile of respondents
The majority (64.7%) of respondents were >40 years of age, and 80% of healthcare professionals had >6 years of experience in SCUs, as illustrated in Table 2.
Healthcare professionals' perception of the knowledge of the PSI reporting and learning guidelines
The scale was based on a Likert scale and only the highest and lowest response for each item is mentioned. Nearly half of the respondents (49.7%) agreed regarding the categorisation of PSI reporting guidelines and 54.1% agreed that each category was further explained by the severity of patient outcome. Approximately 52% agreed regarding consistent surveillance of near misses, and 54.7% agreed regarding prompt reporting of near misses as soon as they become aware of them to promote quality patient care. Although 49.7% agreed regarding timeously reporting and investigation of the root cause analysis (RCA), half of the respondents (50.3%) disagreed that policies and guidelines were understood by RNs/registrars working in SCUs (Table 3).
Healthcare professionals' perception of the implementation of the PSI reporting and learning guidelines
While 44.2% disagreed regarding creation of adequate awareness of the implementation of the PSI reporting guidelines at the institution, only 11.0% strongly affirmed being involved in the implementation. Only 4.4% strongly agreed that Patient Safety Committees had been established and 36.5% disagreed that a simple and quick system of reporting PSIs had been provided by their organisation. Although 47.5% agreed that adhering to the existing PSI reporting system and guidelines was part of staff performance criteria, 42.0% disagreed that adherence of specialised units to PSI reporting occurred. More than half (54.7%) disagreed regarding the existence of implementation of preventive measures to reduce the incidence of PSIs and their reoccurrence, only 4.4% strongly agreed that these measures were effective. While 53.6% agreed regarding analysis of PSI data and immediate action to mitigate harmful consequences of the PSIs, 40.9 % and 54.1 % disagreed regarding existence of support structures and efficient record keeping of PSIs within organisations, respectively (Table 4).
The overall level of perception of knowledge and implementation of PSI reporting and learning guidelines
Table 5 presents the overall perception of healthcare professionals on knowledge of PSI guidelines and implementation scores. Most of the respondents (83.4%) revealed good perception of knowledge on PSI reporting and learning guidelines. In contrast, only 2.2% had a positive perception regarding the implementation of the PSI reporting and learning guidelines.
Demographic factors associated with the perception of knowledge and implementation communication of the PSI reporting and learning guidelines
Pearson's x2 test was used to determine the statistical significance between variables, as illustrated in Table 6. Current unit and shift of the day were factors associated with the perception of knowledge, while age, current unit, and shift of the day were significantly associated with the perception of the implementation of the PSI reporting and learning guidelines, as indicated by a p-value <0.05 (Table 6). This means that healthcare professionals working day shift in certain units were able to implement the PSI guidelines.
Discussion
The purpose of this study was to assess the perception of knowledge and implementation of PSI reporting and learning guidelines in SCUs.
Perception of knowledge of the PSI reporting and learning guidelines
This study revealed that the respondents' perception of knowledge of PSI reporting and learning guidelines was good; this could be attributed to formal education as the majority have specialised education and training. One of the common facilitators of patient safety implementation is education and training opportunities.[19,20] Furthermore, work experience, educational qualification, information regarding patient safety during initial education, and having information concerning patient safety during continuing education were factors significantly associated with knowledge of patient safety.[3,21,22] However, respondents confirmed that the policies and guidelines were not well understood. A similar study revealed that unclear policies, guidelines, and structured formats can also lead to considerable variation in the policies.[23,24]
Perception of the implementation of the PSI reporting and learning guidelines
The respondents had the perception of poor implementation of PSI reporting and learning guidelines in their units. A gap in the communication of patient safety was identified; therefore the recommendation was for the implementation of continuing patient safety education programmes in terms of day courses, safety walk-rounds, conferences, and meetings.[11,25] A similar study affirms that principles acquired from safety awareness campaigns and workshops in the hospitals were also not implemented by staff. [7] The study further revealed that healthcare professionals lacked organisational support, patient safety committees, simple incident reporting systems, and adherence to the PSI reporting and learning guidelines.[26,27]
Age, current unit, and shift of the day were significantly associated with the perception of poor implementation of the PSI reporting and learning guidelines. Research has found that a nurse's age, education, position, and nursing experience have a statistically significant association with their knowledge level.[11,28] This may suggest that certain units were active in the implementation of the PSI guidelines, compared with others, and certain shifts of the day enable the healthcare professionals to implement PSI guidelines. Similar studies found some differences between the working units of healthcare professionals related to safety knowledge.[3,28] Since this study was undertaken in various SCUs, some units may have more updates regarding patient safety than others. This could have improved the implementation of PSI guidelines, compared with their counterparts.
The respondents also indicated the existence of preventative measures; however, they were not effective in reducing the reoccurrence of the PSIs in the SCUs. Similar studies affirm that lack of clinical guidelines, lack of an effective and targeted system for proper monitoring of the programmes, not localising patient safety knowledge, and failure to implement planned programmes to prevent and decrease errors, were challenges to implementing patient safety programmes in hospitals.[29,30]
Most professionals had >6 years of work experience in the SCUs; it is therefore perceived that with this level of work experience healthcare professionals should have adequate knowledge and skill, which should lead to effective implementation of the PSI guidelines.[13,28]
Limitations of the study
The study took place in three government hospitals only, in one province, which limits the generalisability of the results to private hospitals and other provinces in South Africa. Only the respondent's perceptions of knowledge and implementation of PSI reporting and learning guidelines were elicited, not the actual knowledge and observed implementation. Information bias was quite possible as the respondents might have given more or less information based on a Likert scale. Recall bias was also possible since the respondents were asked to recall information on PSIs.
Conclusion
The respondents demonstrated perception of good knowledge of PSI reporting and learning guidelines; however, perception of the implementation of the PSI reporting and learning guidelines was poor. Therefore, a revised implementation strategy coupled with periodical in-service training for healthcare professionals is recommendeded, to foster and facillitate the already available implementation strategies for effective adherence to PSI reporting and learning guidelines. In addition, a situational analysis needs to be conducted to identify barriers that lead to poor perception of implementation of the PSI reporting and learning guidelines, and to devise strategies that are practical in the facilitation of implementation of PSI reporting and learning guidelines.
Declaration. This manuscript is submitted as partial fulfilment of the requirements for a PhD at the University of KZN.
Acknowledgements. Gatekeepers and respondents from the three selected hospitals.
Author contributions. TMHG contributed to the conceptualisation of the project, study design, data collection, data analysis, drafting of the manuscript and editing of the manuscript. SWM contributed to the study design, data analysis and editing of the manuscript.
Funding. The project was funded by the University Capacity Development Programme and National Research Foundation Thuthuka funding.
Conflicts of interest. None.
References
1. World Health Organization . National Guideline for Patient Safety Incident Reporting and Learning in the Public Health Sector of South Africa. Geneva: WHO, 2017. [ Links ]
2. Gqaleni TM, Bhengu BR. Adverse events reporting system as experienced by critical-care nurses in KwaZulu-Natal, South Africa. Afr J Nurs Midwifery 2018;20(1):1-14. [ Links ]
3. Wake AD, Tuji TS, Gonfa BK, et al. Knowledge, attitude, practice and associated factors towards patient safety among nurses working at Asella Referral and Teaching Hospital, Ethiopia: A cross-sectional study. PLoS ONE 2021;16(7):e0254122. https://doi.org/10.1371/journal.pone.0254122 [ Links ]
4. World Health Organization. World Alliance for Patient Safety: WHO Draft Guidelines for Adverse Event Reporting and Learning Systems: From Information to Action. Geneva: WHO, 2005. [ Links ]
5. Galadanci HS. Protecting patient safety in resource-poor settings. Best Pract Res Clin Obstet Gynaecol 2013;27(4):497-508. https://doi.org/10.1016/j.bpobgyn.2013.03.006 [ Links ]
6. Mgobozi P, Mahomed OH. Epidemiology of patient safety incidents in a long-term rehabilitative hospital in KwaZulu-Natal, South Africa (April 2011 to March 2016). Curationis 2021;44(1):1-6. [ Links ]
7. Abraham V, Meyer JC, Godman B, Helberg E. Perceptions of managerial staff on the patient safety culture at a tertiary hospital in South Africa. Int J Qual Stud Health Well-being 2022;17(1):2066252. https://doi.org/10.1080/17482631.2022.2066252 [ Links ]
8. Rosa RG, Teixeira C, Sjoding M. Novel approaches to facilitate the implementation of guidelines in the ICU. J Crit Care 2020;60:1-5. https://doi.org/10.1016/j.jcrc.2020.07.014 [ Links ]
9. Jeffs L, Hayes C, Smith O, et al. The effect of an organizational network for patient safety on safety event reporting. Eval Health Prof 2014;37(3):366-378. [ Links ]
10. Costa DK, White MR, Ginier E, et al. Identifying barriers to delivering the awakening and breathing coordination, delirium, and early exercise/mobility bundle to minimize adverse outcomes for mechanically ventilated patients: A systematic review. Chest 2017;152(2):304-311. https://doi.org/10.1016/j.chest.2017.03.054 [ Links ]
11. Asem N, Sabry HA, Elfar E. Patient safety: Knowledge, influence and attitude among physicians: An exploratory study. J Egyptian Public Health Assoc 2019;94(1):1-9. [ Links ]
12. World Health Organization. WHO Patient Safety Research: Better Knowledge for Safer Care. Geneva: WHO, 2009. [ Links ]
13. Brasaite I, Kaunonen M, Suominen T. Healthcare professionals' knowledge, attitudes and skills regarding patient safety: A systematic literature review. Scand J Caring Sci 2015;29(1):30-50. https://doi.org/10.1111/scs.12136 [ Links ]
14. South African Nursing Council. Education and training. https://www.sanc.co.za/education_and_training/ (accessed on 14 September 2022). [ Links ]
15. Health Professions Council of South Africa. Section 2(1) of the Health Professions Act. Pretoria. 2014. https://www.hpcsa.co.za/ (accessed on 14 September 2022). [ Links ]
16. Schnall R, Stone P, Currie L, Desjardins K, John RM, Bakken S. Development of a self-report instrument to measure patient safety attitudes, skills, and knowledge. J Nurs Scholarship 2008;40(4):391-394. [ Links ]
17. George D, Mallery P. IBM SPSS Statistics 26 Step by Step: A Simple Guide and Reference. Abingdon-on-Thames: Routledge, 2019. [ Links ]
18. Nulty DD. The adequacy of response rates to online and paper surveys: What can be done? Assess Eval Higher Educ 2008;33(3):301-314. [ Links ]
19. Health Quality Ontario. Patient safety learning systems: A systematic review and qualitative synthesis. Ont Health Technol Assess Ser 2017;17(3):1. [ Links ]
20. Sahlstrom M, Partanen P, Rathert C, Turunen H. Patient participation in patient safety still missing: Patient safety experts' views. Int J Nurs Pract 2016;22(5):461-469. https://doi.org/10.1111/ijn.12476 [ Links ]
21. Kavuluru V. Knowledge and attitude of nurses on patient safety: A systematic review. Int J Adv Nurs Manage 2022;10(2):156-160. [ Links ]
22. Nadarajan SP, Karuthan SR, Rajasingam J, Chinna K. Attitudes toward patient safety among medical students in Malaysia. Int J Environ Res Public Health 2020;17(21):7721. [ Links ]
23. Liukka M, Hupli M, Turunen H. Problems with incident reporting: Reports lead rarely to recommendations. J Clin Nurs 2019;28(9-10):1607-1613. https://doi.org/10.1111/jocn.14765 [ Links ]
24. Alquwez N. Association between nurses' experiences of workplace incivility and the culture of safety of hospitals: A Cross-sectional Study. J Clin Nurs 2023;32(1-2):320-331. Epub 2022. https://doi.org/10.1111/jocn.16230. [ Links ]
25. El-Shabrawy E, Anwar M, Mostafa Z. Assessment of patient safety culture among health care workers in Beni-Suef University Hospital, Egypt. Egyptian J Commun Med 2017;35(3):11-9. [ Links ]
26. Lu L, Ko Y-M, Chen H-Y, Chueh J-W, Chen P-Y, Cooper CL. Patient safety and staff well-being: Organizational culture as a resource. Int J Environ Res Public Health 2022;19(6):3722. https://doi.org/10.3390/ijerph19063722 [ Links ]
27. Al Hamid A, Malik A, Alyatama S. An exploration of patient safety culture in Kuwait hospitals: A qualitative study of healthcare professionals' perspectives. Int J Pharm Pract 2020;28(6):617-625. https://doi.org/10.1111/ijpp.12574 [ Links ]
28. Brasaite I, Kaunonen M, Martinkenas A, Mockiene V, Suominen T. Health care professionals' knowledge regarding patient safety. Clin Nurs Res 2017;26(3):285-300. https://doi.org/10.1177/1054773816628796 [ Links ]
29. Naderi S, Zaboli R, Khalesi N, Nasiripour AA. Factors affecting patient safety: A qualitative content analysis. Ethiopian J Health Dev 2019;33(2). [ Links ]
30. Doshmangir L, Ravaghi H, Akbari Sari A, Mostafavi H. Challenges and solutions facing medical errors and adverse events in Iran: A qualitative study. J Hospital 2016;15(1):31-40. [ Links ]
 Correspondence:
Correspondence:
T M H Gqaleni
gqalenit@ukzn.ac.za
Accepted 2 February 2023














