Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
Southern African Journal of Critical Care (Online)
versão On-line ISSN 2078-676X
versão impressa ISSN 1562-8264
South. Afr. j. crit. care (Online) vol.38 no.1 Pretoria Mar. 2022
http://dx.doi.org/10.7196/SAJCC.2022.v38i1.484
RESEARCH
A randomised controlled trial of intracuff lidocaine and alkalised lidocaine for sedation and analgesia requirements in mechanically ventilated patients
V K SaingurI; S NaazII;E OzairIII; A AsgharIV
IMD; Dr. Baba Saheb Ambedkar Medical College and Hospital, Rohini, Delhi, India
IIMD; Department of Anesthesiology, All India Institute of Medical Sciences, Patna, India
IIIMD; Department of Anesthesiology, Sri Krishna Medical College and Hospital, Muzaffarpur, India
IVMD; Department of Anatomy, All India Institute of Medical Sciences, Patna, India
ABSTRACT
BACKGROUND. Airway irritation caused by prolonged inflation of endotracheal tube (ETT) cuff results in post-intubation morbidities.
OBJECTIVE. We aimed to study intracuff lidocaine and alkalised lidocaine on sedation or analgesia requirements of patients undergoing mechanical ventilation in the intensive care unit (ICU). The primary outcome was to calculate the total dose of propofol and fentanyl required to obtund the unwanted airway and circulatory reflexes. Secondary outcomes were to determine the frequency and severity of cough and haemodynamic parameters.
METHODS. It was a double-blinded, randomised controlled study in the ICU after emergency laparotomy, in patients aged 20 - 55 years, and classified as American Society of Anesthesiologists (ASA) classes 1E and 2E with tube in situ. Exclusion criteria were patients with body mass index >30 kg/m2, haemodynamic instability, requiring positive end-expiratory pressure >7 cm H2O, and a history of chronic obstructive pulmonary disease. After ethics clearance and written consent, patients were randomly assigned into two groups (36 in each), Group L (ETT cuff inflated with lidocaine 2%) and Group AL (cuff inflated with a mixture of lidocaine 2% and sodium bicarbonate 1:1).
RESULTS. Mean dose of propofol consumed in Group AL was significantly less than that in Group L (p<0.001). The mean standard deviation (SD) fentanyl utilisation in Group AL was 1 323.61 (187.27) μ& and that in Group L was 1433.09 (42.58) μg (p=0.040). Group L patients had a significantly higher incidence of cough than those in Group AL (p=0.01). There was no significant difference in the mean arterial pressure (p=0.22), although heart rate was significantly higher in Group L (p<0.001).
Conclusions. Alkalised lidocaine reduces the requirement of sedation, analgesia, and the incidence of cough in intubated patients maintaining haemodynamic stability when compared with lidocaine.
Keywords:lidocaine, propofol, artificial respiration, fentanyl, cough, sodium bicarbonate.
Airway irritation and inflammation caused by prolonged inflation of the endotracheal tube (ETT) cuff results in post-intubation morbidities such as sore throat, dysphagia, hoarseness of voice, severe cough, and pulmonary aspiration.[1, 2] ETT presence is a cause of pain and discomfort in mechanically ventilated intensive care unit (ICU) patients. A significant amount of sedatives and analgesics are given to alleviate this. However, the cumulative effects of prolonged use of these drugs prolong the ICU length of stay and morbidity, such as respiratory muscle weakness, which increases patient-ventilator asynchrony and cough, which has been shown to result in potentially dangerous hyperdynamic responses such as hypertension, tachycardia, dysrhythmias, increased intraocular pressure, increased intracranial pressure, wound dehiscence, and bronchospasm.[3] Cough, as a result of stretch receptors locatedthroughout the inner circumference of the trachea and just below the epithelium, is stimulated by irritants such as an ETT.
To reduce the morbidities associated with mucosal irritation due to the ETT, different methods, including high-volume and low-pressure cuffed ETTs, smaller ETT size, topical application of lubricant jellies, administration of opioids, fluticasone, intravenous (IV) dexmedetomidine and injection of IV lidocaine, have been used. ETT cuffs filled with lidocaine have been proposed.[4-6]
Lidocaine has long been used to obtund the unwanted airway and circulatory reflexes. It may be administered by IV injection, endotracheal cuff inflation, intratracheal (IT) instillation, tube lubrication, or in aerosolised form.[1,7] When lidocaine is injected into the ETT cuff, it spreads through the semipermeable membrane wall and induces an anaesthetic action in the trachea. It is not known whether cough suppression from tracheal instillation of lidocaine acts by local action or by systemic absorption. If local, its action on airway reflexes should last longer than an IV injection.[8] Only the non-ionised base form of the drug diffuses across the semipermeable hydrophobic polyvinyl chloride walls of the ETT cuff.[9]
Increasing the alkalinity of the local anaesthetic using sodium bicarbonate (NaHCO3) increases the pH of the solution and can predictably increase the percentage of the non-ionised fraction of the drug, thus dramatically increasing its diffusion through the ETT cuff.[10] A previous study has shown that when the ETT cuff is filled with lidocaine, a small amount of lidocaine diffuses slowly across the cuff.[11] The addition of NaHCO3 increases diffusion. Therefore, we aimed to study the effect of intracuff lidocaine and alkalised lidocaine on sedative or analgesic requirements in patients undergoing mechanical ventilation in the ICU.
The primary outcome was to calculate the total dose of propofol and fentanyl required to obtund the unwanted airway and circulatory reflexes caused by the ETT cuff. The secondary outcomes were to assess the frequency and severity of cough and haemodynamic parameters (heart rate (HR), mean arterial pressure (MAP), and central venous pressure (CVP)) of patients.
Methods
This double-blind, randomised controlled study was conducted in a tertiary care hospital between January 2016 and July 2017. Seventy-two patients, aged 20 - 55 years, who were admitted to the surgical ICU after emergency laparotomy with the tube in situ, fulfilling criteria for American Society of Anesthesiologists (ASA) class 1E and 2E (class 1 and 2 that needed emergency surgery) and with an expected prolonged mechanical ventilation time, were considered for the study recruitment. Exclusion criteria were body mass index more than 30 kg/m2, tracheostomised patients, haemodynamic instability, positive end-expiratory pressure (PEEP) >7 cm H2O, excessive respiratory secretions, and a history of chronic obstructive pulmonary disease, and cardiovascular, hepatic, or renal disease. Patients were excluded from the study after enrolment if muscle relaxation was needed during ventilation.
After getting clearance from the ethics committee of the institute (ref. no. L. No. 476/UPUMS/Dean/2018-19/E.C. No. 2017/126) and well-explained written consent from patients' attendants (https://www.samedical.org/file/1802), we randomly assigned patients to two groups of 36 patients each, Group L (ETT cuff inflated with lidocaine 2%), and Group AL (cuff inflated with a mixture of lidocaine 2% and 8.4% NaHCO3 in 1:1 ratio), by using the computer-generated sequential number and closed-envelope method. The fluid to be instilled in the ETT cuff was prepared in 10 ml syringes by someone independent of the study.
The ETT cuff was filled with either lidocaine or lidocaine with NaHCO3 8.4% in a 1:1 ratio in an amount that would not cause a leak. Patients were ventilated on volume-controlled synchronised intermittent mandatory ventilation mode, and ventilator settings were adjusted to achieve a tidal volume of 6 - 8 ml/kg, PEEP adjusted to maintain partial oxygen pressure (PaO2) >90% but maintained below 7 cm H2O with a fraction of inspired oxygen (FiO2) <0.6.
We maintained the sedation level to achieve a Riker's sedation agitation scale (SAS) score of 3 - 4 with baseline infusion of injected propofol at the rate of 0.2 - 1 mg/kg/h and maintained infusion of fentanyl at 25 - 100 μg/h to achieve a score of 0 - 1 on the 10-point nonverbal pain scale.[12,13] Level of sedation and haemodynamic parameters were monitored hourly. Propofol and fentanyl infusion was initially at the lowest dose. If at any time it was assessed that levels of pain and sedation score were outside the target level, the target levels were achieved by altering the infusion rates. Reversible causes of anxiety and agitation, excessive light or sounds, cough related to suctioning of ETT, and airway obstruction, were excluded prior to titration of propofol and fentanyl infusions. Subsequently propofol was titrated at 5 mg/h, and fentanyl at 25 μg/h until the target scores were achieved. Total requirements for propofol and fentanyl were recorded during the first 24 hours of mechanical ventilation. Coughing episodes not related to endotracheal suctioning were counted and estimated according to the number of bouts of coughing on a three-point scale (1: mild; 2: moderate; and 3: severe). Adequate ventilation was assessed by hourly arterial blood gas (ABG) interpretation.
To determine the effect of ETT cuff inflation with alkalised lidocaine we estimated 30 patients per group using 80% power, and an alpha error as 0.05. The difference between the mean analgesic requirements was considered for sample size estimation from the study done by Basuni.[14] Estimating a dropout rate of 20%, we included 36 patients in each group.
Data were analysed using SPSS version 16.0 (SPSS Inc, USA) and were presented as mean and standard deviation (SD) or frequencies (%). A parametric test (independent sample t-test) was used for determining any difference between the means of two groups for a particular variable. Repeated measures analysis of variance (ANOVA) was used to determine any difference in the basic monitoring profile and amount of drug required at different time intervals (hourly) of individuals in both groups. A p-value <0.05 was considered as statistically significant, and a p-value <0.001 as highly significant.
Results
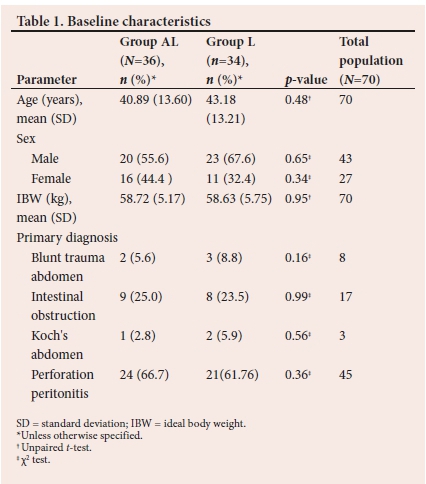
In Group AL results for 36 patients were analysed, while in Group L (n=34) 2 patients were excluded from the study because of the need for neuromuscular blockade for adequate ventilation. There was no significant difference in the age, sex, and ideal body weight between the groups (Table 1). No significant difference in the number of patients with various diagnoses was seen.
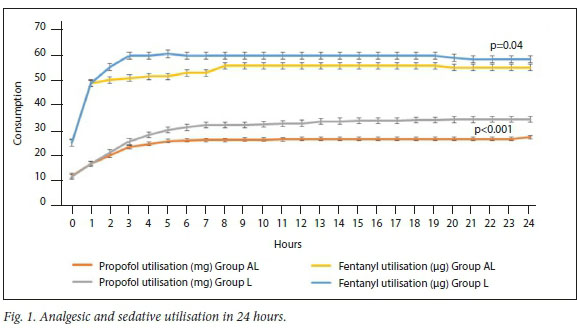
The mean (SD) dose of propofol utilised in Group L (766.32 (136.77) mg) was significantly higher than that in Group AL (624.25 (80.36) mg) (p<0.001). The mean (SD) fentanyl utilisation in Group L was also significantly higher (1433.09 (42.58) μg) than that in the Group AL (1323.61 (187.27) μg) (p=0.040) (Fig. 1).
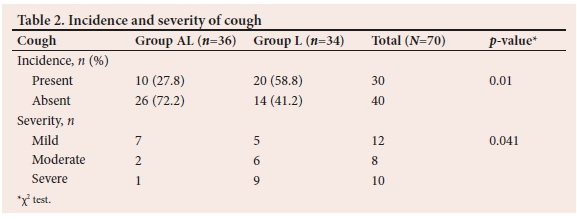
The number of patients with cough in Group L was significantly higher than that in Group AL (p=0.01) (Table 2). Of the patients with cough, the majority (7 out of 10) had a mild cough in Group AL (70%). The incidence of cough according to severity was significantly more in Group L patients as compared with Group AL (p=0.04).
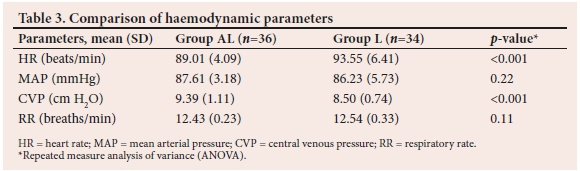
The mean HR in Group L was significantly higher than that in Group AL (p<0.001). There was no significant difference in MAP between the groups (p=0.22). Mean CVP in Group AL (9.39 (1.11) mmHg) was significantly higher than that in Group L (8.50 (0.74) mmHg) (p<0.001). Mean respiratory rates (RRs) were comparable (p=0.11) (Table 3)
There was no significant difference in pH, PaO2 and PaCO2 between groups (Table 4).
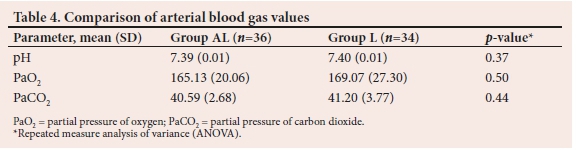
pH was comparable in both groups (p>0.05). There were also insignificant differences between the findings of PaO2 (p=0.50) and PaCO2 (p=0.44) between the groups (Table 4).
Discussion
Use of lidocaine with or without the addition of NaHCO3 (i.e. alkalisation) in the ETT cuff instead of air has been studied during general anaesthesia for a long time. However, the same procedure for the purpose of decreasing the requirement of sedation and analgesia has been evaluated less in ICU patients.[8,15] Hence we undertook this study in the ICU.
Basuni[14] in 2014, reported significant reduction in propofol and sedation requirements in mechanically ventilated patients utilising intracuff alkalised lidocaine compared with those on intracuff air. Results of this study showed that the requirement of propofol and sedation was significantly reduced in patients in whom alkalised lignocaine was used.[15] In our study, too, alkalised lidocaine reduced the sedative or analgesic requirements, although our comparison was with plain lidocaine.
Estebe et al.[15]in 2005 reported a decrease in the sedation and analgesia requirements with alkalised lidocaine in the ETT cuff. We also observed a reduced requirement of sedatives and analgesics when alkalised lidocaine was used in the ETT cuff. According to their study, lidocaine alone had a low diffusion rate across the ETT cuff. The addition of NaHCO3 to lidocaine alkalinises the solution. This provides the hydrophobic base and allows the diffusion of this uncharged form through the polyvinylchloride wall of the cuff more readily than occurs with lidocaine. Owing to more diffusion of alkalised lidocaine from the cuff, tube tolerance in patients should increase, and this might be the reason for the decrease in sedation and analgesia requirements.[16]
The incidence of cough was significantly lower in Group AL and when present was significantly milder than in Group L. Navarro et al.[9] in 2007 conducted a study to evaluatethe effect and safety of filling the ETT cuff with alkalised lidocaine in comparison with air. They found that the alkalisation of lidocaine improves the diffusion across the cuff, and the incidence of cough, sore throat, and tube intolerance were significantly less in patients in the alkalised lidocaine group in comparison with those in the air group.[9] Findings of this study are consistent with our study.
In the study by Basuni,[14] cough was reported as significantly less in the alkalised lidocaine group, and of all patients who had a cough, a significantly higher number had a mild cough.[14] These findings are in concurrence with our findings where the alkalised lidocaine group had less incidence of cough, and the majority of them had a mild cough.
In 2015 Salman et al.[16]conducted a study to compare the effects of intracuff plain lidocaine, alkalised lidocaine, and air. They found that the incidence of cough was least in the intracuff alkalised lidocaine group and highest with intracuff air. Findings of this study were in concurrence with our study.[17]
Acharya et al.[12]in 2016 conducted a study to compare the effect of air and alkalised lidocaine in postoperative sore throat and cough. They found that the incidence of cough was significantly less in the alkalised lidocaine group.[12] In our study, alkalised lidocaine decreased the incidence of coughing, although we compared it with plain lidocaine. MAP was comparable in both groups (p=0.22) in our study. Rashmi et al.[17]in 2017 compared the incidence of sore throat and other haemodynamic parameters using intracuff lidocaine (2%), alkalised lidocaine, and ketamine. The study showed that all three cause haemodynamic stability; however, alkalised lidocaine and ketamine were better than lidocaine.[17]
In Salman et al.'s[16] study, comparing haemodynamic parameters of plain lidocaine and alkalised lidocaine, they found there was no significant difference in the MAP of both groups. The findings of this study were in concurrence with our study.
Mean HR was significantly lower in Group AL than in Group L, as it speaks directly to the reasons, i.e. analgesia and tube tolerance (p<0.001). The mean CVP of the patients of Group AL was significantly higher than that in group L patients (p<0.001). This finding might be due to the higher utilisation of propofol in Group L, as propofol causes vasodilation and decreases the peripheral vascular resistance, which causes peripheral pooling of venous blood and reduced venous return. These parameters in this context have not been reported in the current literature.
The mean RRs in both groups of patients were similar. This is probably explained by a consistent targeted level of sedation.
Study limitations
The main limitation in this study is that it is a single-centre study, and may therefore not be representative of broader general populations. The second limitation is that patients had comorbidities and these were not case-matched after randomisation.
Further, the study excluded elderly patients and patients with obesity, and therefore findings cannot be considered in these phenotypes.
Conclusions
Alkalised lidocaine reduces the requirement of sedation and analgesia in mechanically ventilated patients in the ICU and reduces haemodynamic abnormality and cough. The findings suggest that intracuff alkalised lidocaine may be a useful method to maintain sedo-analgesia in mechanically ventilated and haemodynamically stable patients.
Declaration. None.
Acknowledgements. None.
Author contributions. VKS: Manuscript writing and literature search. SN and EO: Manuscript editing and literature search AA: Data analysis and manuscript writing.
Funding: None.
Conflicts of interest: None.
References
1. Fagan C, Frizelle HP, Laffey P, Hannon V, Carey M. The effects of intracuff lidocaine on endotracheal-tube-induced emergence phenomena after general anesthesia, Anaesthesia Analg 2000;91:201-205. https://doi.org/10.1097/00000539-200007000-00038 [ Links ]
2. Sumathi P, Shenoy T, Ambareesha M, Krishna HM. Controlled comparison between betamethasone gel and lidocaine jelly applied over tracheal tube to reduce postoperative sore throat, cough, and hoarseness of voice. Br J Anaesth 2008;100:215-218. https://doi.org/10.1093/bja/aem341 [ Links ]
3. Rafiei MR, Arianpour N, Rezvani M, Ebrahimi A. Effects of intracuff dexamethasone on post-extubation reactions. J Res Med Sci 2012;17:338. [ Links ]
4. Jensen PJ, Hommelgaard P, Sondergaard P, Eriksen S. Sore throat after operation: Influence of tracheal intubation, intracuff pressure and type of cuff. Br J Anaesth 1982;54:453-457. https://doi.org/10.1093/bja/54.4.453 [ Links ]
5. Stout DM, Bishop MJ, Dwersteg JF, Cullen BF. Correlation of endotracheal tube size with sore throat and hoarseness following general anesthesia. Anesthesiology 1987;67:419-421. https://doi.org/10.1097/00000542-198709000-00025 [ Links ]
6. Guler G, Akin A, Tosun Z, et al. Single-dose dexmedetomidine attenuates airway and circulatory reflexes during extubation. Anaesthesiol Scand 2005;49:1088-1091. https://doi.org/10.1111/j.1399-6576.2005.00780.x [ Links ]
7. Jaichandran VV, Angayarkanni N, Karunakaran C, Bhanulakshmi IM, Jagadeesh V. Diffusion of lidocaine buffered to an optimal pH across the endotracheal tube cuff - An in-vitro study. Indian J Anaesthesia 2008;52:536-534. [ Links ]
8. Tanaka Y, Nishimori M, Sato Y, Furuya H. Lidocaine for preventing postoperative sore throat. Cochrane Database Syst Rev 2009;8:CD004081. https://doi.org/10.1002/14651858.cd004081.pub2 [ Links ]
9. Navarro LHC, Braz JRC, Nakamura G, Lima RM, Silva FP, Módolo NSP. Effectiveness and safety of endotracheal tube cuffs filled air versus filled alkalinised lidocaine: A randomised clinical trial. São Paulo Med J 2007;125:1390. https://doi.org/10.1590/s1516-31802007000600004 [ Links ]
10. Matias E. Effect of NaHCO3 on the diffusion of lignocaine through the wall of endotracheal tube's cuff. Br J Anaesth 1995;74:A.238. [ Links ]
11. Estebe JP, Dollo G, le Corre P, et al. Alkalinisation of intracuff lidocaine improves endotracheal tube-induced emergence phenomena. Anesth Analg 2002;94:227-230. https://doi.org/10.1097/00000539-200201000-00044 [ Links ]
12. Acharya G, Gill RS, Arya PC, Arora KK. Comparision of intracuff lignocaine and air and its related complications. Eur J Pharm Med Res 2016,3(4):382-387. [ Links ]
13. Jawad M, Azeez Alsaady M. Effect of endotracheal tube lidocaine instillation in prevention of smokers emergence coughing: Sample of Iraqi patients undergoing emergency appendectomy. J Intensive Crit Care 2016; 2(22):1-4. https://doi.org/10.18203/2320-6012.IJRMS20161981 [ Links ]
14. Basuni AS. Intracuff alkalised lidocaine reduces sedative/analgesic requirements for mechanically ventilated patients, Saudi J Anesth 2014;8(4):451-455. https://doi.org/10.4103/1658-354x.140816 [ Links ]
15. Estebe JP, Gentili M, le Corre P, Dollo G, Chevanne F. Alkalinisation of intracuff lidocaine: Efficacy and safety. Anesth Analg 2005;101:1536-1541. https://doi.org/10.1213/01.ane.0000180995.24211.89 [ Links ]
16. Salman W, Shamim A, Shounthoo RS, Gul S. A comparative study between intracuff alkalinised lignocaine, intracuff plain lignocaine and intracuff air for decreasing post intubation sore throat and emergence phenomena. J Dental Med Sci 2015;14(10):60-66. https://doi.org/10.9790/0853-141096066 [ Links ]
17. Rashmi NR, Shashidhar GS, Balabhaskar S, Kiranchand N. Comparison of intracuff air, lignocaine, lignocaine with sodium bicarbonate and ketamine for attenuating postoperative sore throat. Int J Anesthesiol 2017;3(1):5-8. [ Links ]
 Correspondence:
Correspondence:
S Naaz
drshaguftanaaz@gmail.com
Accepted 8 November 2021.
Contributions of the study: Alkalised lidocaine when used in endotracheal tube cuff inflation reduces the need for sedation and analgesia in mechanically-ventilated patients, and improves haemodynamic stability.














