Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
Southern African Journal of Critical Care (Online)
On-line version ISSN 2078-676X
Print version ISSN 1562-8264
South. Afr. j. crit. care (Online) vol.38 n.1 Pretoria Mar. 2022
http://dx.doi.org/10.7196/SAJCC.2022.v38i1.515
RESEARCH
The impact of government- and institution-implemented COVID-19 control measures on tertiary- and regional-level intensive care units in Pietermaritzburg, KwaZulu-Natal Province, South Africa
K RangaiI; A RamkillawanII; M T D SmithIII
IMB ChB ; Department of Anaesthetics and Critical Care, School of Clinical Medicine, University of KwaZulu-Natal, Durban, South Africa
IIMB ChB, Cert Crit Care (SA) ; Department of Anaesthetics and Critical Care, School of Clinical Medicine, University of KwaZulu-Natal, Durban, South Africa
IIIMB ChB, MMed (Surg). Department of Anaesthetics and Critical Care, School of Clinical Medicine, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND. The COVID-19 pandemic has had a significant impact on healthcare systems globally as most countries were not equipped to deal with the outbreak. To avoid complete collapse of intensive care units (ICUs) and health systems as a whole, containment measures had to be instituted. In South Africa (SA), the biggest intervention was the government-regulated national lockdown instituted in March 2020.
OBJECTIVE. To evaluate the effects of the implemented lockdown and institutional guidelines on the admission rate and profile of non-COVID-19 patients in a regional and tertiary level ICU in Pietermaritzburg, KwaZulu-Natal Province, SA.
METHODS. A retrospective analysis of all non-COVID-19 admissions to Harry Gwala and Greys hospitals was performed over an 8-month period (1 December 2019 - 31 July 2020), which included 4 months prior to lockdown implementation and 4 months post lockdown.
RESULTS. There were a total of 678 non-COVID-19 admissions over the 8-month period. The majority of the admissions were at Greys Hospital (52.4%; n=355) and the rest at Harry Gwala Hospital (47.6%; n=323). A change in spectrum of patients admitted was noted, with a significant decrease in trauma and burns admissions post lockdown implementation (from 34.2 - 24.6%; p=0.006). Conversely, there was a notable increase in non-COVID-19 medical admissions after lockdown regulations were implemented (20.1 - 31.3%; p<0.001). We hypothesised that this was due to the gap left by trauma patients in an already overburdened system.
CONCLUSIONS. Despite the implementation of a national lockdown and multiple institutional directives, there was no significant decrease in the total number of non-COVID-19 admissions to ICUs. There was, however, a notable change in spectrum of patients admitted, which may reflect a bias towards trauma admissions in the pre COVID-19 era.
Keywords: COVID-19, non-COVID-19 admissions, ICU, lockdown.
The novel coronavirus pandemic has resulted in significant changes in both healthcare infrastructure and systems globally. South Africa (SA), along with other countries across the globe, resorted to large-scale nonpharmaceutical interventions in an attempt to curb the impact on vulnerable groups and an already stressed healthcare system. On the 15 March 2020, the SA government declared a national state of disaster. Twelve days later, a country-wide lockdown was implemented from the 27 March 2020. This involved closure of schools and non-essential services, cessation of the distribution and sale of alcohol and cigarettes, cessation of visitation to correctional facilities, the implementation of a curfew and restriction on any travel as well as various other measures. This swift action led to a reduction in doubling time of new infections from two days to 15 in the 35 days following the implementation of lockdown.[1]
Implementation of lockdown regulations had a significant impact on the SA healthcare system. Healthcare resources and staff were redeployed as part of an attempt to streamline workflow, improve intensive care capacity and aid in combating the pandemic. The interventions included (but were not limited to) termination of nonurgent (elective) surgical services and the curtailment of outpatient services.[2] These changes had both direct and indirect effects on intensive care unit (ICU) services, and led to significant short- and long-term consequences for patients. A local study demonstrated a 47% reduction in the number of trauma cases presenting to the emergency department after the implementation of lockdown regulations.[3] Furthermore, there was a 30% reduction in theatre operations, resulting in a significant backlog that may take close to a year to resolve.[4]
The restructuring of ICUs in preparation for COVID-19 patients has been widely reported. What effect the pandemic and associated regulations have had on non-COVID-19 admissions to the ICUs is unknown.[5,6] We aimed to evaluate the effect of government regulations and institutional directives during the COVID-19 pandemic on both tertiary- and regional-level ICU non-COVID-19 admissions.
Methods
A retrospective descriptive analysis of all non-COVID-19 admissions to a tertiary- and regional-level ICU was performed by interrogation of a prospectively-collected critical care database known as the Intensive Care Electronic System (ICES). Ethical approval to collect and maintain data in ICES was granted by the University of KwaZulu-Natal Biomedical Research Ethics Committee (ref. no. BCA 211/14). The study was conducted at both Greys Hospital (GH) and Harry Gwala Hospital (HGH). Data were collected over an 8-month period from 1 December 2019 - 3 July 2020. The first four months i.e.. 1 December - 31 March 2020 were predominantly prior to the implementation of lockdown, hereafter referred to as pre-lockdown, and 1 April - 31 July 2020 occurring afterwards, hereafter referred to as post-lockdown. All data pertaining to referrals, admissions and discharges to the respective ICUs were collated in an Excel spreadsheet (Microsoft Corp., USA).
Capturing information to the database is usually done by the attending ICU doctor and is based on a hand-written referral form, as well as a bedside clinical assessment of the patient. This forms part of the clinical hospital record and therefore includes general information such as type of referral/admission (i.e. elective v. emergency), patients' demographic details, medical history, clinical condition and vital signs, as well as biochemical results. As the unit functions as a multi-disciplinary unit, patients were further categorised according to discipline on admission, namely trauma and burns surgery, general surgery, paediatric surgery, orthopaedics, urology, obstetrics and gynaecology, ear, nose and throat surgery, maxillofacial surgery, plastic surgery, internal medicine and paediatrics. Paediatric patients were only admitted to the ICU if no beds were available in the paediatric ICU. Ethics approval for this study was obtained from the University of KwaZulu-Natal's Biomedical Research Ethics Committee (ref. no. BREC/2064/2020); the provincial Department of Health's Research Committee (ref. no. KZ_202103_016), as well as the CEO and medical managers of GH and HGH.
Clinical setting
The Pietermaritzburg Metropolitan Hospital Complex in KwaZulu-Natal Province, SA, provides healthcare services to ~5.9 million people. In SA, there are six critical care beds per 100 000 people.[7,8] Only 25% of these beds are available in the public healthcare sector.[9] GH and HGH form part of this complex, providing tertiary- and regionallevel critical care services, respectively. HGH was previously known as Edendale Hospital at the time that the data were collected. GH runs 510 inpatient beds and 11 adult ICU beds, with the ability to surge to 12 beds when needed. HGH is a 897-bed hospital which runs six ICU and three high-care beds. The units functioned as consultant-led closed multidisciplinary ICUs. Preceding lockdown, the Department of Health issued multiple directives to healthcare institutions, halting elective surgical services and redistributing staff to bolster intensive care services in preparation for the expected surge of COVID-19 cases. However, at GH, allowances were made once a week for a single surgical oncology elective case as bed availability allowed.
HGH maintained their non-COVID-19 ICU capacity and repurposed a general ward to manage COVID-19-positive patients. ICU staff were mobilised to care for ventilated COVID-19-positive patients in the satellite ward. In GH, infrastructural changes occurred to divide the unit to create an isolation area where COVID-19 critically ill patients could be managed safely. This resulted in a reduction in the non-COVID-19 component to nine beds, with seven beds allocated to caring for COVID-19-positive patients. Any overflow of non-COVID-19 ICU admissions was managed in a 4-bed temporary ICU in the Coronary Care Unit, which operated as an open ICU. Extra nursing staff were employed on a short-term contract basis to bolster human resources and skills.
Statistical analysis
The Excel (Microsoft Corp., USA) spreadsheet was exported to R (RStudio, USA) for analysis. Categorical variables were expressed as frequencies and percentages and were compared using the Chi-squared test. Continuous variables were expressed as medians and interquartile range (IQR) as the distribution was non-normal. The Wilcoxon test was used for comparison of non-parametric data. Alpha level was set at 0.05.
Results
Admission profile
Over the 8-month period, there was a total of 678 non-COVID-19 admissions to the public sector ICUs in Pietermaritzburg. Of these, 52.4% (n=355) were admitted to GH and 47.6% (n=323) to HGH. The median (IQR) age at admission was 36 (26 - 51) years. The overall mortality rate was 15.9% (n=108). The distribution of admissions was as follows: trauma and burns (29.4%; n=199); general surgery (27.0%; n=183), non-COVID-19 medical ward (25.8%; n=175) and obstetrics (8.4%; n=57). Elective admissions to ICU accounted for 9.0% (n=61) of all admissions over the 8-month period. These details may be seen in Table 1.
Pre-lockdown comparison between tertiary- and regional-hospital ICU admissions
GH admitted 203 patients to the ICU in the pre-lockdown period, while HGH admitted 130 patients. Patients admitted at GH were older than HGH patients (p=0.002) with a median (IQR) age of 38 (29 - 52) years and 32.5 (24 - 38) years, respectively. GH had a greater proportion of elective admissions than HGH (p=0.036) with 12.3% and 5.4%, respectively. In-ICU mortality rates were similar between the two hospitals (15.8% and 14.6%; p=0.777). There was no significant difference between the proportion of trauma and burns admissions between the two ICUs (p=0.555). GH admitted 33% (n=67) of trauma and burns patients while HGH admitted 36.2% (n=47) of trauma and burns patients during the pre-lockdown period. HGH admitted a significantly greater proportion of medical patients than GH in the pre-lockdown period. More than a third of admissions to HGH ICU (36%; n=47) were medical admissions while this subset of patients accounted only for 9.9% (n=20) of GH admissions (odds ratio (OR) 5.13; 95% confidence interval (CI) 2.89 - 9.40). Conversely, GH admitted a greater proportion of general surgical patients than HGH. General surgical conditions accounted for 35% (n=71) of GH ICU admissions and only 16.2% (n=21) of HGH admissions. These differences may be seen in Table 2.
Post-lockdown comparison between tertiary-and regional-level hospital ICU admissions
In the post lockdown period, the median age of patients at admissions was similar between the two hospitals (37 and 36 years; p=0.720). Mortality rate was also similar (15.1% and 17.6%; p=0.537). Although the absolute number of trauma and burns admissions to HGH were similar between the two periods (n=47 and n=48), the proportion of trauma and burns admissions to overall admissions to HGH ICU, decreased by 11.3% to 24.9% (p=0.029). Trauma and burns admissions to GH decreased from 33% (n=67) to 24.3% (n=37). These differences, however, did not meet statistical significance (p=0.076). At HGH, the absolute number of general surgery admissions increased from 16.2% (n=21) to 20.7% (n=40) of ICU admissions. Non-COVID-19 medical patients increased from 36.2% (n=47 ) to 42% (n=81). Obstetrics and gynaecology ICU admissions increased from 5.4% (n=7) to 7.3% (n=14). These trends can be seen in Fig. 1. Although there was an increase in non-trauma and burns admissions in HGH (63.8 - 75.1%; p=0.029), there was no individual discipline that showed statistical significance in proportional change. At GH, there were no significant changes in both general surgical and obstetric admissions to ICU (p=0.780 and p=0.835, respectively). Notably, there was a significant increase in the proportion of non-COVID-19 medical admissions to GH (17.8%; p=0.030). Elective admissions remained relatively constant at both GH and HGH (15.1% and 3.1%, respectively; p=0.443). Details may be seen in Table 3.
Overall changes to Pietermaritzburg state sector ICUs after lockdown regulations
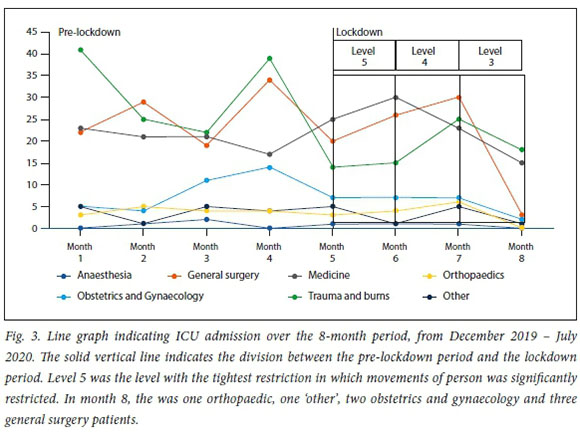
The median (IQR) age was 36 (26 - 51) years. This was similar to the pre-lockdown median (IQR) age of 37 years (25 - 51; p=0.798). Elective admissions accounted for 9.6% of ICU admissions, which was not significantly different post lockdown (8.4%; p=0.584). There was a change in the spectrum of patients admitted as demonstrated in Fig. 2. Overall, there was a significant decrease in trauma and burns admissions after regulations were implemented (34.2% (n=114) to 24.6% (n=85); p=0.006). However, general surgery and obstetric admissions were unchanged (p=0.714 and p=0.783, respectively). Of note, there was a significant increase in non-COVID-19 medical admissions after lockdown regulations were implemented (20.1% - 31.3%; p<0.001). These trends can be seen in Fig. 3. The mortality rate trended higher after lockdown was implemented but this finding was not statistically significant (14.6% and17.6%; p=0.475).
Impact of regulations on admission physiological variables
The pre lockdown median (IQR) heart rate was 114 (96 - 130) bpm and 111 (94 - 126) bpm post lockdown. This difference was not significant (p=0.202). The median (IQR) respiratory rate was also similar in both groups (17 (15 - 22) bpm and 18 (15 - 21) bpm; p=0.947). Serum lactate was similar in the two groups (2.3 and 2.1 mmol/L, respectively). Of note, patients admitted during the lockdown period had reduced metabolic acidosis with >2 mmol/L improvement in median serum-base excess than before lockdown (p=0.033). Details may be found in Table 1.
Subgroup analysis
Harry Gwala Hospital
Physiological parameters on admission to ICU were similar in the pre- and post lockdown subgroups admitted to HGH ICU. The only significant difference found regarded serum urea levels. The median (IQR) serum urea was 6.6 (4.1 - 9.7 ) mmol/L pre lockdown while the median (IQR) serum levels were 8.1 (4.8 - 15.3) mmol/L post lockdown (p=0.040).
Greys Hospital
The physiological parameters were also similar in the GH subgroup. The only significant difference was in the base excess (BE). The median (IQR) BE was -6.8 mmol/L (-11.4 -2.2mmol/L)) pre lockdown and improved to -2.5 (-8.9 - 2.9) mmol/L (p<0.001) post lockdown.
Discussion
The government and institutional regulations instituted in response to the coronavirus pandemic aimed to reduce the non-COVID burden on healthcare facilities, as well as to mobilise resources towards the management of COVID-19 patients. Our study performed an analysis to investigate what the actual consequences of these regulations were on ICU non-COVID-19 admissions to our hospital complex.
ICU need outweighs ICU capacity
There is a significant burden placed on public ICUs in SA. Prior to the COVID-19 pandemic, SA had six ICU beds per 100 000 people.]7,8] Only 25% of these beds were available in the public sector, 14% of which were in KwaZulu-Natal Province.[9] In Pietermaritzburg, 62% of suitable ICU candidates are never admitted to ICU due to a lack of bed availability.[10] This indicates that the need far outweighs the capacity.
The government regulations that were implemented on 27 March 2020, in terms of Section 27(2) of the Disaster Management Act of 2002, included the closure of schools and partial-care facilities, closure of non-essential services and cessation of the distribution and sale of alcohol and cigarettes. Zsilavecz et al.found that the rate of trauma admissions decreased significantly in response to the change in regulations. This was consistent with our findings of decreased percentage of trauma admissions to the ICU. The authors hypothesised that this was in part due to reduced consumption of alcohol by the public[11] However, there were various conditions that were not affected by social behaviour and therefore were not affected by the regulations.
Prior to the implementation of the regulations, trauma referral rates were higher than medical patients in ICUs in Pietermaritzburg. ICU acceptance rates also favoured trauma patients over medical patients (79% and 60%, respectively).[10] This may reflect bias in favour of trauma patients in Pietermaritzburg ICUs. This discrepancy may also be guided by bed availability. A French study by Robert etal.[12]suggested that ICU bed availability influenced the triage of ICU patients. The rate of patients deemed 'too sick' for ICU increased as bed availability decreased.[12] This may have possibly impacted the profile of ICU admissions in the pre-COVID era. With the decrease in trauma cases and subsequent ICU referrals during the lockdown period, a capacity gap may have been created that allowed more non-trauma admissions.
More non-COVID-19 medical admissions to ICU during lockdown
At both our regional- and tertiary-level ICUs, there were significantly more non-COVID-19 medical admissions during lockdown. This may reflect the capacity gap left by the decrease in trauma cases. However unlikely, we cannot exclude that some of these medical patients may have, in fact, had COVID-19 although they had tested PCR-negative or perhaps previously had COVID-19. Kanji et al.[13] state that due to the false-negative rate associated with various phases of COVID-19, a positive PCR should not be the only diagnostic criterion for the disease. In future, we may need to reassess our criteria for diagnosing COVID-19. The decrease in trauma admissions and increase in non-COVID-19 medical admissions resulted in the number of non-COVID-19 admissions during lockdown being similar to pre lockdown ICU admissions.
There was a change in the physiological profile of patients post lockdown. This may reflect the changes in disease frequency and distribution but more information is needed to support this possibility. There seemed to be an overall lower rate of metabolic acidosis during lockdown and a higher prevalence of renal impairment at our regional ICU.
No reduction in elective cases
Our study reflects the low admission rate of elective cases to our ICUs even prior to lockdown. This reflects the burden of emergency surgery cases on our ICUs. By allowing surgical oncology cases to be performed once a week pending bed availability, the rate of these admissions remained relatively constant.
Study limitations
The findings of the study reflect the workload of two ICUs in a single city. This was a retrospective study and insufficient clinical admission data precludes the ability to compare severity of illness during the investigated periods. In order to assess the national impact of lockdown regulations, a national multi-centre study is required. Owing to missing gender variables at one of our centres, we could not comment on the significance of gender in this study. Admission to ICU was at the discretion of the specialist on call. This may have resulted in inter-consultant variability and possibly, bias.
Conclusion
The need for ICU beds in SA far outweighs the available capacity. Although the number of trauma patients decreased after implementation of lockdown regulations, the total number of non-COVID admissions at our ICUs did not significantly decrease. Instead, the spectrum of admissions changed by creating a gap for non-COVID-19 medical admissions. This may reflect bias toward trauma admissions. These factors need to be studied further so that they can be understood and reform instituted.
Declaration. None.
Acknowledgements. None.
Author contributions. KR conceptualised and designed the study. MTDS collected and analysed data. AR interpreted the findings and wrote the draft manuscript. KR and MTDS revised the manuscript. All authors approved the final version of the manuscript for publication.
Conflicts of interest. None.
Funding. None.
References
1. Abdool Karim SS. The South African response to the pandemic. N Engl J Med 2020;382(24):e95 https://doi:10.1056/NEJMc2014960 [ Links ]
2. Parker A, Karamchand S, Schnieder N, et al. Leadership and early strategic response to the SARS-CoV-2 pandemic at a COVID-19 designated hospital in South Africa. S Afr Med J 2020;110(6):463-465. https://doi.org/10.7196/SAMJ.2020v110i6.14809. [ Links ]
3. Morris D, Rogers M, Kissmer N, et al. Impact of lockdown measures implemented during the COVID-19 pandemic on the burden of trauma presentations to a regional emergency department in Kwa-Zulu Natal, South Africa, African J Emergency Med 2020;10(4):193-196. https://doi.org/10.1016/j.afjem.2020.06.005 [ Links ]
4. Laäs DJ, Farina Z, Bishop DG. Effect of COVID-19 pandemic decisions on tertiary-level surgical services in Pietermaritzburg, KwaZulu-Natal Province, South Africa. S Afr Med J 2021;111(2):120-123. https://doi.org/10.7196/SAMJ.2021.v111i2.15332. [ Links ]
5. Aziz S, Arabi YM, Alhazzani W, et al. Managing ICU surge during the COVID-19 crisis: Rapid guidelines. Intensive Care Med 2020;46:1303-1325. https://doi.org/10.1007/s00134-020-06092-5 [ Links ]
6. Grasselli G, Pesenti A, Cecconi M. Critical care utilisation for the COVID-19 outbreak in Lombardy, Italy: Early experience and forecast during an emergency response. JAMA 2020;323(16):1545-1546. https://doi.org/10.1001/jama.2020.4031 [ Links ]
7. Ayebale E, Kassebaum NJ, Roche AM, Biccard BM. Africa's critical care capacity before COVID-19. S Afr J Anaes Analg 2020;26:162-164. https://doi:10.36303/SAJAA.2020.26.3.2431 [ Links ]
8. Bhagwanjee S, Scribante J. National audit of critical care resources in South Africa - unit and bed distribution. S Afr Med J 2007;97(12):1311-1314. https://doi.org/10.7196/SAMJ.555. [ Links ]
9. Naidoo K, Singh J, Lalloo U. A critical analysis of ICU/HC beds in South Africa: 2008-2009, 2013. S Afr Med J 2013;103(10):751-753. https://doi.org/10.7196/SAMJ.6415. [ Links ]
10. Gordon K, Allorto N, Wise R. Analysis of referrals and triage patterns in a South African metropolitan adult intensive care service 2015. S Afr Med J 2015;105(6):491-495. https://doi.org/10.7196/SAMJ.9007. [ Links ]
11. Zsilavecz A, Wain H, Bruce JL, et al. Trauma patterns during the COVID-19 lockdown in South Africa expose vulnerability of women. S Afr Med J 2020;110(11):1110-1112. https://doi.org/10.7196/SAMJ.2020.v110i11.15124 [ Links ]
12. Robert R, Coudroy R, Ragot S, et al. Influence of ICU-bed availability on ICU admission decisions. Ann Intensive Care 2015;5(1):55. https://doi.org/10.1186/s13613-015-0099-2 [ Links ]
13. Kanji JN, Zelyas N, MacDonald C, et al. False negative rate of COVID-19 PCR testing: A discordant testing analysis. Virology J 2021;18(1):13. https://doi.org/10.1186/s12985-021-01489-0 [ Links ]
 Correspondence:
Correspondence:
M T D Smith
mtdsmith1708@yahoo.com
Accepted 24 February 2022
Contributions to the field
We describe the impact of the COVID-19 pandemic on critical care services in a resource-limited setting. We also demonstrate the ongoing need for intensive care unit beds within the public sector.














