Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
Southern African Journal of Critical Care (Online)
versão On-line ISSN 2078-676X
versão impressa ISSN 1562-8264
South. Afr. j. crit. care (Online) vol.38 no.2 Pretoria Jul. 2022
http://dx.doi.org/10.7196/SAJCC.2022.v38i2.535
ARTICLE
A mixed-methods study on evaluating an updated, francophone version of ETAT+ training in Madagascar
M GalatschI, VIII; H-J LangI; C NoaII, III; Η RavelohariminoIV, V; A RobinsonVI, VII; H RabesandratanaII, IV; L I MageraVIII; R WeigelI; D Köcher-AndrianarimananaIV, IX
IPhD Friede Springer-endowed professorship for Global Child Health, Faculty of Health, School of Human Medicine, Witten/Herdecke University, Witten, Germany
IIMD; Faculté de Médecine, Université de Mahajanga, Madagascar
IIIMD; Association TSIKY, Mahajanga, Madagascar
IVMD ; Faculté de Médecine, Université de Mahajanga, Madagascar
VMD ; Faculté de Médecine, Université d'Antananarivo, Madagascar
VIMD; Faculté de Médecine, Université d'Antananarivo, Madagascar
VIIMD; Management Sciences for Health, USAID ACCESS Program, Antananarivo, Madagascar
VIIIPhD Institute of Nursing, School of Health Science, Zurich University of Applied Science, Winterthur, Switzerland
IXMPH;Institute of Nursing, School of Health Science, Zurich University of Applied Science, Winterthur, Switzerland
ABSTRACT
BACKGROUND. Madagascar needs major efforts to achieve the UN Sustainable Development Goals, despite the considerable reduction of child mortality during past years. In this context, implementation of emergency triage assessment and treatment (ETAT) plays an important role. In recent years, ETAT training activities rarely took place in Madagascar. To strengthen ETAT in Madagascar, a pilot training course was conducted in December 2019 at the University Hospital Mahajanga.
OBJECTIVE. This study aims to evaluate if the ETAT+ pilot training content matches clinical needs in Madagascar and whether participants achieved their learning objectives.
METHODS. In this cross-sectional mixed-methods study, a 41-item questionnaire was used at the end of the ETAT+ training to evaluate their learning experience from the 12 participants (paediatricians, physicians, nurses and midwives). Six weeks after the training, guided interviews were conducted among five participants to describe how training content could be transferred into clinical practice in five health facilities.
RESULTS. Results suggest that this pilot project designed to contribute to the re-establishment of ETAT in Madagascar meets participants' needs and is adapted to clinical realities in terms of transmitted knowledge, skills and competencies. However, results also show that considerable multi-disciplinary efforts are needed to advance ETAT+ implementation in Madagascar.
CONCLUSIONS. Implementation processes of ETAT training programmes need re-evaluation to assure their validity to contribute to quality of care improvements efficiently. Further operational research is required to evaluate sustainable, innovative implementation strategies adapted to contexts in Madagascar.
Keywords: Emergency triage assessment and treatment (ETAT) training; essential emergency and critical care (EECC).
The under-five mortality rate (U5MR) in Madagascar is still high despite a considerable reduction within the last three decades from 157 to 51 per 1 000 live births.[1] Additionally, morbidity and mortality in the age group of 5 - 14 years and among adolescents need to be tackled in efforts to improve child health.[1] Most deaths among children and adolescents are either preventable and/or treatable.[1,2] Socio-economic and political determinants, as well as public health interventions, have significant impact on child health.[1-5]
Many deaths among children, especially in resource-limited settings, are due to severe infections; e.g. respiratory infections, severe malaria, and diarrhoeal diseases.[6,7] Malnutrition increases the risk of developing critical illness, and ~45% of deaths in U5 children are associated with undernutrition.[7,8] Additionally, human immunodeficiency virus (HIV), infections and tuberculosis (TB) substantially contribute to morbidity and mortality among children and adolescents.[9,10]
Without early efficient management, serious infections can progress to severe multi-organ dysfunction. This process can be defined as sepsis and is not necessarily documented as a distinct entity in Global Burden of Disease estimates.[6,11] A considerable number of children who survive critical illness (e.g. cerebral malaria) suffer subsequently from life-long disabilities.[12] Access to essential paediatric emergency and critical care (EPECC) can contribute to a reduction of mortality and also of preventable disability.[12,13] To improve access to EPECC, referral pathways from communities and peripheral health facilities to district or regional hospitals need to be strengthened.[14-16] However, access to adequate hospital-based emergency and critical care is challenging for many populations in sub-Saharan Africa (SSA).[15]
At health facility level, it has been shown that implementing efficient patient circuits and essential paediatric emergency care services can have a considerable impact on paediatric hospital mortality.[17] In this context, the World Health Organization (WHO) produced guidelines and training modules for emergency triage assessment and treatment (ETAT) targeting care of children managed at hospital level.[18,19] ETAT guidelines follow international emergency care algorithms (e.g. advanced paediatric life support (APLS)),[20] but are not designed to cover the whole spectrum of competencies needed to treat critically ill children at hospital level. Based on WHO guidelines, levels of paediatric emergency and critical care can be adapted to available resources, workload and skill levels of clinical teams.
In previous years, ETAT training activities rarely took place in Madagascar. To revive ETAT in Madagascar, a multidisciplinary team from the University Hospital Mahajanga (Chu PZaGa), the WHO, the Management Sciences for Health (MSH)/USAID Accessible Continuum of Care and Essential Services Sustained (ACCESS) project, Madagascar and Witten/Herdecke University conducted an ETAT+ pilot training course in December 2019 at Chu PZaGa. The present article describes the preparation process and delivery of this training activity. The study uses a mixed-methods design to examine whether the ETAT+ pilot training met the clinical needs of participants and whether participants met their learning objectives.
Methods
ETAT+ training (adapted Malagasy version)
The training content is based on the ETAT+ training curriculum outlined by the Royal College of Paediatrics and Child Health (RCPCH)[21] and management algorithms defined by the WHO in their Pocket Book of Hospital Care for Children.[ls,19] These materials have been evaluated and successfully used in several low-resource contexts.[17] The process to develop an ETAT+ training version adapted to clinical realities in Madagascar (Fig. 1) was endorsed by the Société Malgache de Pediatrie (SOMAPED), the CHU PZaGa Mahajanga and the Ministry of Health. In a multi-step process led by Malagasy partners, training contents, teaching methods and course organisation were adapted to the anticipated training needs of inter-professional course participants. This process was finalised in a 5-day preparation workshop in Mahajanga.
Design of the evaluation process
A mixed-method design was applied for this evaluation.[22] The mix of methods refers to the combination and integration of quantitative and qualitative methods. This approach is well adapted for complex evaluations in comparison with purely qualitative or quantitative approaches.[23] The evaluation of the present study uses a sequentially explanatory mixed-methods design. The initial quantitative results and interpretations are strengthened by subsequent interviews conducted six weeks after the initial pilot training.[23]
Sample
Twelve Malagasy health professionals (paediatricians, physicians, nurses and midwives) from six health facilities situated in four different regions of Madagascar attended a five-day ETAT+ training course in December 2019 in Mahajanga. Participating health workers practised in paediatric and emergency departments on different health system levels.
Data collection
In the quantitative part, data were collected at the end of the training using a paper-and-pencil self-administered questionnaire. All 12 participants gave informed consent. Additionally, participants were asked whether they would be available for a telephone interview six weeks after the 5-day training to evaluate their experience in the practical application of the ETAT training content in their respective health facilities. All 12 participants consented to the interviews. Subsequently, five participants were selected randomly for interviews.
Questionnaire
In the questionnaire, eight dimensions (reading materials, engagement, critical thinking, collaborative working, overall experience, training delivery, role as trainer and training content) were used to evaluate the training's learning success. The questionnaire was based on structures frequently used and assessed in different training contexts.[24] For use in this ETAT+ training evaluation, questions were adapted and some training-specific questions were added (Annex 2). The questionnaire consisted of 37 closed questions and four free-text options (completion time about 15 - 20 minutes) in the French language. For the quantitative data, descriptive responses to each item were shown.
Interviews
Five guided interviews were conducted six weeks after the training (January 2020). The objective of these interviews was to evaluate the potential role of ETAT+ principles in the respective health facilities and to identify opportunities and challenges to implement or improve processes of essential paediatric emergency and critical care using ETAT+ management algorithms. Owing to the significant geographical distance of the participants, interviews were carried out by telephone and were recorded via a digital recording device. Interviews were conducted by a Malagasy project member in French. Subsequently, interview results were anonymised and transcribed. Content analysis followed the procedures described by Mayring.[25]
Translation
All materials used in the study were reviewed in a standard forward-and-backward translation process with monolingual and bilingual tests.[26] This approach allows study information, informed consent, questionnaire and guided questions translated from English to French. The evaluation free-text answers and interview transcripts were translated from French to English using the same method.
Results
Descriptive profile participants
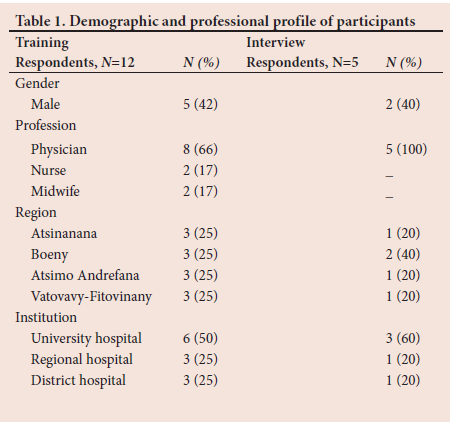
The demographic and professional characteristics of participants (N=12) are shown in Table 1. More than half of the participants were female (58%) and were physicians (66%). The participants came from four different regions of Madagascar and six different health facilities. Three participants from each region attended the training. Most of the participants worked in university hospitals (50%); others came from regional hospitals (25%) and district hospitals (25%).
Quantitative evaluation
Questionnaire results are shown in Table 2. Participants described training content, training methods and course organisation as highly relevant to Madagascar's clinical realities and felt motivated and encouraged to engage in the training process.
Pre-course reading material
Five of the 12 participants stated that they studied pre-course reading materials which were provided online. Participants' feedback on content, relevance and structure of pre-course reading materials was positive (75% positive answers). However, 42% of participants stated that pre-course study time was limited owing to late provision of reading materials.
Engagement
Nevertheless, half of the participants (50%) felt well-prepared for the training. The interactive design of the training and opportunities to contribute during training sessions actively were rated positively. Eighty-four percent of participants stated that they asked questions during the training. However, only 58% said they discussed their actual personal training performance with facilitators during the training.
Critical thinking
Participants engaged with a positive attitude in the learning process and indicated that the training helped them to develop new ideas or new understanding (100%). Additionally, 83% of participants stated that the training experience exposed them to previously unknown or poorly understood management approaches of severely ill children.
Collaborative working
During the training, participants experienced numerous opportunities to interact and discuss with other participants. Eighty-three percent of participants reported that they worked together during the teaching course sessions and discussed each other's training experiences as well as specific clinical topics. Outside the training sessions during the 5-day course, training experiences were less frequently discussed with other participants (42%).
Overall experience
The general feedback on the training was consistently positive. All participants (100%) rated the training as interesting, stating that it challenged them to recall their best performance and achieve their learning objectives.
Training delivery
All participants (100%) rated the course content as up-to-date and relevant for their work. Equally positive (100%) was the rating for clarity of the presentation of learning objectives as well as the illustration of course content. Additionally, the set-up of the course and the use of multiple training methods was evaluated positively. Using different training methods benefited the learning process. Some participants (33%) stated that the 5-day training course was too short to transmit the training content comprehensively.
Role as trainer
After the training, all participants felt capable of providing teaching of certain elements of the ETAT+ course in their facilities. Participants also felt able to identify essential training needs in the care of critically ill children in their respective hospitals. Furthermore, all participants (100%) stated that a refresher course would have the potential to benefit their clinical skills as well as their capacity to function as a trainer. Some participants perceived the implementation process of ETAT+ in their institutions as a considerable challenge. Only 42% could imagine a rapid and comprehensive introduction of ETAT+ management principles in their institution at this stage.
Training content
According to participants, the training did not include irrelevant content (100%), nor were there any essential topics missing (100%). The participants indicated the following training topics as most relevant for their routine clinical practice (Fig. 2). The structured 'ABCDE-approach' to a critically ill child was described as the most relevant content (n=11), followed by 'management of shock and fluid-resuscitation (n=5)', 'the triage process and identification of the critically ill child' as well as 'the practice to gain intra-osseous access' (both n=4).
Interview findings
In the qualitative content analysis, the content of the interviews was conceptualised into six categories: 'ETAT+ training content', 'qualification of course participants to apply learned knowledge, skills and competencies', 'qualification of participants to act as trainers and transfer ETAT+ training content', 'motivation of course participants to practise learned skills and competencies and to act as trainer', 'conditions and requirements needed for ETAT+ implementation' and 'general challenges in daily clinical reality and the implementation of ETAT+ principles'.
ETAT training content
Participants emphasised different elements of the training content, which were particularly challenging to practise as an individual clinician, and which were also difficult to introduce in routine clinical practice. One participant described the difficulties as follows:
"The intraosseous access ... the subject on the intraosseous access is a theme that I do not sufficiently master and that I still hesitate to put into practice... it is true that we practised on chicken bone in Mahajanga during the training, but we had no direct practice on a human being." (Interview no. 1 en: 16 - 16)
In this context, both lack of appropriate practical experience and lack of equipment, as well as adequate set-up of the clinical environment, were elements seen as challenges in implementing training content. This example highlights the importance of clinical mentoring by experienced paediatric critical care clinicians in the trainee's clinical environment. Additionally, participants stated that equipment, supply processes and the set-up of clinical environments needed to be adapted.
In the implementation of specific clinical interventions lack of adequate equipment and logistic set-up of health facilities were highlighted as particular challenges:
"...the resuscitation phase requires the use of oxygen... but in the case of our institution, we have no source of oxygen... only the CHU of Tuléar around here has a working oxygen extractor... The training is undoubtedly feasible and relatively simple even... but it is the practical implementation, which is problematic..." (Interview no. 2 en: 22 - 22)
However, all participants agreed that the content of the training was beneficial for their daily clinical practice. Rapid identification of the critically ill child and focusing on essential priorities in the structured approach to stabilising vital organ function in their opinion is crucial to the ETAT+ training. This approach was considered as a beneficial concept, which can be directly translated into clinical practice.
Qualifications
When asked to rate their qualifications as trainers in general and their clinical competencies, participants indicated that they felt qualified and confident in aspects of essential paediatric emergency and critical care. However, we need to emphasise that clinical performance and training skills were not directly evaluated in the participants' clinical setting. The interest and need for ETAT+ training of clinical staff in the respective health facilities are described as high by the interview participants.
Motivation
The motivation of interview participants and clinical staff at the health facilities was repeatedly emphasised during interviews and described as exceptionally high, both for training activities and for daily clinical work.
Content transfer
In general, interview participants did not see their skills as trainers as a problem but rather the practical implementation of continuous training programmes in their respective health facilities.
A further challenge for the mostly young participants was to convey content to experienced or hierarchically higher-ranking colleagues:
"The second challenge, which I also face, is the fact that I have to train personnel... let's say, more competent or even qualified than me... It is a great challenge for me to play the trainer's role towards my superiors." (Interview no. 2: 30 - 30)
ETAT implementation conditions
Participants gained further skills and knowledge and developed additional competencies. However, the results of the interviews emphasise considerable challenges, which need to be addressed in the process of implementing ETAT in health facilities. These challenges were related to structural and organisational priorities and clinical equipment. Here, the interview participants considered support from health facility administrators in particular, but also external groups such as NGOs, as very important.
Furthermore, the importance of personal effort and motivation was also pointed out. Thus, the interview participants saw sufficient payment of health workers and on-the-job training, as well as training outside the institution, as important factors for successful implementation of a 'Madagascar's ETAT+ version'.
Discussion
The Malagasy ETAT+ pilot training can contribute to a process leading to the establishment of an ETAT+ programme adapted to regional clinical realities. Course evaluation results indicate that the design and delivery of ETAT+ training by a multidisciplinary team meets the needs of participants. Directly after the 5-day course, participants were highly motivated and able to describe plans to implement ETAT+ contents in their respective health facilities. Results of interviews conducted among five-course participants six weeks after the initial training suggest that this level of motivation could be maintained. In several resource-limited settings, ETAT+ training has been adapted to match specific contexts while maintaining essential elements of paediatric emergency and critical care as outlined in WHO guidelines.[27-30] Implementing ETAT principles can contribute to a substantial reduction of paediatric hospital mortality in resource-limited settings.[17,28-31]
Results of this evaluation suggest that perceptions of learning experiences and training methods were similar among health professionals with different clinical backgrounds such as general practitioners, nurses and midwives. However, results also indicate that certain elements in the preparation and delivery of ETAT+ training need to be adapted (e.g. earlier and better access to pre-course learning materials). In the future, efforts can be undertaken to develop an online learning platform providing learning materials in French. Furthermore, the pace of delivery of the training content needs to be tailored to different levels of knowledge, skills and competencies of participants. This aspect highlights a major limitation of ETAT+ 'short courses' running over a few days: that this training format can only introduce essential elements of ETAT+ but is certainly not sufficient to develop comprehensive clinical competencies.
Interview results demonstrate important challenges of participants to implement ETAT+ principles in their health facilities. While participants largely retained essential knowledge of training course content, evaluation results revealed challenges in practice of particular procedures (e.g. insertion of intraosseous access) or managing complex critical scenarios independently without senior support. These results suggest that the initial introduction of training content needs to be followed by mentoring periods assisted by experienced training teams in clinical settings.[32] The use of log-books (paper or app) can guide an individual comprehensive learning process. On-the-job training periods can be coupled with online mentoring activities supporting self-directed and peer group learning activities.[33] Additionally, the training format of short courses is not sufficient to develop competencies necessary for performing as an ETAT+ instructor. Short courses can help to identify participants with instructor potential. Following existing models of instructor training processes,[34] an instructor training and support strategy needs to be developed in order to implement ETAT+ in low-resource settings. This strategy should include efforts to clarify the role of ETAT+ trainers within the human resource systems of health facilities to effectively contribute to quality improvement in essential paediatric emergency and critical care.[35,36]
Participants identified further challenges in implementing ETAT+. Firstly, patient circuits need to be optimised in health facilities to improve triage and access to immediate emergency care.[17,31] Additionally, essential equipment, consumables and medication need to be provided to efficiently treat critically ill patients (e.g. O2-concentrators, intraosseous needles, paediatric infusion sets). To safely run biomedical equipment, reliable electricity systems are essential.[37,38] Context-adapted biomedical equipment needs to be available, and efficient repair and maintenance systems must be developed.[39-
This discussion underlines the importance of a multidisciplinary approach to ETAT+ implementation. The process includes clinical expertise, training programmes, human resource management, logistical and biomedical engineering support, and functioning supply chains.[36,40,41]
Before the training, different stakeholders conducted a preparation workshop to define content and training methods of the ETAT+ pilot training. WHO management guidelines for hospital care of children provided the core elements of the ETAT+ training.[18,19] Additional topics important to practitioners in Madagascar were highlighted (Fig. 1), e.g. the particular importance of essential newborn hospital care was expressed as well as the introduction of basic non-invasive respiratory support (e.g., bubble continuous positive airway pressure (CPAP), further context-adapted critical care after initial stabilisation of vital organ functions and an introduction to essential trauma care and burns management. Additional important topics were identified which could not be included in the initial ETAT+ pilot training, e.g., management of obstetric emergencies as part of adolescent care, and treatment of complications associated with certain non-communicable diseases (e.g. sickle cell disease, diabetic ketoacidosis). In the future, also, dengue virus infections and other outbreak diseases need to be considered.
In addition, training methods were defined during the preparation workshop for the ETAT+ pilot training, while realising that further continuous medical education programmes need to be introduced in the different regions of Madagascar (Supplementary files 1 and 2).
A process ensuring regular review of training content, emerging evidence, and efficiency of training methods, needs to be established[42,43] This process needs to be led by SOMAPED as well as national training institutions. In this context, further research is required to find sustainable solutions for the implementation of training programmes in essential paediatric emergency and critical care in Madagascar.[36,44,45] This process must take into account the different levels of care available at various levels of referral pathways.[35] In addition to ETAT+ training programmes, it may be beneficial to develop a further training module covering more advanced levels of paediatric critical care (Fig. 1).
Study limitations
To our knowledge, this is the first study to evaluate ETAT+ training activities in Madagascar in the last decade. In addition, the study describes factors influencing implementation and scaling-up of ETAT+ guidelines in Madagascar.
Several limitations associated with this study need to be considered. The sample size of the study was small. Furthermore, associated with the paper-based survey with self-reporting, the nature of the data collection may have influenced the responses of participants. In addition, biases may have occurred in the transmission or translation of data. During the ETAT+ pilot training, practical skills, knowledge and clinical competencies, as well as communication skills, were reviewed continuously by instructors. However, this evaluation process can be strengthened by sequential evaluation of clinical simulations exercises[34,46,47]
Challenges and opportunities associated with the implementation of ETAT management principles were assessed by telephone interviews. Multidisciplinary on-site evaluations may be of greater value to contribute to implementation processes aiming to improve essential paediatric emergency and critical care in health facilities.[36]
Conclusion
Implementation of ETAT+ could have the potential to substantially improve paediatric hospital care in resource-limited settings. This study highlights that training programmes in essential paediatric emergency and critical care need re-evaluation to ensure efficient contribution to quality-of-care improvements. Further operational research is needed to evaluate sustainable, innovative implementation strategies adapted to clinical realities in Madagascar.
Declaration. None.
Acknowledgements. We would like to thank the teams from Management Sciences for Health (MSH), USAID ACCESS Project Madagascar and the WHO office in Madagascar, who were crucial in organising the ETAT+ training evaluated in this article.
Author contributions. MG, RW, DKA: conceptualisation; MG, HJL, CN: data curation; MG: formal analysis; RW, MG: methodology; MG: visualisation, project administration; MG, HJL: equal contribution authors, wrote original draft; MG, HJL, CN, HR, AR, NR, LIM, RW, DKA: writing, reviewing, editing.
Funding. This study was supported by the Friede Springer-endowed professorship for Global Child Health.
Conflicts of interest. None.
References
1. UN/Inter-Agency-Group. Levels & Trends Child Mortality; Report 2020: UN Inter-agency Group for Child Mortality Estimation 2020. https://childmortality.org/reports (accessed 2 May 2022). [ Links ]
2. United Nations. Sustainable development goals (SDH) - United Nations 2015. https://www.un.org/sustainabledevelopment/ (accessed 2 May 2022). [ Links ]
3. O'Hare B, Makuta I, Chiwaula L, Bar-Zeev N. Income and child mortality in developing countries: A systematic review and meta-analysis. J R Soc Med 2013;106(10):408-414. https://doi.org/10.1177/0141076813489680 [ Links ]
4. Burstein R, Henry NJ, Collison ML, et al. Mapping 123 million neonatal, infant and child deaths between 2000 and 2017. Nature 2019;574(7778):353-358. https://doi.org/10.1038/s41586-019-1545-0 [ Links ]
5. UNICEF. Campaign: Children Under Attack 2021. https://www.unicef.org/children-under-attack (accessed 2 May 2022). [ Links ]
6. Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: Analysis for the Global Burden of Disease Study. Lancet 2020;395(10219):200-211. https://doi.org/10.1016/s0140-6736(19)32989-7 [ Links ]
7. UNICEF. Inter-agency Group for Child Mortality Estimation (UN IGME), Levels & Trends in Child Mortality: Report 2020, Estimates developed by the United Nations Inter-agency Group for Child Mortality Estimation. New York: United Nations Children's Fund; 2020. [ Links ]
8. World Health Organization. Fact sheet Malnutrition. New York: WHO; 2021. https://www.who.int/news-room/fact-sheets/detail/malnutrition. [ Links ]
9. World Health Organization. Fact sheet HIV/AIDS. New York: WHO; 2021. https://www.who.int/news-room/fact-sheets/detail/hiv-aids. [ Links ]
10. World Health Organization. Fact sheet Tuberculosis. New York: WHO; 2021. https://www.who.int/news-room/fact-sheets/detail/tuberculosis. [ Links ]
11. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392(10159):1736-1788. https://doi.org/10.1016/S0140-6736(18)32203-7 [ Links ]
12. Birbeck GL, Molyneux ME, Kaplan PW, et al. Blantyre Malaria Project Epilepsy Study (BMPES) of neurological outcomes in retinopathy-positive paediatric cerebral malaria survivors: A prospective cohort study. Lancet Neurol 2010;9(12):1173-1181. https://doi.org/10.1016/s1474-4422(10)70270-2 [ Links ]
13. Razzak J, Usmani MF, Bhutta ZA. Global, regional and national burden of emergency medical diseases using specific emergency disease indicators: Analysis of the 2015 Global Burden of Disease Study. BMJ Global Health 2019;4(2):e000733. https://doi.org/10.1136/bmjgh-2018-000733 [ Links ]
14. World Health Organization. Hospitals 2020. New York: WHO; 2020. https://www.who.int/health-topics/hospitals#tab=tab_1 (accessed 2 May 2022). [ Links ]
15. Ouma PO, Maina J, Thuranira PN, et al. Access to emergency hospital care provided by the public sector in sub-Saharan Africa in 2015: A geocoded inventory and spatial analysis. Lancet Glob Health 2018;6(3):e342-e350. https://doi.org/10.1016/s2214-109x(17)30488-6 [ Links ]
16. Hodkinson P, Argent A, Wallis L, et al. Pathways to care for critically ill or injured children: A cohort study from first presentation to healthcare services through to admission to intensive care or death. PLoS One 2016;11(1):e0145473. https://doi.org/10.1371%2Fjournal.pone.0145473 [ Links ]
17. Molyneux EM. Paediatric emergency care in resource-constrained health services is usually neglected: time for change. Ann Trop Paediatr 2010;30(3):165-176. https://doi.org/10.1179/146532810x12703902516482 [ Links ]
18. World Health Organization. Pocket book of hospital care for children : Guidelines for the management of common childhood illnesses 2013. New York: WHO; 2013. [ Links ]
19. World Health Organization. Guideline: Updates on paediatric emergency triage, assessment and treatment: Care of critically-ill children. New York: WHO; 2016. https://apps.who.int/iris/bitstream/handle/10665/204463/9789241510219_eng.pdf?sequence=1 (accessed 2 May 2022). [ Links ]
20. Samuels M, Wieteska S. Advanced Paediatric Life Support. Chichester: John Wiley & Sons; 2016. [ Links ]
21. RCPCH. Emergency triage, assessment and treatment plus (ETAT+) - online learning 2021. https://www.rcpch.ac.uk/resources/emergency-triage-assessment-treatment-plus-etat-online-learning (accessed 2 May 2022). [ Links ]
22. Klassen AC, Creswell J, Plano Clark VL, Smith KC, Meissner HI. Best practices in mixed methods for quality of life research. Qual Life Res 2012;21(3):377-380. https://doi.org/10.1007/s11136-012-0122-x [ Links ]
23. Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. Aust NZ J Publ Health 2007;31(4):388. [ Links ]
24. Trowler V. Student engagement literature review. York: The Higher Education Academy; 2010. [ Links ]
25. Mayring P. Qualitative Inhaltsanalyse, grundlagen und techniken. Weinheim: Beltz; 2015. [ Links ]
26. Maneesriwongul W, Dixon JK. Instrument translation process: A methods review. J Adv Nurs 2004;48(2):175-186. https://doi.org/10.1111/j.1365-2648.2004.03185.x [ Links ]
27. Hategeka C, Mwai L, Tuyisenge L. Implementing the emergency triage, assessment and treatment plus admission care (ETAT+) clinical practice guidelines to improve quality of hospital care in Rwandan district hospitals: Healthcare workers' perspectives on relevance and challenges. BMC Health Serv Res 2017;17(1):256. https://doi.org/10.1186/s12913-017-2193-4 [ Links ]
28. Hands S, Verriotis M, Mustapha A, Ragab H, Hands C. Nurse-led implementation of ETAT+ is associated with reduced mortality in a children's hospital in Freetown, Sierra Leone. Paediatr Int Child Health 2020;40(3):186-193. https://doi.org/10.1080/20469047.2020.1713610 [ Links ]
29. Crouse HL, Torres F, Vaides H, et al. Impact of an emergency triage assessment and treatment (ETAT)-based triage process in the paediatric emergency department of a Guatemalan public hospital. Paediatr Int Child Health 2016;36(3):219-224. https://doi.org/10.1179/2046905515y.0000000026 [ Links ]
30. Dekker-Boersema J, Hector J, Jefferys LF, et al. Triage conducted by lay-staff and emergency training reduces paediatric mortality in the emergency department of a rural hospital in Northern Mozambique. Afr J Emerg Med 2019;9(4):172-176. https://doi.org/10.1016/j.afjem.2019.05.005 [ Links ]
31. Molyneux EM, Langton J, Njiram'madzi J, Robertson AM. Setting up and running a paediatric emergency department in a hospital in Malawi: 15 years on. BMJ Paediatr Open 2017;1(1):e000014. https://doi.org/10.1136/bmjpo-2017-000014 [ Links ]
32. Drake M, Bishanga DR, Temu A, et al. Structured on-the-job training to improve retention of newborn resuscitation skills: A national cohort Helping Babies Breathe study in Tanzania. BMC Pediatr 2019;19(1):51. https://doi.org/10.1186/s12887-019-1419-5 [ Links ]
33. Woods DL. Improving neonatal care in district and community health facilities in South Africa. Paediatr Int Child Health 2015;35(3):187-191. https://doi.org/10.1179/2046905515y.0000000031 [ Links ]
34. Resuscitation Council United Kingdom. Generic Instructor Course 2021. https://www.resus.org.uk/training-courses/instructor-courses/gic-generic-instructor-course (accessed 2 May 2022). [ Links ]
35. O'Hare B, Phiri A, Lang H-J, et al. Task sharing within a managed clinical network to improve child health in Malawi. Hum Resour Health 2015;13(1):60. https://doi.org/10.1186/s12960-015-0053-z [ Links ]
36. English M. Improving emergency and admission care in low-resource, high mortality hospital settings - not as easy as A, B, C. Health Policy Plan 2022; 37(6):808-810. https://doi.org/10.1093/heapol/czab128 [ Links ]
37. World Health Organization. WHO technical consultation on oxygen access scale-up for COVID-19 2021. https://www.who.int/publications/i/item/9789240031517 (accessed 2 May 2022). [ Links ]
38. WHO-UNICEF. WHO-UNICEF technical specifications and guidance for oxygen therapy devices 2019 [cited 2019]. https://apps.who.int/iris/handle/10665/329874 (accessed 2 May 2022). [ Links ]
39. World Health Organization. Human resources for medical devices, the role of biomedical engineers 2017. https://www.who.int/publications/i/item/9789241565479. (accessed 2 May 2022). [ Links ]
40. World Health Organization. Standards for improving the quality of care for small and sick newborns in health facilities 2020. https://www.who.int/publications/i/item/9789240010765 (accessed 2 May 2022). [ Links ]
41. World Health Organization. Standards for improving the quality of care for children and young adolescents in health facilities 2018. Geneva: WHO; 2018 [ Links ]
42. World Health Organization. Interagency Triage Tool 2020. https://www.who.int/publications-detail/clinical-care-of-severe-acute-respiratory-infections-tool-kit (accessed 2 May 2022). [ Links ]
43. Mitchell R, McKup JJ, Bue O, et al. Implementation of a novel three-tier triage tool in Papua New Guinea: A model for resource-limited emergency departments. Lancet Reg Health West Pac 2020;5:100051. https://doi.org/10.1016/j.lanwpc.2020.100051 [ Links ]
44. Hategeka C, Lynd LD, Kenyon C, Tuyisenge L, Law MR. Impact of a multifaceted intervention to improve emergency care on newborn and child health outcomes in Rwanda. Health Policy Plan 2022;37(1):12-21. https://doi.org/10.1093/heapol/czab109 [ Links ]
45. Irimu G, Aluvaala J, Malla L, et al. Neonatal mortality in Kenyan hospitals: A multisite, retrospective, cohort study. BMJ Glob Health 2021;6(5):e004475. https://doi.org/10.1136/bmjgh-2020-004475 [ Links ]
46. Peng WS, Wang L, Zhang H, et al. Application of virtual scenario simulation combined with problem- based learning for paediatric medical students. J Int Med Res 2021;49(2):300060520979210. https://doi.org/10.1177%2F0300060520979210 [ Links ]
47. Dagnone JD, Hall AK, Sebok-Syer S, et al. Competency-based simulation assessment of resuscitation skills in emergency medicine postgraduate trainees - a Canadian multi-centred study. Can Med Educ J 2016;7(1):e57-e67. [ Links ]
 Correspondence:
Correspondence:
M Galatsch
michael.galatsch@zhaw.ch
Accepted 20 June 2022
Contribution of the study
This study aims to evaluate an updated Malagasy version of the Emergency Triage Assessment and Treatment Plus (ETAT+). The training met the participants' needs and was adapted to the clinical realities in Madagascar relating to transmitted knowledge, skills and competencies.














