Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
Southern African Journal of Critical Care (Online)
versión On-line ISSN 2078-676X
versión impresa ISSN 1562-8264
South. Afr. j. crit. care (Online) vol.39 no.1 Pretoria mar. 2023
http://dx.doi.org/10.7196/SAJCC.2023.v39i1.550
RESEARCH
Malawian critical care nurses' views on the implementation of an educational intervention to enhance sustained use of an evidence-based endotracheal tube cuff pressure management guideline: A survey study
F MpasaI; Dalena R M van RooyenII; P J JordanIII; D VenterIV; W ten Ham-BaloyiV
IDip RN, Dip Int Care Nurs, BSc (Nurs Edu), MCur, PhD; Lecturer, Department of Nursing and Midwifery Science, Faculty of Health Sciences, Mzuzu University, Luwinga, Malawi; Former PhD candidate, Department of Nursing Science, Faculty of Health Sciences, Nelson Mandela University, Gqeberha, South Africa
IIBCur, MCur, Dip Int Care Nurs, Dip Nurs Edu, PhD; Deputy Dean, Faculty of Health Sciences, Nelson Mandela University, Gqeberha, South Africa
IIIRN, MBA, PhD; Associate Professor and Head, Department of Nursing and Midwifery, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IVPhD; Consultant Statistician, Faculty of Health Sciences, Nelson Mandela University, Gqeberha, South Africa
VBCur, MCur, Dip Nurs Edu, PhD; Research Associate, Faculty of Health Sciences, Nelson Mandela University, Gqeberha, South Africa
ABSTRACT
BACKGROUND: Evidence-based guidelines can assist critical care nurses in promoting best practices, including those related to endotracheal tube cuff pressure management. However, these guidelines require tailored strategies to enhance their implementation, uptake, and sustained use in practice
OBJECTIVES: To evaluate Malawian critical care nurses' views on the implementation of an endotracheal tube cuff pressure management guideline to enhance sustained guideline use
METHODS: An explorative-descriptive survey design was employed, using a questionnaire with closed- and open-ended questions that was distributed after implementation of an educational intervention based on an endotracheal tube cuff pressure management guideline. The questionnaire had a Cronbach's alpha score of 0.85
RESULTS: A total of 47 nurses working in four public and two private hospital intensive care units in Malawi participated. Quantitative findings showed that the majority of the participants (92%) indicated that the strategies used for the group that received the full intervention including both active (monitoring visits) and passive (a half-day educational session using a PowerPoint presentation, and a printed guideline and algorithm) strategies (intervention 1 group) were useful, clear and applicable and enhanced implementation of the guideline. These results were statistically significant (mean (standard deviation) 1.86 (0.84); f=6.07; p<0.0005). Qualitative data revealed three major themes related to recommendations for uptake and sustained use of the guideline in nursing practice: the guideline needs to be translated, updated, and made available to ICU staff; implementation strategies (continuous supervision and follow-up); and facilitating factors for successful implementation (education and training on guideline content, resources, and commitment to best practices
CONCLUSION: The study highlighted that although the implementation strategies used were positively received by participants, they need to be further tailored to their context to enhance guideline uptake and sustained use in practice. Further study is required to ensure that tailored implementation strategies facilitate guideline uptake and sustained use, specifically in resource-constrained contexts
Keywords: implementation strategies, evidence-based guideline, endotracheal tube cuff pressure management, intensive care units, ICUs, critical care nurses.
In critical care, if endotracheal cuff pressure is not well managed, complications such as aspiration pneumonia, tracheal stenosis, adhesions and tracheomalacia may result.[1,2] Minimising such complications requires implementation of evidence-based guidelines designed to promote best practices, minimise practice variation, decrease healthcare costs, and improve clinical outcomes.[3,4] Although a number of guidelines have been developed for nurses, including guidelines on endotracheal tube cuff pressure management, guideline development alone does not
automatically lead to implementation, uptake and sustained use of the guideline in practice.[3] Research indicates that because of a variety of barriers, guidelines are often not well implemented or adhered to.[5,6] In the critical care nursing context, barriers have been reported to include inadequate resources; lack of time, skills, education, knowledge and guidance; and role ambiguities.[6,7] Non-adherence to guidelines can result in unnecessary, inadequate or potentially harmful practices.[5] For example, non-adherence to practices recommended in guidelines for endotracheal cuff pressure management by critical care nurses can lead to complications such as sore throat, tracheal mucosa ulcers, tracheal rupture and subglottic stenosis resulting from over-inflation of the cuff, and aspiration of gastric contents, aspiration pneumonitis and pneumonia resulting from under-inflation of the cuff.[8,9] In Malawi, during the time of the present study, it was observed that, owing to lack of guidelines, nurses working in intensive care units (ICUs) used manual palpation of the balloon cuff to monitor cuff pressure, which is not accurate and can lead to complications due to under- and over-inflation. Implementation of an endotracheal tube cuff pressure management guideline was therefore needed in this context.
There are three steps to successful introduction of guidelines: development, dissemination, and implementation.[10] Successful implementation depends among other things on the use of evidence-based implementation strategies.[3] Implementation strategies enable practitioners to adopt and integrate guidelines and optimally implement and use them to inform and change their practice patterns in specific settings or healthcare institutions.[11]
There are various implementation strategies. Active strategies include educational outreach visits where the researcher meets the implementers face to face and explains what they should be doing, conferences, monitoring visits and champion leaders, while passive strategies include dissemination of guidelines, reminders, audit and feedback.[12] Strategies that are effective in facilitating guideline implementation, uptake and sustained use in practice in specific settings or healthcare institutions must be used. [13] For critical care contexts, it is recommended that multiple strategies be used to facilitate the implementation of guidelines, as they appear to be more effective than single strategies in this setting. Strategies commonly used in critical care contexts are printed educational material, information sessions, audit, feedback, use of champion leaders, educational outreach visits, and computer or internet use.[14,15] However, such strategies on their own may not be effective in achieving implementation. [16] In order to facilitate the implementation and uptake of guidelines into practice and enhance their sustained use, these implementation strategies should be tailored to address the unique needs of the context in which they are used, such as the ICU, and the preferences of the user of the guideline, in this case the critical care nurse.[12,17,18] Implementation strategies should therefore not just consider relevant theory and evidence, but also take into account stakeholder feedback.[19]
The objective of this study was to evaluate Malawian critical care nurses' views on the implementation of an endotracheal tube cuff pressure management guideline to enhance sustained guideline use.
Methods
Study design
An explorative-descriptive survey design was used. This article reports part of a larger, quasi-experimental pretest-post-test study aiming to improve nurses' knowledge with regard to managing endotracheal tube cuff pressure in ICUs, as described elsewhere.[14] The article focuses on evaluation of Malawian critical care nurses' views on the implementation of an endotracheal tube cuff pressure management guideline to enhance sustained guideline use, which was done in the post-test study.
Setting
Malawi is classified as a low- to middle-income country, with a population of ~18.6 million in 2019. Most of the country's population use public health services (hospitals and clinics).[20] During the study period (2016), Malawi had six functional ICUs in six hospitals (two private hospitals and four public central hospitals). The average bed capacity for private and public hospital IUCs was four, with the exception of one public hospital ICU that had six beds. Admissions numbered 20 - 30 per month, with almost 50% of these patients being mechanically ventilated. The setting can be considered resource constrained in terms of lack of qualified critical care nurses, as most nurses in both private and public hospitals had not undergone formal specialised intensive care nursing training.
Participants
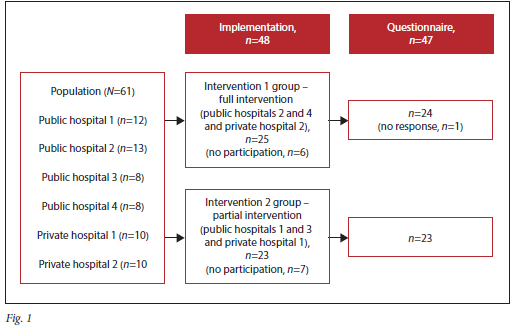
A convenience sample of all 61 nurses available in the six ICUs during the study period was randomised into two intervention groups. The names of one private and two public hospitals were randomly picked by an independent observer from two bowls containing the names of the private and public hospitals, respectively. The names of the first set of hospitals were then placed into an envelope and the second set of hospitals was put in another envelope. These envelopes were then placed in a basket. The first envelope chosen by the same independent observer was the group that would receive the full educational intervention (intervention 1 group), comprising both active (monitoring visits) and passive implementation strategies (a PowerPoint presentation, a printed version of the guideline, a printed and laminated summary of the guideline, and a related algorithm), while the group in the second envelope (intervention 2 group) received only passive implementation strategies. Two intervention groups were used instead of a control group, as pretest data from the larger study showed that knowledge among participants was generally very poor for both groups,[14] and the researcher felt ethically obliged to provide both groups with information on monitoring endotracheal cuff pressure in mechanically ventilated patients. A total of 47 nurses took part in the study, as 13 nurses declined to partake in the intervention (and therefore could not complete the questionnaire), and another one did not complete the questionnaire, as outlined in Fig. 1.
Data collection instrument
A structured, self-administered questionnaire was used, adopted from Jordan,[21] that measured critical nurses' management practices and their views regarding an endotracheal tube cuff pressure guideline for mechanically ventilated adults in South Africa (SA). The questionnaire had a good Cronbach's alpha score of 0.85 for reliability and internal consistency. It used closed- and open-ended questions, in two sections. Section A captured the participants' demographic data, i.e. age, gender, whether they had a formal intensive care qualification, years of work experience in intensive care, and the hospital at which they were employed. Section B comprised six questions: one closed-ended question regarding which implementation strategy was used in the ICU to implement the guideline (e.g. printed guideline and algorithm with monitoring visits by the researcher, or printed guideline and algorithm only), four questions (using 4 - 5-point Likert scales) that captured data regarding the implementation strategy's usefulness, clarity and applicability, and whether it enhanced guideline implementation ('Indicate how useful the implementation strategy was to you in implementing the clinical practice guideline for measuring endotracheal tube pressure'), and one final open-ended question that required the nurses to give their own recommendations for improved implementation, uptake and sustained use of guidelines in nursing practice ('What recommendations/suggestions would you put forward that would improve the implementation, uptake and sustained use of guidelines in practice?').
Data collection
The study was conducted in 2016, using a self-administered questionnaire after implementation of an educational intervention. The intervention was developed based on an evidence-based guideline for monitoring endotracheal cuff pressure in mechanically ventilated patients.[22] The guideline was selected because it was developed in the context of a low- to middle-income country, considering the resource constraints experienced in this context. The educational intervention included multiple implementation strategies, as this approach has been proven to enhance staff compliance with evidence-based interventions in the ICU setting,[15] and was reviewed by six purposefully selected ICU experts prior to its application to ensure alignment with the guideline, as well as contextualisation in terms of its feasibility given the available resources, and its relevance. Both intervention groups received passive implementation strategies, including a half-day educational session using a PowerPoint presentation of the contents of the guideline (definition of mechanical ventilation, indications for mechanical ventilation, complications of mechanical ventilation, management of endotracheal cuff pressure, endotracheal cuff pressure complications, and prevention of endotracheal cuff pressure complications), a printed version of the guideline, a printed and laminated summary of the guideline, and a related algorithm. In addition, an active implementation strategy comprising four monitoring visits over the 3-month period (April - June 2016) of guideline implementation was used in the intervention 1 group.[23]
The questionnaire was administered immediately after the 3-month implementation period. With permission from the hospital managers, a suitable date and time to visit the hospital for data collection was determined with each ICU manager. Tea breaks were used by the first author (FM) to provide a detailed explanation to each participant on day duty regarding the objectives of the study prior to their signing a consent form agreeing to participate. Those who agreed to participate were requested to complete the self-administered questionnaire. Immediately after completion of the questionnaire, which took ~15 minutes, the questionnaires were collected by the author. The author made appointments to meet nurses who were on night shifts, and the same process of data collection was followed. This was done for all the ICUs over a 2-month period (July - August 2016).
Data analysis
Completed questionnaires were checked and data were captured by author FM and analysed with the assistance of the fourth author (DV), a senior statistician, using Excel version 16.0 (Microsoft, USA). The quantitative data were analysed using descriptive (means, frequencies and standard deviations) and inferential analyses (t-test and x2 test to determine the relationship between variables). The Likert scale options for the scores of participants on the implementation strategies were merged into positive (strongly agree and agree), neutral (neutral) and negative (disagree and strongly disagree).
Qualitative data were analysed by authors FM and RMvR, using content analysis following the steps of coding by Tesch[24] as follows: the two authors, who had expertise in analysing qualitative data, independently read the captured answers and coded and categorised the codes, forming preliminary themes, followed by a consensus discussion. The consensus discussion allowed for comparisons of the categories and (sub)themes between both authors and resulted in the final themes and subthemes.
Ethical considerations
Ethical clearance was obtained from Nelson Mandela University, Gqeberha, SA (ref. no. H14-HEA-NUR-3) and the National Health Sciences Research Committee, Malawi (ref. no. 15/3/1397). Written permission was obtained from the six hospitals included in the study. Information about the study and the participants' rights (e.g. right to withdraw, voluntary participation) was provided to all study participants, and written informed consent was obtained prior to data collection. The questionnaire was anonymous, as it did not request any personal or identifiable data.
Results
Out of the 61 nurses approached, 47 agreed to participate in the study and completed the questionnaire, representing a response rate of 77%.
Demographic data
Table 1 outlines the demographic data of the participants in the two intervention groups, with the intervention 1 group receiving the full intervention with all implementation strategies, including the monitoring visits.
As outlined in Table 1, the average age of the participants was 26.4 years, with an average of 2.8 years of working experience in the ICU. Most participants were female (81%), had no formal intensive care qualification (85%), and were employed in public hospitals (68%). No statistically significant differences between the groups were noted with regard to demographic data.
Evaluation of the implementation strategies
Table 2 outlines the descriptive statistics on evaluation of the implementation strategies for the intervention 1 group (half-day educational session using a PowerPoint presentation, printed educational material, and monitoring visits) and the intervention 2 group (the same implementation strategies as for the intervention 1 group, but no monitoring visits) in terms of usefulness, clarity and applicability.
As shown in Table 2, most participants indicated that they agreed or strongly agreed that the implementation strategies were useful, clear and applicable and that they enhanced implementation of the guideline, although percentages of positive responses were generally higher for the intervention 1 group (full intervention) compared with the intervention 2 group (partial intervention).
Table 3 presents descriptive statistics by intervention group for the overall score measuring respondents' evaluation of the implementation strategies used, this being the average of the responses for the four items relating to usefulness, clarity, applicability and enhanced implementation of the guideline.
As shown in Table 3, most participants (87%) had a positive score (1.00 - 2.59) measuring their assessment of the implementation strategies. A larger proportion of those who received the full intervention (intervention 1 group) (92%) were positive about the implementation strategies compared with those who received the partial intervention (83%). The difference between the two groups was found not to be significant (X2(2)=0.87; p=0.649).
Table 4 reports inferential statistics for the mean score reflecting participants' assessment of the implementation strategies. It consists of two parts: (i) one-sample f-tests to determine whether it can be concluded, based on the sample data, that the mean population score regarding the implementation can be described as positive, i.e. µ<<2.6, the applicable threshold value for the Likert scale that was used (1 = very positive to 5 = very negative); and (ii) a f-test of independence to determine whether the mean for the intervention 1 group differs significantly from the mean for the intervention 2 group.
As seen in Table 4 (section 1), the overall mean and the means for each intervention group are all significantly (p<0.05; d>0.20) lower than the threshold value of 2.60 for the positive interval for the response that was used, and it can therefore be concluded that the corresponding mean scores for the sampled population can be regarded as positive. The results for the f-test of independence reflected in Table 4 indicate that the mean score difference between the two intervention groups is not significant (p=0.421).
Recommendations for implementation, uptake and sustained use of the guideline in nursing practice
Participants were required to provide recommendations or suggestions for implementation, uptake and sustained use of guidelines in nursing practice. The themes and subthemes that emerged are presented in Table 5, with relevant quotations. Note that only 38 of the 47 participants (81%) completed this item, and participants B25, B28 and B50 provided recommendations that could be categorised under more than one theme/ subtheme.
As outlined in Table 5, three main themes were identified, with the last theme having three subthemes related to recommendations related to the implementation, uptake and sustained use of guidelines in nursing practice. It was noted that participants mostly referred to the actual guideline for monitoring endotracheal tube cuff pressure in mechanically ventilated patients that was implemented, although some comments referred to the general implementation of guidelines in the ICU. Firstly, nurses recommended that the guideline should be translated, updated, and made available to ICU staff so that they could use it. Secondly, nurses
recommended continuous supervision (to a lesser extent, as this was only mentioned by participant B27) and follow-up post implementation of the guideline. The third and last theme was facilitating factors for successful implementation, related to: (i) education and training of ICU staff on the practical application of the content of the guideline; (ii) the need for resources to support the implementation of the guideline (manometers that assist in the monitoring of endotracheal cuff pressure were specifically mentioned by four participants); and (iii) commitment to best practices regarding endotracheal tube cuff pressure management.
Discussion
The objective of this study was to evaluate Malawian critical care nurses' views on implementation of an endotracheal tube cuff pressure management guideline to enhance sustained guideline use. The results revealed that the educational intervention based on the guideline was generally positively received by participants. The full intervention, including a half-day educational session using a PowerPoint presentation, a printed version of the guideline, a printed and laminated summary of the guideline and a related algorithm, together with monitoring visits, was generally positively received by the study participants. The partial intervention, using the same implementation strategies but without the monitoring visits, was also positively received, although with a slightly lower score with lesser significance compared with a higher score with a high degree of significance for the full intervention. Monitoring visits or outreach visits are part of a systematic approach that helps to implement and scale up evidence, but further exploration is required, as their effect on guideline adherence is not known.[25] Furthermore, a systematic review found that no single strategy or combination of strategies can be directly linked to successful implementation of nursing guidelines, which warrants a more systematic approach and reporting checklists with a detailed description of the implementation strategies.[26]
Demographic data in the present study were not significantly correlated with positive scores. However, the fact that the majority of the participants did not have a formal intensive care qualification may have posed challenges to the implementation of the guideline, which was confirmed by the need for education and training of ICU staff on the content of the guideline being most frequently indicated factor in terms of facilitating successful implementation. This finding is confirmed by a systematic review which concluded that education significantly improves the uptake of evidence, resulting in enhanced competence (knowledge and practice levels) among ICU nurses.[27] The young average age of our participants (26.4 years) linked with their low average of 2.8 years of working experience may also have posed challenges to the implementation of the guideline and could explain the need for more education and training on its content. Although there is no clear link between age, working experience and the implementation, uptake and sustained use of evidence, including guidelines, knowledge and practices were found to improve with each year's additional work experience of ICU nurses, which often translates into better adherence to practices recommended in guidelines.'[28]The present study showed the importance of the usefulness, clarity and applicability of strategies to enhance implementation of guidelines, together with identification of facilitating factors and barriers that need to be considered. Implementation of guidelines is important, as a growing body of literature demonstrates that due to various circumstances, a large proportion of critically ill patients in the ICU do not receive guideline-recommended care.[29] There are many difficulties in determining what strategies are most effective for the implementation, uptake and sustained use of guidelines in nursing practice.[30] Stakeholder feedback, which
in the present study was done by determining the strategies' usefulness, clarity, applicability and ability to enhance implementation of the guideline, can be used to develop tailored implementation strategies that address the unique contextual needs of an organisation.[19] Apart from stakeholder feedback, other contextual factors can be determined to develop tailored implementation strategies. These factors can be related to patients (e.g. alignment of the strategies with the patient's values, patient buy-in), providers (e.g. attitudes towards change and evidence-based practice), the organisation (e.g. how the organisational culture relates to evidence-based practice), and systems (e.g. policies and funding opportunities).[19] Furthermore, to enhance the use of effective tailored implementation strategies, Powell et al. '191 recommend that methods for designing and tailoring these strategies should be enhanced (e.g. through the use of intervention mapping - a stepwise approach to developing implementation strategies using a detailed and participatory needs assessment, with identification of implementation facilitators, behaviours and determinants), together with enhanced effectiveness research on multiple, tailored implementation strategies, economic evaluation of implementation strategies, and improved tracking and reporting of implementation strategies.
Identifying facilitating factors in the form of recommendations for uptake and sustained use of guidelines in nursing practice was also done in the present study through the open-ended question in the questionnaire. Firstly, our participants suggested that the guideline should be translated, updated, and made available to and used by ICU staff so that they could become familiar with it. Although a printed summary of the guideline was given to each ICU, the guideline may not have been sufficiently visible and accessible for the nurses to familiarise themselves with it. Open access to information has been proven to support healthcare professionals with knowledge to assist with patient management and enhance patient safety.[31,32] When nurses do not have access to or knowledge of specific guidelines, uptake is affected and they are unable to incorporate them into their daily practice.[31] Use of technology such as mobile phone applications should be encouraged to support nurses and enhance their access to guidelines, together with both electronic and hard-copy reminders.[32,33]
Secondly, implementation strategies such as continuous supervision, and follow-up post implementation, were recommended. Although author FM conducted four visits over a 3-month period to oversee
implementation of the guideline, as described by the Registered Nurses' Association of Ontario,[34] some participants expressed the opinion that these visits were not sufficient and that continuous supervision and follow-up is required. Although continuous supervision and follow-up has been recommended elsewhere to enhance guideline implementation in the ICU context, it requires a well-funded infrastructure,[35] which may pose a challenge in resource-constrained contexts such as Malawi.[36] Self-accountability is therefore important in this context, i.e. nurses need to be accountable for their practices and work environments and for patient safety, not only by upholding high clinical practice and ethical standards, but also by accepting professional responsibility when or if deviations from care standards occur.[37] Self-accountability can be fostered through improving clinical skills and knowledge as well as mentoring of novice nurses, among other things.[37] Furthermore, management should embrace a root-cause analysis approach to identifying system failures that result in bad practices and non-implementation and uptake of guidelines, rather than using a punitive approach.[37]
Thirdly, facilitating factors were identified to enhance the implementation and uptake of the guideline and its sustained use in practice. The need for education and training of ICU staff on practical application of the content of the guideline was highlighted. Ongoing education, training and clinical examinations on the practical application of learned content are proven implementation methods, and should be considered as cost-effective ways to enhance the implementation, uptake and sustained use of guidelines in the ICU context.[38] Furthermore, the need for resources to support the implementation of guidelines was mentioned. In most sub-Saharan African countries, including Malawi, shortages of both human and material resources are barriers to guideline implementation, uptake and sustained use.'361 This problem was evident from the findings of the present study. While the majority of the participants worked in public hospitals, which are often resource-constrained environments, the need for resources (in this context, aneroid manometers as the recommended method to assist in the management of endotracheal cuff pressure) to facilitate implementation was a factor mentioned by participants in private as well as public hospitals. Implementation should therefore be carefully planned, and strategies should consider the availability of resources and how a guideline could be implemented in a cost-effective way.[39]
Finally, commitment to best practices was recommended, which is crucial in successful implementation, uptake and sustained use of guidelines.[37] Commitment to best practices can be fostered using a number of strategies, such as involvement of the major key stakeholders, e.g. ICU staff, clinicians, and middle managers, through a 'change committee' that meets regularly; the use of champions to identify barriers and facilitators, provide support and drive the guideline's implementation, uptake and sustained use; and management support in providing the necessary time and resources.[40]
Study limitations
Because this was a doctoral study with a limited scope and timeframe that could not be extended, there were time constraints in following up on sustained use of the guideline after implementation. The study focused only on nurses, as the major bedside practitioners in the ICU and frequent users of the guideline. The limited sample, the brief questionnaire, the use of an open-ended question, the lack of necessary resources for some settings, and limited implementation strategies made it difficult to draw conclusions on the nurses' views on the implementation of the guideline. Furthermore, the context in terms of patient, provider and organisational factors influencing the success of implementation strategies was not considered in the study, but could have affected implementation and the preferred implementation strategies. The study should therefore be repeated, including a wider range of multiple implementation strategies and targeting other healthcare practitioners besides nurses, with careful planning, taking into consideration the resources required.
Conclusion
The study has highlighted that implementation of a guideline using multiple strategies such as printed educational material together with monitoring visits was positively received in terms of the strategies' usefulness, clarity, applicability, and ability to enhance implementation of the guideline. However, more consideration should be given to contextual (patient, provider and organisational) factors that could also have affected the success of implementation. Furthermore, recommendations for the uptake and sustained use of the guideline in nursing practice provided by our study participants, including the translation, updating and availability of the guideline, the need for continuous supervision, and for follow-up post implementation, and facilitating factors such as education and training on the practical application of the guideline's content, resources and commitment to best practices, should be kept in mind. Further study is required on how to ensure tailored implementation strategies that facilitate the implementation, uptake and sustained use of guidelines in resource-constrained contexts such as a Malawian ICU.
Declaration. None.
Acknowledgements. The authors thank Natalie Stear and Kegan Topper of Nelson Mandela University for editing the article, and the respondents for participating in the study.
Author contributions. FM: conception and design of the study, acquisition, analysis and interpretation of data, drafting the article, and final approval of the version to be submitted. RMvR, PJJ and DV: conception and design of the study, analysis and interpretation of data, revising the article critically for important intellectual content, and final approval of the version to be submitted. WtHB: conception and design of the study, analysis and interpretation of data, writing the article, and final approval of the version to be submitted.
Funding. None.
Conflicts of interest. None.
References
1. Bent S, Toschlog E. Reducing the risk for microaspiration and postintubation pulmonary complications in the surgical and critical care settings. Anesthesiology News, 2012. https://www.anesthesiologynews.com/download/SR1217_Covidien_WM.pdf (accessed 3 March 2022). [ Links ]
2. Jaillette E, Zerimech F, de Jonckheere J, et al. Efficiency of a pneumatic device in controlling cuff pressure of polyurethane-cuffed tracheal tubes: A randomised controlled study. BMC Anesthesiol 2013;13(1):50. https://doi.org/10.1186/1471-2253-13-50 [ Links ]
3. Fischer F, Lange K, Klose K, Greiner W, Kraemer A. Barriers and strategies in guideline implementation - a scoping review. Healthcare 2016;4(3):1-36. https://doi.org/10.3390/healthcare4030036 [ Links ]
4. Busse R, Klazinga N, Panteli D, Quentin W Improving healthcare quality in Europe: Characteristics, effectiveness and implementation of different strategies. World Health Organization Regional Office for Europe, 2019. https://apps.who.int/iris/handle/10665/327356 (accessed 22 February 2022). [ Links ]
5. Cairney P. The myth of 'evidence-based policymaking' in a decentred state. Public Policy Admin 2022;37(1):46-66. https://doi.org/10.1177/0952076720905016 [ Links ]
6. Jansson MM, Syrjala HP, Talman K, Merilainen MH, Ala-Kokko TI. Critical care nurses' knowledge of, adherence to, and barriers toward institution-specific ventilator bundle. Am J Infect Control 2018;46(9):1051-1056. https://doi.org/10.1177/0952076720905016 [ Links ]
7. Jansson M, Ala-Kokko T, Ylipalosaari P, Syrjala H, Kyngas H. Critical care nurses' knowledge of, adherence to and barriers towards evidence-based guidelines for the prevention of ventilator-associated pneumonia - a survey study. Intensive Crit Care Nurs 2013;29(4):216-227. https://doiorg/10.1016/j.iccn.2013.02.006 [ Links ]
8. Feng TR, Ye Y, Doyle DJ. Critical importance of tracheal tube cuff pressure management. World J Anesthesiol 2015;4(2):10-12. https://doi.org/10.5313/wja.v4.i2.10 [ Links ]
9. Rosero EB, Ozayar E, Eslava-Schmalbach J, Minhajuddin A, Joshi GP. Effects of increasing airway pressures on the pressure of the endotracheal tube cuff during pelvic laparoscopic surgery. Anesth Analg 2018;127(1):120-125. https://doi.org/10.1213/ANE.0000000000002657 [ Links ]
10. Eccles MP, Armstrong D, Baker R, et al. An implementation research agenda. Implement Sci 2009;4:18. https://doi.org/10.1186/1748-5908-4-18 [ Links ]
11. Leeman J, Birken SA, Powell BJ, Rohweder C, Shea CM. Beyond 'implementation strategies': Classifying the full range of strategies used in implementation science and practice. Implement Sci 2017;12(1):125. https://doi.org/10.1186/s13012-017-0657-x [ Links ]
12. Harrison MB, Legare F, Graham ID, Fervers B. Adapting clinical practice guidelines to local context and assessing barriers to their use. CMAJ 2010;182(2):E78-E84. https://doi.org/10.1503/cmaj.081232 [ Links ]
13. Pereira VC, Silva SN, Carvalho VK, Zanghelini F, Barreto JO. Strategies for the implementation of clinical practice guidelines in public health: An overview of systematic reviews. Health Res Policy Syst 2022;20(1):13. https://doi.org/10.1186/s12961-022-00815-4 [ Links ]
14. Jordan P, Mpasa F, ten Ham-Baloyi W, Bowers C. Implementation strategies for guidelines at ICUs: A systematic review. Int J Health Care Quality Assur 2017;30(4):358-372. https://doi.org/10.1108/IJHCQA-08-2016-0119 [ Links ]
15. Villarosa AR, Maneze D, Ramjan LM, Srinivas R, Camilleri M, George A. The effectiveness of guideline implementation strategies in the dental setting: A systematic review. Implement Sci 2019;14(1):106. https://doi.org/10.1186/s13012-019-0954-7 [ Links ]
16. McArthur C, Bai Y, Hewston P, Giangregorio L, Straus S, Papaioannou A. Barriers and facilitators to implementing evidence-based guidelines in long-term care: A qualitative evidence synthesis. Implement Sci 2021;16(1):70. https://doi.org/10.1186/s13012-021-01140-0 [ Links ]
17. Kwok EY, Moodie ST, Cunningham BJ, Cardy JE. Selecting and tailoring implementation interventions: A concept mapping approach. BMC Health Serv Res 2020;20(1):385. https://doi.org/10.1186/s12913-020-05270-x [ Links ]
18. Wang Z, Norris SL, Bero L. The advantages and limitations of guideline adaptation frameworks. Implement Sci 2018;13:72. https://doi.org/10.1186/s13012-018-0763-4 [ Links ]
19. Powell BJ, Beidas RS, Lewis CC, Aarons GA, McMillen JC, Proctor EK, Mandell DS. Methods to improve the selection and tailoring of implementation strategies. J Behav Health Serv Res 2017;44(2):177-194. https://doi.org/10.1007/s11414-015-9475-6 [ Links ]
20. World Bank. Malawi overview. https://www.worldbank.org/en/country/malawi/overview#1. 2022 (accessed 1 March 2022). [ Links ]
21. Jordan PJ. Evidence-informed clinical guidelines for nursing care practices related to the safety of the mechanically ventilated patient. PhD thesis. Nelson Mandela Metropolitan University, Port Elizabeth, South Africa, 2011. [ Links ]
22. Jordan P, Bowers C, Morton D. Barriers to implementing evidence-based practice in a private intensive care unit in the Eastern Cape. South Afr J Crit Care 2016;32(2):50-54. https://doi.org/10.7196/SAJCC.2016.v32i2.253 [ Links ]
23. Mpasa F. Management of endotracheal tube cuff pressure in mechanically ventilated adult patients in intensive care units in Malawi. Unpublished PhD thesis. Nelson Mandela University, Port Elizabeth, South Africa, 2017. [ Links ]
24. Tesch R. Qualitative Research: Analysis Types and Software Tools. London: Elsevier, 1990. [ Links ]
25. Reynolds SS. Implementation strategies to improve critical care nurses' knowledge of and adherence to evidence-based guidelines. PhD thesis. Indiana University-Purdue University Indianapolis, 2016. https://doi.org/10.7912/C2/1285 [ Links ]
26. Spoon D, Rietbergen T, Huis A, et al. Implementation strategies used to implement nursing guidelines in daily practice: A systematic review. Int J Nurs Stud 2020;111:103748. https://doi.org/10.1016/j.ijnuretu.2020.103748 [ Links ]
27. Almarhabi M, Cornish J, Lee G. The effectiveness of educational interventions on trauma intensive care unit nurses' competence: A systematic review and meta-analysis. Intensive Crit Care Nurs 2021;64:102931. https://doi.org/10.1016/j.iccn.2020.102931 [ Links ]
28. Khojastehfar S, Ghezeljeh TN, Haghani S. Factors related to knowledge, attitude, and practice of nurses in intensive care unit in the area of pressure ulcer prevention: A multicenter study. J Tissue Viability 2020;29(2):76-81. https://doi.org/10.1016/j.jtv.2020.02.002 [ Links ]
29. Kahn JM. Bringing implementation science to the intensive care unit. Curr Opin Crit Care 2017;23(5):398-399. https://doi.org/10.1097/MCC.0000000000000446 [ Links ]
30. Reynolds HW, Sutherland EG. A systematic approach to the planning, implementation, monitoring, and evaluation of integrated health services. BMC Health Serv Res 2013;13:168. https://doiorg/10.1186/1472-6963-13-168 [ Links ]
31. Alotaibi YK, Federico F. The impact of health information technology on patient safety. Saudi Med J 2017;38(12):1173-1180. https://doi.org/10.15537/smj.2017.12.20631 [ Links ]
32. Keyworth C, Hart J, Armitage CJ, Tully MP. What maximises the effectiveness and implementation of technology-based interventions to support healthcare professional practice? A systematic literature review. BMC Med Inform Decis Mak 2018;18(1):93. https://doi.org/10.1186/s12911-018-0661-3 [ Links ]
33. Jun J, Kovner CT, Stimpfel AW. Barriers and facilitators of nurses' use of clinical practice guidelines: An integrative review. Int J Nurs Stud 2016;60:54-68. https://doi.org/10.1016/j.ijnurstu.2016.03.006 [ Links ]
34. Bajnok I, McConnell H, Grinspun D, Stewart-Pyne A. An evidence-based approach to successful practice change, the Toolkit: Implementation of best practice guidelines. https://sigma.nursingrepository.org/bitstream/handle/10755/335652/Slides.pdf?sequence=1&isAllowed=y (accessed 6 March 2023). [ Links ]
35. Joint Professional Standards Committee. Guidelines for the provision of intensive care services. https://www.rcslt.org/wp-content/uploads/media/docs/clinical-guidance/critical-care-gpics-v2.pdf 2019 (accessed 15 July 2022). [ Links ]
36. Docherty M, Shaw K, Goulding L, et al. Evidence-based guideline implementation in low and middle income countries: Lessons for mental health care. Int J Mental Health Syst 2017;11:8. https://doi.org/10.1186/s13033-016-0115-1 [ Links ]
37. Spears TL, Allen L. Evidence-based care sheet: Accountability in nursing practice. 6 April 2018. https://www.ebscohost.com/assets-sample-content/NRCP_EBCS_Accountability-in-NursingPractice.pdf (accessed 6 March 2023). [ Links ]
38. Rosa RG, Teixeira C, Sjoding M. Novel approaches to facilitate the implementation of guidelines in the ICU. J Crit Care 2020;60:1-5. https://doi.org/10.1016/j.jcrc.2020.07.014 [ Links ]
39. Grol R, Wensing M. Effective implementation of change in healthcare: A systematic approach. In: Wensing M, Grol R, Grimshaw J, eds. Improving Patient Care: The Implementation of Change in Health Care. Pondicherry, India: John Wiley & Sons, 2020. [ Links ]
40. Webb-Anderson K, Daley P, Isenor C, Kelly E, Ash M, McMullen S. Supporting critical care best practice with an integrated approach to quality improvement. Can J Crit Care Nurs 2018;29(2):44. https://cjccn.ca/wp-content/uploads/2022/02/29-2-CJCCNSummer2018.pdf (accessed 6 March 2023). [ Links ]
 Correspondence:
Correspondence:
W ten Ham-Baloyi
wilma.tenham-baloyi@mandela.ac.za
Accepted 9 February 2023














