Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
Southern African Journal of Critical Care (Online)
versão On-line ISSN 2078-676X
versão impressa ISSN 1562-8264
South. Afr. j. crit. care (Online) vol.38 no.1 Pretoria Mar. 2022
http://dx.doi.org/10.7196/SAJCC.2022.v38i1.517
RESEARCH
Professional quality of life of nurses in critical care units: Influence of demographic characteristics
E NdlovuI; C FilmalterII; J JordaanI; T HeynsII
IMCur; Department of Nursing Science, Faculty of Health Sciences, University of Pretoria, South Africa
IIPhD ; Department of Nursing Science, Faculty of Health Sciences, University of Pretoria, South Africa
ABSTRACT
BACKGROUND. Professional quality of life, measured as compassion satisfaction, is a prerequisite for nurses working in intensive care units where patients rely on their care. Nurses who experience compassion satisfaction, or good professional quality of life, engage enthusiastically with all work activities and render quality patient care. In contrast, compassion fatigue eventually leads to disengagement from work activities and unsatisfactory patient outcomes. In this study, we described the demographic factors influencing professional quality of life of intensive care nurses working in public hospitals in Gauteng, South Africa (SA), during the first wave of the COVID-19 pandemic.
OBJECTIVE. To describe the demographic factors associated with professional quality of life of critical care nurses working in Gauteng, SA.
METHODS. In this cross-sectional study, we used total population sampling and invited all nurses who had worked for at least 1 year in one of the critical care units of three selected public hospitals in Gauteng to participate. One-hundred and fifty-four nurses responded and completed the ProQol-5 tool during the first wave of the COVID-19 pandemic. Data were analysed using descriptive and inferential statistics.
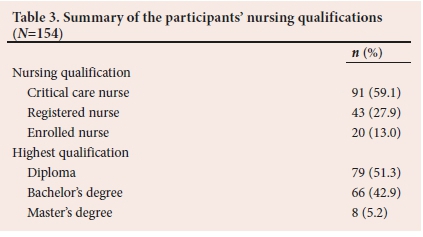
RESULTS. The nurses' average age was 45 years, and 59.1% (n=91) had an additional qualification in critical care nursing. Most of the nurses had a diploma (51.3%; n=79), with a mean work experience of 12.56 years. The main demographic variables that influenced professional quality of life were years of work experience (p=0.047), nurses' education with specific reference to a bachelor's degree (p=0.006) and nurse-patient ratio (p<0.001).
CONCLUSIONS. Nurses working in critical care units in public hospitals in Gauteng experienced low to moderate compassion satisfaction, moderate to high burnout and secondary traumatic stress, suggesting compassion fatigue. The high workload, which may have been associated with the COVID-19 pandemic, influenced nurses' professional quality of life.
Keywords: COVID-19, critical care, compassion fatigue, compassion satisfaction, nurses, professional quality of life.
Caring is an essential value in nurses' personal and professional lives'1-and a complex part of professional nursing practice. The quality of patient care and outcomes largely depends on a caregiver's professional quality of life (QOL). Nurses who have a positive professional QOL experience compassion satisfaction, while negative professional QOL is called compassion fatigue, which can be subdivided into burnout and secondary traumatic stress.[2] Behaviour and the trends resembling low professional QOL in the nursing profession as a whole have been reported in South Africa (SA),[3,4] and other countries such as the USA.[5] The QOL of nurses working in critical care units (CCUs) are of special concern, as the patients they care for are at high risk for actual or potential life-threatening health problems and require intensive and vigilant care.[6]
Critical care nurses gain satisfaction from giving compassionate care to patients and their families, but are prone to compassion fatigue as a result of repeated exposure to traumatic events.[7] CCUs are stressful working environments for healthcare workers owing to high morbidity and mortality rates, as well as ethical dilemmas that healthcare workers face on a daily basis.[8] The stressful environment was aggravated by the COVID-19 pandemic, described by the World Health Organization as a global health crisis. The pandemic caused an increase in number of admissions to CCUs, with healthcare organisations being overwhelmed by patients with COVID-19.[9] During the initial response to COVID-19 there were rapid protocol changes, and an increase of infection rates and deaths among patients and nurses infected with the virus.[10]
The chronic exposure to complex and demanding work issues in caring for critically ill patients in often resource-constrained CCUs, exacerbated by the COVID-19 pandemic, increases the risk for nurses to develop compassion fatigue.[11] This could cause nurses to leave the profession, causing increased turnover of CCU nurses, that may lead to increased healthcare costs, decreased productivity, low staff morale and an overall reduction in the quality of care provided.[12]
During day-to-day clinical practice we observed nurses working in three selected CCUs (prior to the outbreak of the COVID-19 pandemic) as being disengaged from their work environment and patient care, with high absenteeism rates and late-coming becoming a trend. We observed behaviours and trends associated with compassion fatigue, as described by other authors.[3,5] In this article, we determine whether certain demographic variables are associated with professional QOL of CCU nurses in public hospitals in Gauteng, SA, during the start of the COVID-19 pandemic.
Methods
Study setting and design
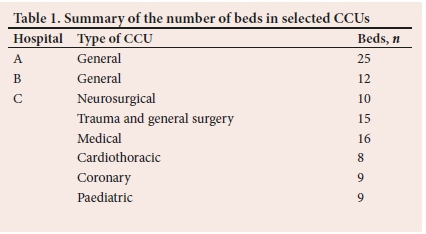
This cross-sectional study was conducted in eight CCUs of three selected public hospitals in the Tshwane region of Gauteng Province. The hospitals were selected as they employed the majority of critical care nurses in the Tshwane region. Table 1 gives a summary of the number of beds in the selected CCUs. The study was conducted from January to May 2020 during the first wave of the COVID-19 pandemic in SA. In many countries around the world, the COVID-19 pandemic has exacerbated the workload in CCUs,[13] potentially affecting staffing and impacting the professional QOL of nurses.
Study population and study procedure
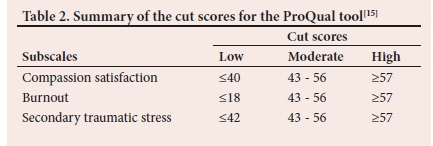
We sampled the total population,[14] of the 225 nurses that worked in the selected CCUs, including registered nurses specialising in critical care (115), registered nurses (86) and enrolled nurses (24). The population included all full-time employed nurses working in the selected CCUs for more than 1 year and who were willing to participate. Data were collected using the standardised Professional Quality of Life 5 tool (ProQoL-5), an English questionnaire with 30 items in the format of 5-point Likert scale questions, with answers ranging from 1 (never) to 5 (very often).[15] The ProQoL-5 is a validated tool that measures a participant's feelings or experiences of compassion satisfaction (10 items) and compassion fatigue (burnout (10 items) and secondary traumatic stress (10 items)). The scores for the three subscales are calculated on the 50th percentile and range between 43 and 57. Table 2 summarises the cut scores used by the ProQOL-5 tool to determine the three subscales of professional QOL. The questionnaire, which can be completed within 15 minutes, has been extensively tested, and has a reliability coefficient of 0.92 for compassion satisfaction, 0.84 for burnout, and 0.87 for secondary traumatic stress.[16]
Ethics approval was obtained from the Faculty ofHealth Science Research Ethics Committee of the University of Pretoria (ref. no. 491/2019), and the Department of Health, as well as the three selected public hospitals. Following ethics approval, we conducted information sessions with the unit managers and potential participants in each CCU to introduce and inform them of the aim of the study. We left 225 information leaflets and anonymous questionnaires to be voluntarily completed when and where convenient. The completed questionnaires were posted into a sealed container situated in the CCU unit managers' offices. Data were collected from January to May 2020, during the first wave of the COVID-19 pandemic. The time for data collection was extended to provide all the nurses an opportunity to participate and to ensure that we did not overwhelm them during the crisis.
Statistical analysis
Data were captured in Excel (Microsoft, USA) and analysed in collaboration with a statistician (JJ) using SPSS Statistics 27 (IBM, USA), and password protected. Data were analysed using frequencies and descriptive statistics including medians, means and standard deviations (SDs). We calculated total scores for each subscale using the Concise ProQoL-5 manual.[15] The subscales were transformed into standardised t-scores and categorised using the cut scores for the ProQoL-5. Cronbach's α was computed to assess the internal reliability of the subscales. The Shapiro-Wilk test was used to test if the data were normally distributed. Non-parametric Kruskal-Wallis tests were used to compare the median scores for the professional QOL in terms of compassion satisfaction and compassion fatigue (burnout and secondary traumatic stress) across selected demographic variables.
Results
We had a 68.4% response rate, and of the total of 154 questionnaires returned, 26.0% (n=40) were from hospital 1, 33.8% (n=52) from hospital 2 and 40.3% (n=62) from hospital 3. Cronbach's α revealed good internal reliability for the subscales: compassion satisfaction α=0.909; burnout α=0.805 and secondary traumatic stress α=0.797.
Demographic information
The respondents (n=154) had a mean (SD) age of 45 (9.59) years, ranging from 25 to 64 years old. Respondents reported having worked at the CCU for an average of 12.56 (7.76) years, ranging from 1 to 35 years. Respondents indicated that they cared for an average of 2.21 (1.30) patients per shift. Table 3 lists the nursing qualifications of the participants.
Professional quality of life
The descriptive statistics revealed that the majority of participants experienced low to moderate compassion satisfaction, compared with moderate to high burnout and secondary traumatic stress. Table 4 gives more detailed results.
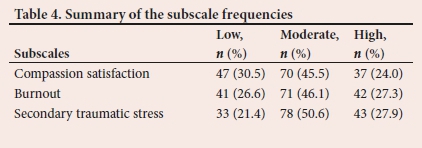
For compassion satisfaction, 30.5% (n=47) of participants scored below 44; 45.5% (n=70) scored between 44 and 57 and 24.0% (n=37) scored higher than 57, with a median score of f=51.75. For burnout, 26.6% of participants (n=41) scored below 43, 46.1% (n=71) scored between 43 and 56, and 27.3% (n=42) scored higher than 56 with a median of t=48.8. For secondary traumatic stress, 21.4% of participants (n=33) scored below 42, 50.6 (n=78) scored between 42 and 56, and 27.9% (n=43) scored higher than 56, with a median of t=51.35.
We compared the professional QOL subscales - compassion satisfaction, burnout and secondary traumatic stress across demographic variables (Table 5).
Professional QOL subscales did not differ for nurses of different ages or nursing categories. More experienced nurses reported higher compassion satisfaction (p=0.047), while more educated nurses experienced greater secondary traumatic stress (p=0.004). Dunn's post hoc tests for multiple comparisons revealed that nurses with bachelor's degrees had higher secondary traumatic stress subscale scores than nurses with diplomas (p=0.006).
All three subscales of the professional QOL were influenced by the number of patients nurses cared for per day. Nurses caring for only one patient had higher median compassion satisfaction scores (median t=56.27), compared with the nurses who cared for more than one patient (median t=50.46). Nurses who cared for one patient only had lower scores for secondary traumatic stress (median t=42.0) compared with nurses who cared for more than one patient (median t=53.04). Nurses caring for only one patient had lower scores for burnout (median t=42.93) compared with nurses who cared for more than one patient (median t=48.80).
Discussion
In this study, we measured the professional QOL of nurses working in CCUs in three selected public hospitals in Gauteng, SA. Data were collected during the first wave of the COVID-19 pandemic in SA. Our results indicate that the professional QOL of nurses working in CCUs at the start of the pandemic was low. Nurses working in CCUs experienced low to moderate compassion satisfaction and moderate to high burnout and secondary traumatic stress. These findings confirm conclusions reported in a systematic review done by Alharbi et al.[17]and a metaanalysis by Sinclair et al.[18] In addition, the COVID-19 pandemic has had a significant influence on nurses' professional and personal life, increasing the risk of developing compassion fatigue.[19, 20]
Caring for critically ill patients in highly stressful environments may put nurses at risk of developing compassion fatigue. The CCU environment exposes nurses to high patient morbidity and mortality, challenging daily work routines, excessive workloads,[20] conflicting professional relationships, emotional challenges and moral distress.[21,22]
The CCU environment was further complicated during the early stages of the COVID-19 pandemic as critical care nurses were required to triage patients and decide on modalities of care that increased their moral distress.[23] The results indicated that nurses in our sample were already presenting with moderate compassion fatigue, and the COVID-19 pandemic may further compromise interpersonal relationships, reduce productivity, decrease personal achievement, and increase absenteeism and high turnover.[24,25]-
Professional QOL may be influenced by demographic characteristics, suggesting that intrinsic qualities may affect how nurses cope in stressful environments. In our study, professional QOL was not associated with age, although conflicting reports about the influence of age exist.'26-A study conducted in the UK on the critical care workforce, including nurses, found that ProQol-5 scores were not influenced by age.[27] In the USA, Sacco and Copel[28] reported that older nurses (50 years or older) had higher compassion satisfaction. In Venezuela, nurses who were older than 40 years reported a healthier professional QOL, although they were more prone to burnout.[29] In Australia, younger nurses had higher burnout scores, but age was not associated with secondary traumatic stress.[30]
Years of experience and nursing category may influence professional QOL. In our study, nurses with more years of experience had higher compassion satisfaction. Compassion satisfaction was similar across the different nursing categories. Our findings concur with previous studies reporting that nurses with more years of working experience tend to have higher levels of compassion satisfaction, which may be due to their level of knowledge and coping skills.'31- In our study, all nurses suffered the same levels of burnout and secondary traumatic stress irrespective of age and category. Other studies have reported that burnout was more common in experienced nurses because of their work responsibility.[30,32] Austin et al.[33] also reported that years of experience had no influence on secondary traumatic stress. Public healthcare settings in SA have been shown to be high-stress environments, which may have resulted in nurses not being able to cope, irrespective of their experience or category.
The ability to function in a stressful environment may be linked to education. In our study, nurses in the CCU who had a bachelor's qualification scored higher on the secondary traumatic stress subscale than nurses with a diploma qualification, suggesting that nurses with diplomas may be more prepared to cope in a stressful environment. Other studies have reported that nurses with a bachelor's degree had lower compassion satisfaction than nurses with master's degrees. [28] In other studies, educational level had no effect on compassion satisfaction, compassion fatigue and burnout.[30] Higher education levels have previously been associated with higher levels of compassion satisfaction and reduced levels of compassion fatigue.[18] Education levels may influence healthcare professionals' perceptions of responsibility and duty towards patients.[26] Most of the nurses who responded in our study were registered nurses (n=134) and 59.1% of these nurses had an additional qualification in critical care nursing. Nurses with additional qualifications in critical care may be better prepared for the challenges experienced in practice, which could allow for a better professional QOL.[29,34] However, regardless of demographic characteristics, Wu et al.[35] have theorised that nurses caring for patients suffering from COVID-19 may be so focused on achieving optimal patient outcomes that their personal care is put on the back burner.
Nurses in our study were exposed to heavy workloads, which is an important factor contributing to compassion fatigue.[36] Nurses reported having to care for more than one patient per shift, which is in contrast to the recommended 1:1 nurse-to-patient ratio for critical care settings.[37-Heavy workload is described as an organisational challenge brought about by having to care for many patients with high patient acuity.[1] As in our study, in healthcare environments where resources and staffing are not ideal, nurses tend to report lower levels of compassion satisfaction.[38] In addition, shift (day and night) work has been found to be directly linked to burnout in nurses.[26] It is possible to enjoy work when a balance exists between a challenging workload and support in the work environment.[27] However, the demographic characteristics that influence the nurses' ability in dealing with the COVID-19 pandemic will only come to light with the dissemination of more research.
Conclusions
Our results support previously reported findings. Burnout is common among nurses caring for critically ill patients and organisations should provide support to preserve the nursing workforce. In this study setting, nurses with more years of experience had a better professional QOL. Younger nurses must be nurtured and enabled to develop coping skills when entering the critical care environment. We also noticed that nurses with bachelors' degrees experienced higher secondary traumatic stress, a phenomenon which needs further investigation. The nurses cared for an average of 2.21 patients per day, which is above the suggested 1:1 ratio in a CCU. To improve compassion satisfaction that promotes quality patient care, health services should optimise efficiency and align resources to promote nurses' wellbeing.
The results give us an important glimpse into the circumstances of nurses working under the extreme stress of a pandemic. Of concern is that the critical care nurses experienced moderate to high burnout and secondary traumatic stress at the start of the pandemic. This study was conducted during the first wave of the COVID-19 pandemic and the accompanied stressors, uncertainty and increased workload may have limited the participation of nurses, especially in certain CCUs. The participants only represent critical care nurses working in the public hospitals in the Tshwane region. Further research is therefore required to explore the compassion of nurses working in CCUs as the COVID-19 pandemic unfolds, including critical care nurses working in the private sector and in other provinces. Future research should focus on the nurse as 'self', their personal life, and their perceptions of wellbeing, as well as requirements to promote mental health. Quality patient care depends on the professional QOL of nurses, which should be prioritised in all organisations as the COVID-19 pandemic has provided evidence of nurses' irreplaceable contribution to healthcare.
Declaration. None.
Acknowledgements. Dr Cheryl Tosh for editing.
Author contributions. ET conceptualised the study, collected and analysed the data, and wrote the manuscript. CF and TH conceptualised the study, assisted with interpretation of the results, and wrote and finalised the manuscript for submission. JJ analysed data and guided data analysis and the results section of the manuscript.
Funding. None.
Conflicts of interest. None.
References
1. Mohammadi M, Peyrovi H, Mahmoodi M. The relationship between professional quality of life and caring ability in critical care nurses. Dimens Crit Care Nurs 2017;36(5):273-277. https://doi.org/10.1097/dcc.0000000000000263 [ Links ]
2. Kim K, Han Y, Kim J-S. Korean nurses' ethical dilemmas, professional values and professional quality of life. Nurs Ethics 2015;22(4):467-478. https://doi.org/10.1177/0969733014538892 [ Links ]
3. Nolte AG, Downing C, Temane A, Hastings-Tolsma M. Compassion fatigue in nurses: A metasynthesis. J Clin Nurs 2017;26(23-24):4364-4378. https://doi.org/10.1111/jocn.13766 [ Links ]
4. Maila S, Martin PD, Chipps J. Professional quality of life amongst nurses in psychiatric observation units. S Afr J Psychiatry 2020;26(1):1-7. [ Links ]
5. Lachman VD. Compassion fatigue as a threat to ethical practice: Identification, personal and workplace prevention/management strategies. Medsurg Nurs 2016;25(4):275. [ Links ]
6. Urden LD, Stacy KM, Lough ME. Priorities in Critical Care Nursing, 8th ed. (E-book). Elsevier Health Sciences, 2019; 9 January. [ Links ]
7. Mathias C, Wentzel D. Descriptive study of burnout, compassion fatigue and compassion satisfaction in undergraduate nursing students at a tertiary education institution in KwaZulu-Natal. Curationis 2017;40(1):1-6. https://doi.org/10.4102/curationis.v40i1.1784 [ Links ]
8. Alharbi H, Alshehry A. Perceived stress and coping strategies among ICU nurses in government tertiary hospitals in Saudi Arabia: A cross-sectional study. Ann Saudi Med 2019;39(1):48-55. https://doi.org/10.5144/0256-4947.2019.48 [ Links ]
9. Shen X, Zou X, Zhong X, Yan J, Li L. Psychological stress of ICU nurses in the time of COVID-19. Crit Care 2020;24(1):1-3. https://doi.org/10.1186/s13054-020-02926-2 [ Links ]
10. Crowe S, Howard AF, Vanderspank-Wright B, et al. The effect of COVID-19 pandemic on the mental health of Canadian critical care nurses providing patient care during the early phase pandemic: A mixed method study. Intensive Crit Care Nurs 2021;1;63:102999. https://doi.org/10.1016/j.iccn.2020.102999 [ Links ]
11. Mo Y, Deng L, Zhang L, et al. Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. J Nurs Manag 2020;28(5):1002-1009. https://doi.org/10.1111/jonm.13014 [ Links ]
12. Mealer M, Moss M. Moral distress in ICU nurses. Intensive Care Med 2016;42(10):1615-1617. https://doi.org/10.1007%2Fs00134-016-4441-1 [ Links ]
13. Lucchini A, Giani M, Elli S, et al. Nursing activities score is increased in COVID-19 patients. Intensive Crit Care Nurs 2020;59. https://doi.org/10.1016%2Fj.iccn.2020.102876 [ Links ]
14. Etikan I, Musa SA, Alkassim RS. Comparison of convenience sampling and purposive sampling. Am J Theoretical Applied Statist 2016;5(1):1-4. https://doi.org/10.11648/j.ajtas.20160501.11 [ Links ]
15. Stamm BH. The Concise ProQOL Manual. 2nd ed. Pocatello: Eastwoods, 2010. [ Links ]
16. Hemsworth D, Baregheh A, Aoun S, Kazanjian A. A critical enquiry into the psychometric properties of the professional quality of life scale (ProQol-5) instrument. Appl Nurs Res 2018;39:81-88. https://doi.org/10.1016/j.apnr.2017.09.006 [ Links ]
17. Alharbi J, Wilson R, Woods C, Usher K. The factors influencing burnout and job satisfaction among critical care nurses: A study of Saudi critical care nurses. J Nurs Manag 2016;24(6):708-717. https://doi.org/10.1111/jonm.12386 [ Links ]
18. Sinclair S, Raffin-Bouchal S, Venturato L, Mijovic-Kondejewski J, Smith-MacDonald L. Compassion fatigue: A meta-narrative review of the healthcare literature. Int J Nurs Stud 2017;69:9-24. https://doi.org/10.1016/j.ijnurstu.2017.01.003 [ Links ]
19. Alharbi J, Jackson D, Usher K. The potential for COVID-19 to contribute to compassion fatigue in critical care nurses. J Clin Nurs 2020; May. https://doi.org/10.1111/jocn.15314 [ Links ]
20. Moss M, Good VS, Gozal D, Kleinpell R, Sessler CN. A Critical Care Societies Collaborative Statement: Burnout syndrome in critical care health-care professionals. A call for action. Am J Respir Crit Care Med 2016;194(1):106-113. https://doi.org/10.1164/rccm.201604-0708st [ Links ]
21. Austin CL, Saylor R, Finley PJ. Moral distress in physicians and nurses: Impact on professional quality of life and turnover. Psychol Trauma 2017;9(4):399. https://doi.org/10.1037/tra0000201 [ Links ]
22. Ingebretsen LP, Sagbakken M. Hospice nurses' emotional challenges in their encounters with the dying. Int J Qual Stud Health Well-being 2016;11(1):31170. https://doi.org/10.3402%2Fqhw.v11.31170 [ Links ]
23. Bambi S, Iozzo P, Rasero L, Lucchini A. COVID-19 in critical care units: Rethinking the humanisation of nursing care. Dimens Crit Care Nurs 2020;1;39(5):239-241. https://doi.org/10.1097/dcc.0000000000000438 [ Links ]
24. Dilig-Ruiz A, MacDonald I, Demery Varin M, et al. Job satisfaction among critical care nurses: A systematic review. Int J Nurs Stud 2018;88:123-134. https://doi.org/10.1016/j.ijnurstu.2018.08.014 [ Links ]
25. Cishahayo E, Nankundwa E, Sego R, Bhengu B. Burnout among nurses working in critical care settings: A case of a selected tertiary hospital in Rwanda. Int J Res Med Sci 2017;5(12):5121-5128. https://doi.org/10.18203/2320-6012.ijrms20175430 [ Links ]
26. Ruiz-Fernández MD, Ramos-Pichardo JD, Ibáñez-Masero O, et al. Compassion fatigue, burnout, compassion satisfaction and perceived stress in healthcare professionals during the COVID-19 health crisis in Spain. J Clin Nurs 2020;29(21-22):4321-4330. https://doi.org/10.1111/jocn.15469 [ Links ]
27. Highfield J, Parry-Jones J. Professional quality of life in intensive care medicine: The 2018 Faculty of Intensive Care Medicine Workforce survey. J Intensive Care Soc 2020;21(4):299-304. https://doi.org/10.1177/1751143719877102 [ Links ]
28. Sacco TL, Copel LC. Compassion satisfaction: A concept analysis in nursing. Nurs Forum 2018;53(1):76-83. https://doi.org/10.1111/nuf.122130 [ Links ]
29. Quijada-Martínez PJ, Cedeño-Idrogo IR, Terán-Ángel G. Quality of professional life and burnout of the nursing staff at an intensive care unit in Venezuela. Invest Educ Enferm 2021;39(2). https://doi.org/10.17533/udea.iee.v39n2e08 [ Links ]
30. Jakimowicz S, Perry L, Lewis J. Compassion satisfaction and fatigue: A cross-sectional survey of Australian intensive care nurses. Aust Crit Care 2018;31(6):396-405. https://doi.org/10.1016/j.aucc.2017.10.003 [ Links ]
31. Salimi S, Pakpour V, Rahmani A, Wilson M, Feizollahzadeh H. Compassion satisfaction, burnout, and secondary traumatic stress among critical care nurses in Iran. J Transcult Nurs 2020;31(1):59-66. https://doi.org/10.1177/1043659619838876 [ Links ]
32. Shoorideh FA, Ashktorab T, Yaghmaei F, Alavi Majd H. Relationship between ICU nurses' moral distress with burnout and anticipated turnover. Nurs Ethics 2015;22(1):64-76. https://doi.org/10.1177/0969733014534874 [ Links ]
33. Austin CL, Pathak M, Thompson S. Secondary traumatic stress and resilience among EMS. J Paramedic Pract 2018;10(6):240-247. https://doi.org/10.12968/jpar.2018.10.6.240 [ Links ]
34. Fraley TE. Transitioning novice nurses to expert nurses in progressive telemetry care. Master of Science nursing thesis, Gardner-Webb University, 2016. [ Links ]
35. Wu Y, Wang J, Luo C, et al. A comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in Wuhan, China. J Pain Symptom Manag 2020;1;60(1):e60-5. https://doi.org/10.1016/j.jpainsymman.2020.04.008 [ Links ]
36. O'Callaghan EL, Lam L, Cant R, Moss C. Compassion satisfaction and compassion fatigue in Australian emergency nurses: A descriptive cross-sectional study. Int Emerg Nurs 2020;48:100785. https://doi.org/10.1016/j.ienj.2019.06.008 [ Links ]
37. Marshall JC, Bosco L, Adhikari NK, et al. What is an intensive care unit? A report of the task force of the World Federation of Societies of Intensive and Critical Care Medicine. J Crit Care 2017;37:270-276. https://doi.org/10.1016/j.jcrc.2016.07.015 [ Links ]
38. Baek J, Cho H, Han K, Lee H. Association between nursing work environment and compassion satisfaction among clinical nurses. J Nurs Manag 2020;28(2):368-376. https://doi.org/10.1111/jonm.12937 [ Links ]
 Correspondence:
Correspondence:
C Filmalter
celia.filmalter@up.ac.za
Accepted 3 February 2022
Contributions of the study
This study reports on the important problem of compassion fatigue and burnout amongst South African ICU nurses working in the public sector. Associated factors were identified, which should be addressed to improve nurses' wellbeing.














