Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
Southern African Journal of Critical Care (Online)
versão On-line ISSN 2078-676X
versão impressa ISSN 1562-8264
South. Afr. j. crit. care (Online) vol.37 no.2 Pretoria Ago. 2021
http://dx.doi.org/10.7196/SAJCC.2021.v37i2.481
REVIEW
Guidelines for the hospital role of the clinical nurse in antimicrobial stewardship: A scoping review
J RoutI; S EssackII; P BrysiewiczIII
IMN; OrcID 0000-0002-2100-1980; College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
IIPhD; OrcID 0000-0003-3357-2761; Antimicrobial Research Unit, College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
IIIPhD; OrcID 0000-0001-6258-1603 College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND. Antimicrobial stewardship aims to optimise the use of antimicrobial medicines to preserve the efficacy of these medicines and to contain antimicrobial resistance where possible. Nurses constitute the largest group of healthcare workers; however, the role played by nurses within current antimicrobial stewardship strategies is largely unacknowledged despite nurses being at point-of-care at the hospital bedside.
OBJECTIVE. To identify recommendations for the antimicrobial stewardship role of the bedside nurse in key global antimicrobial stewardship guidelines.
METHODS. Scoping review methodology was used to systematically search published and 'grey' literature in PubMed, EBSCOhost, Google Scholar, government websites, and websites of professional societies and organisations. Search dates were 1990 to 2020. Inclusion criteria were English language antimicrobial stewardship guidelines for hospitals. Screening was conducted in two stages for title and abstract and then full text relevancy and documented according to the PRISMA Extension for Scoping Reviews.
RESULTS. Of the 1 824 articles that were retrieved, only 43 met the inclusion criteria. Inclusion of the bedside nurse on the antimicrobial stewardship team occurred in 13.9% (n=6) of the papers. A role for the bedside nurse was recommended in antibiotic stewardship (32.5%; n=14), infection prevention and control (23.2%; n=10), and administration of antimicrobial medicines (20.9%; n=9) of reviewed documents. Other recommendations included the use of evidence-based antimicrobial stewardship (20.9%; n=9), collaboration with other healthcare staff (11.6%; n=5), facilitation of transition of care (18.6%; n=8), and nurse prescription of antibiotics (4.6%; n=2).
CONCLUSION. This scoping review highlights a slow but incremental increase in recognition of the role of the bedside nurse within the operational hub of antimicrobial stewardship strategies.
Keywords: antimicrobial stewardship; clinical; guidelines; bedside nurse; role; scoping review.
Antimicrobial stewardship (AMS) is a proactive measure to slow the development of antimicrobial resistance (AMR)[1] through coordinated interventions to improve and measure appropriate use of antimicrobial agents, promote the selection of optimal antimicrobial regimens, and incorporate appropriate dosing, duration and route of administration.^ AMS became familiar in healthcare following the formulation of guidelines (SHEA/IDSA)[3] in response to increasing reports on AMR.[4] Recommendations by expert policy groups were for a multidisciplinary commitment to the goals of AMS,[5] based on rational use of antimicrobial medicines and prevention of the spread of resistance by effective infection prevention and control.[1·6·
Recent literature questions exclusion of nurses in formulating AMS strategies, recommends their inclusion in the AMS team,[7-10] and raises concern that the nurse's role in AMS has not been adequately leveraged.[11-13] AMS forms an important component of patient safety,[6,7] which is unequivocally in the domain of nursing care.[14,15] Advocacy and collaborative roles of nurses in AMS are well understood,[9·16] as is infection prevention and control (IPC);[9,1117] however, other clinical roles of the nurse, of possible importance for preventing and containing AMR, should also be considered.[8,9,1819]
Nursing organisations such as the Royal College of Nursing[20] and the American Nurses Association[21] have released position papers on the role of nurses. A scoping review was therefore conducted to search for other key recommendations (i.e., guidelines, policy statements, position statements, white papers, standards, strategies, protocols, action plans, or briefs) on the role of the bedside nurse in AMS within the hospital setting. Preliminary search of PROSPERO, MEDLINE, the Cochrane Database of Systematic Reviews and the Joanna Briggs Institute Database of Systematic Reviews and Implementation Reports identified no current nor proposed scoping reviews or systematic reviews on the topic. This review title is registered with JBI Systematic Review and Open Science Framework (OSF).
Methods
Study design
Scoping review methodology developed by the Johanna Briggs Institute[22] based on the Arksey and O'Malley framework[23] and further advanced by Levac, Colquhoun and O'Brien,[24 was used to compile the scoping review protocol by the authors guided by the PRISMA Extension for Scoping Reviews (PRISMA-ScR).[25] An iterative team approach was used to follow a series of steps with regular team meetings held to discuss progress and agree on each step. The steps followed were: (i) identifying the research question based on the review objectives; (ii) conducting the search using Boolean operators, and identifying studies within electronic databases, reference lists, hand searches, and grey literature; (iii) selecting relevant studies using inclusion and exclusion criteria; (iv) charting the extracted data; and (v) collating, summarising, reporting the findings according to key themes, and identifying gaps.[22]
Identifying the research question
Consultation with the review team defined the main research question as 'Do key antimicrobial stewardship guidelines and policies include recommendations for the role of a bedside nurse in AMS, and what are these recommendations?' The objectives of the review were to: (i) describe the timeline, origin, and purpose of AMS guidelines; (ii) describe the inclusion of nurses on panels/ committees developing AMS guidelines; (iii) describe recommendations for the inclusion of bedside nurses on hospital AMS teams; and (iv) analyse recommendations for the clinical role and responsibilities of the bedside nurse in AMR and AMS. The nature of the review findings led to a second research question, 'do key antimicrobial stewardship guidelines and policies include recommendations for AMS education for hospital-based clinical nursing practice, and what are these recommendations?', which yielded results and analysis that were too lengthy to include in this manuscript and will therefore be presented in a subsequent manuscript.
Identifying relevant studies
Inclusion and exclusion criteria
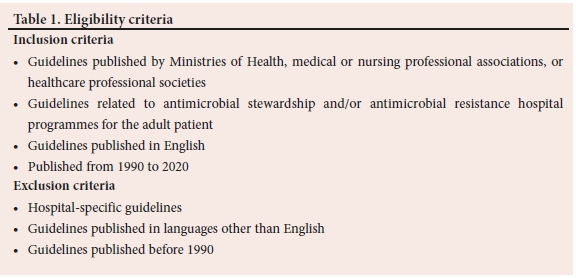
The search strategy considered all published and unpublished (grey literature)[22] English language AMS guidelines from 1990 to 2020, to include documents published before the first known AMS guideline (1997)[3] (Table 1). All documents specific to AMS (incl. recommendations, guidelines, policy statements, position statements, white papers, standards, strategies, protocols, action plans, or briefs) authored by government bodies, national healthcare organisations, interested healthcare societies, medical, pharmacy, and nursing professional bodies were targeted.
Search strategy
Database and manual searches were conducted in 2018 and updated in 2020 using a three-step search strategy:[22](i) a limited PubMed search was conducted to identify articles on the topic; (ii) text words in titles and abstracts, and descriptive index terms of relevant articles were then used to develop a full search strategy using Boolean operators to narrow the search; and (iii) manual searches were performed on relevant websites and reference lists of identified key articles for potentially relevant documents and articles (http://www.sajcc.org.za/public/sup/481.pdf).[26]
The final search strategy including all identified keywords and index terms was adapted for each included information source and electronic literature databases (PubMed and EBSCOhost (academic search complete); CINAHL, Health source, MEDLINE, Nursing/ academic edition) (Table 1: http://www.sajcc.org.za/public/sup/481.pdf).
Study selection
The search yielded 1 824 articles. All identified records were exported to EndNote, version 7.8 (EndNote, USA) to organise titles and abstracts. After removing 1 325 duplicate and irrelevant articles, a two-part selection process was used in which two reviewers excluded 357 ineligible articles during firstlevel screening of titles and abstracts, and 99 articles through second-level full-text screening. Eight documents were referred to a third reviewer for arbitration. Forty-three documents were finally selected following the JBI Population Concept Context (PCC) framework,[27] and inclusion and exclusion criteria. (Table 1): (P)opulation - nurses who practice in an acute hospital setting; (C)oncept - guidelines for clinical nurse practice; (C)ontext - AMS strategies and interventions that have developed to address antimicrobial resistance. The selection process for both searches was documented according to the PRISMA-ScR (http://www.sajcc.org.za/public/sup/481.pdf).[25]
Charting the data
Data were extracted from included papers by two independent reviewers using a data extraction tool developed by the reviewers and tabulated according to authors, organisations/ societies represented, year published, country of origin, and overall goal and objectives of the guideline (Table 2: http://www.sajcc.org.za/public/sup/481.pdf).[27,28] Disagreements arising between the reviewers were resolved through discussion, or third reviewer consultation.[22]
Collating, summarising and reporting results
We applied a common descriptive-analytical framework to the reviews,[22,23] consistent with scoping review methodology using a narrative synthesis to answer the objectives of the study.[29]
Results
Characteristics of included documents
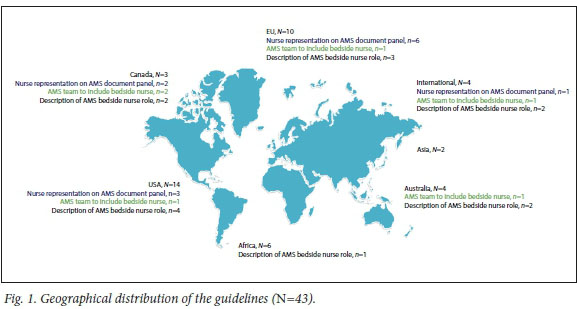
Of the 43 guidelines[1-3,6,20,21,30-66] that were identified, 69.7% (n=30) had recommendations for AMS; the remaining 13 addressed AMR (25.5%; n=11) and appropriate prescribing (4.6%; n=2). No recommendations were found in reviewed guidelines for a role of bedside nurses in AMS until 2014 when the Centers for Disease Control and Prevention released the 'Core elements of hospital antibiotic stewardship programmes' in 2014.[1-In the same year, a nursing document from the Royal College of Nursing (UK) entitled Antimicrobial resistance. RCN position on the nursing contribution' was released (Table 2: http://www.sajcc.org.za/public/sup/481.pdf).[20-In 2017, the American Nurses Association/ CDC workgroup,[21] the Canadian Nurses Association,[54- the European Federation of Nurses Associations,[57] and the International Council of Nurses made further contributions to the recommendations.[58- Most of the reviewed documents originated from North America (39.5%; n=17) (Fig. 1). Documents were from government ministries/departments of health (53.4%; n=23), professional organisations (13.9%; n=6), professional societies (23.2%; n=10), world organisations (4.6%; n=2), and committees and commissions (4.6%; n=2) and were published in professional journals or on their websites. Recommendations for AMS bedside nurse practice were found in 32.5% (n=14) of the documents; USA (9.3%; n=4), EU (6.9%; n=3), Australia (4.6%; n=2), Canada (4.6%; n=2), Africa (2.3%; n=1) and rest of the world (4.6%; n=2) (Fig. 1). More than a tenth of the documents (11.6%; n=5) were from professional nursing organisations (Table 2: http://www.sajcc.org.za/public/sup/481.pdf).
Inclusion of nursing practitioners on panels/ committees
Nurses were represented on 12 panels (27.9%) tasked with developing guidelines (Table 2: http://www.sajcc.org.za/public/sup/481.pdf). Other disciplines involved were from medical specialties (infectious diseases, microbiology, surgery, internal medicine, epidemiology and public health) and pharmacology
Recommendations for the inclusion of nurses on hospital AMS teams
More than two-thirds of the documents (72%; n=31) described AMS team composition; 32.5% (n=14) of these included various nursing categories (the hospital IPC nurse specialist (13.9%; n=6), the bedside nurse (13.9%; n=6), and the hospital nurse manager (4.6%; n=2)) (Table 2: http://www.sajcc.org.za/public/sup/481.pdf).
Recommendations for the AMS clinical role and responsibilities of the bedside nurse
Of the 60.4% (n=26) of the documents that mentioned the role of bedside nurse in AMS, 32.5% (n=14) made recommendations categorised into six groups: infection prevention and control (23.2%; n=10); administering antimicrobial medicines (20.9%; n=9); using evidence-based AMS practices (20.9%; n=9); collaboration with other healthcare staff (11.6%; n=5); facilitating transitions of care (18.6%; n=8); and nurse prescription of antibiotics (4.6%; n=2) (Table 2).
Discussion
The results demonstrate that key AMS guidelines by various government and health professional bodies have either not specified recommendations to guide bedside nursing practice in the prevention and containment of AMR by AMS or have only recently engaged with the issue.
Characteristics of included documents
Key documents placed in the public domain by professional bodies should reflect the evolutionary development of organisational thinking influenced by current research and advances in a particular area.[67]
Internal organisational agreement is indicated by publication of documents such as guidelines, position papers and standards, and the conclusion drawn that information therein accurately represents a consensus view deemed important enough to communicate to others outside the organisation.[67] A professional body maintains oversight of the knowledge, skills, conduct and practice of its individual members within the profession.[68] The 43 guideline documents[1-3,6,20,21,30-66] in this scoping review therefore reflect the various organisations' views on specific AMS measures. It was not always possible to determine the type of nursing representation noted on the AMS panels/committees tasked with formulating the reviewed guidelines, and only four of the 12 panels/committees with nurse representation gave recommendations for the inclusion of the bedside nurse on AMS teams,[21,48,54,58] three of which were nursing organisations (Table 2).[21,54,58] 'Governments and decision-making bodies need to understand that including nurses in their deliberation is not a 'nice to do' but a 'must do' because of the knowledge and practice that nursing brings to this burning agenda.'[18]
Inclusion of nurses on the hospital AMS team
Historically, AMS has been the responsibility of physicians and pharmacists with infectious diseases/antimicrobial stewardship training, and frontline nurses have not always been formally engaged to perform AMS activities. The earliest identified AMS guideline describes a team comprising a microbiologist, pharmacist, infection-control practitioner, and hospital epidemiologist dedicated to the control of AMR.[3] AMS was therefore considered to be multidisciplinary from its inception. Although there is strong support for a multidisciplinary approach to AMR in the guidelines, only a third of the reviewed documents recommended inclusion of nurses within the AMS team, and these even were only initially for primary healthcare (PHC) and IPC specialist nurse categories. Recommendations for inclusion of bedside nurses on AMS teams only appeared within the reviewed guidelines from 2016 onwards (Table 2: http://www.sajcc.org.za/public/sup/481.pdf).[21,48,54,56,58,61] This may be due to the medical focus of early AMS guidelines from North America[3,4] that emphasised 'medical staff' function rather than a hospital function within strategy formation and execution and seems to have become entrenched in subsequent guidelines for development and implementation of AMS programmes.[1,6,44] Unfortunately, this has been perpetuated in medical AMS literature.[69]
'Nurse's exclusion from ASPs has created an environment in which antimicrobial management is considered outside the remit of nursing responsibilities and expertise, which essentially has disempowered healthcare institutions from taking a true multidisciplinary approach to preventing AMR.'[70] More recently, an international consensus group (2018) recommended the use of all available expertise on AMS teams including nurses where possible.[71] This better supports a culture of AMS within the hospital and is a necessity if AMR is to be addressed successfully.
Challenges to inclusion of the bedside nurse on AMS teams
Although there is strong support in AMS literature that nurses should be included on AMS committees and teams, and involved in AMS goals and development, and review and implementation of organisational policies advancing AMS strategies, this has been slow to emerge in practice.[7,8,11,12,14,18,72,73] Analysis of the implementation of AMS interventions within AMS toolkits, 'TARGET and Start Smart-Then Focus',[74] indicates that nurse representation on AMS committees in NHS trusts remains low (47%). A survey of 35 IPC leaders (managers, directors and administrators),[75] responsible for the standardisation of IPC surveillance systems, policies, practices, products and processes across multihospital systems, found that IPC nurse specialists (96%), within the hospital setting, were more likely than bedside registered nurses (RNs) (54%) to be members of the AMS team, and to receive more feedback from the AMS programme; this may reflect perceptions of AMS falling within the ambit of the IPC nurse specialist, rather than that of the bedside nurse. Nurse administrators surveyed across 34 Los Angeles County acute care hospitals, who were requested to describe how bedside RNs participate in AMS, reported minimal inclusion represented by access to an antimicrobial resistance/multidrug-resistant organism advisory group (2.9%), and serving on AMS committee (8.8%), or subcommittees (9%).[76,77] However, RNs within these hospitals were still expected to participate in AMS quality assurance initiatives (26.5%), such as the implementation of antimicrobial 'time-outs' (de-escalation protocol) within these institutions.[76,77] In an observational pilot study conducted in five hospitals that were developing a national AMS registry in the Netherlands,[78] only one hospital included a nurse on the AMS team. The lack of inclusion of the nurse demonstrated by these examples is attributed to profound socio-cultural-professional differences between and within healthcare disciplines, and is thought to considerably influence the dynamics of AMS.[13,79]
Recommendations for the clinical role and responsibilities of the bedside nurse in AMR and AMS
Nursing is the central hub of patient care; however, 'many nurses do not directly see their impact in antibiotic stewardship programmes (ASPs) owing to being omitted from formal ASP guidelines.'[11] Newer versions of the reviewed guidelines demonstrate an expanding role of the hospital-based nurse, with most recommendations outlining a role for nurses within IPC, administration of antimicrobial medicines, evidence-based AMS practices, and facilitating transitions of care. Few recommendations were for nurse collaboration with other healthcare staff, and fewer yet for nurse prescription of antibiotics within the in-patient setting (Table 2). Support for bedside nurse involvement within AMS is growing in multidisciplinary literature,[8,80-85] in particular supporting nurse practice with regard to allergy confirmation,[81] specimen collection for culture,[83] timely antimicrobial initiation,[81,84] appropriate administration,[80,84,85] assessing response to therapy[80,81.84,85] and prompting discussion of de-escalation,[82,84] participating in the intravenous to oral therapy (IV/ PO) switch,[81] patient education[83,84] and assessing suitability for outpatient antimicrobial therapy (OPAT), defined by Norris et al.[86] as the administration of at least two doses of antimicrobial therapy on different days out of the hospital environment).[81]
Support within nursing literature for the AMS role of the bedside nurse has rapidly gained traction during the last 10 years, recognising that many aspects of AMS care throughout the hospital already comprise part of current daily nursing practice.[9,11,15,73] The AMS responsibilities for nurses identified in the literature include: (i) obtaining the patient's allergy history,[10,11,15,16,73] antibiotic initiation, safe and timely administration of antimicrobial treatment,[9,10,11,16,18,19,69,70,73] and monitoring and communicating patient response to antimicrobial therapy[10,11,73] including therapeutic levels;[11,19,70] (ii) implementation of care bundles to minimise hospital-acquired infections,[9] collection of specimens for culture before starting antimicrobial treatment, tracking and communicating sensitivity reporting,[9,16,18,73] monitoring adverse events such as superinfection and resistant infection, and implementing necessary isolation precautions;[11,16,73](iii) participating in de-escalation[9,11] by advocating for 'antibiotic timeout' at 48-hour intervals when antimicrobial treatment is reviewed,[11,15,16,87] and initiating conversion from IV/PO switch;[10,11,15,16,70,87](iv) provision of patient education;[10,11,16,18] and (v) assessing patient suitability for OPAT.[10,70]
Development of the AMS role and responsibilities of the bedside nurse
AMS by its very structure and implementation is multidisciplinary and nursing involvement within AMS is recognised as a necessity if AMR is to be addressed.[1,9,11,15,18,58,80,88] 'Ideally, the gold standard for AMS would be nurses at the bedside who promote responsible, targeted antibiotic use by being able to identify the patients' pathogen, verify that the pathogen is sensitive to the prescribed antibiotic, communicate discrepancies with the multidisciplinary team and provide appropriate interventions and patient education.'[16] AMR is viewed as a critically important research topic by the WHO (2001),[89] and although research into the clinical nursing role is growing, continued definition of this role is needed. [11,18,75-77,88] AMR should be viewed by all healthcare professionals in all healthcare settings as relevant to their specific disciplines,64 using a multi-disciplinary collaborative approach between all members of the healthcare team to meet AMS goals.[1,8,9,11,18,19,73,88,90-92] This is particularly important as global healthcare interrogates AMR within the added burden of COVID-19.[93,94] Failure to recognise those responsible for direct patient care is an oversight[12,14] that may impact the success of AMS. Healthcare professional organisations must recognise that stewardship reaches beyond the responsibilities of the prescriber, adding the efforts of the bedside nurse to those of infectious disease clinicians, pharmacists, microbiologists, hospital epidemiologists, and IPC specialists.[12,21,54,64,73,80,92,95]
Study limitation
We decided to include only recommendations indicated specifically for nurses within the hospital setting; guidelines that included this role within general recommendations to healthcare professionals might have been excluded unless it was stated that recommendations were aimed at all healthcare workers. Guidelines published in languages other than English were excluded. Search terms which were entered as plurals may also be a potential limitation.
Conclusion
The bedside nurse is central to effective organisation and communication within AMS strategies monitoring compliance with best practice and influencing prescribing decisions. Despite the worldwide implementation of AMS in the past 20 years, recognition of the bedside nurse has been slow to emerge in influential AMS guidelines, perhaps reflecting a time lag in the inclusion of recent evidence. This review demonstrated that policy recommendations for the inclusion of nurses on hospital AMS teams and within AMS programmes are minimal, with insufficient attention given to the role of the bedside nurse. Nursing as the discipline closest to the patient with an established patient advocacy role, should be recognised as the communication and operational hub within AMS strategies, and the practical management of antimicrobial drugs should be given the same focus as their prescription. AMS is not a medical function, but a hospital function, and as such should leverage the competencies and skills of all healthcare workers in efforts to contain AMR.
Declaration. None.
Acknowledgements. None.
Author contributions. JR, SE and PB conceptualised the manuscript. JR analysed the data and wrote the manuscript. SE and PB analysed the data and revised the manuscript. All authors approved the final version of the manuscript for publication.
Funding. None.
Conflicts of interest. None.
References
1. Centers for Disease Prevention and Control. Core elements of hospital antibiotic stewardship programs. Atlanta: CDC, 2014. https://www.cdc.gov/antibiotic-use/healthcare/implementation/core-elements.html (accessed 10 June 2018). [ Links ]
2. Society for Healthcare Epidemiology of America; Infectious Diseases Society of America; Pediatric Infectious Diseases Society. Policy statement on antimicrobial stewardship by the Society for Healthcare Epidemiology of America (SHEA), the Infectious Diseases Society of America (IDSA), and the Pediatric Infectious Diseases Society (PIDS). Infect Control Hosp Epidemiol 2012;33(4):322-327. https://doi.org/10.1086/665010 [ Links ]
3. Shlaes D, Gerding D, John J, et al. Society for Healthcare Epidemiology of America and Infectious Diseases Society of America Joint Committee on the Prevention of Antimicrobial Resistance: Guidelines for the prevention of antimicrobial resistance in hospitals. Clin Infect Dis 1997;25(3):584-599. https://doi.org/10.1086/513766 [ Links ]
4. Marr J, Moffet H, Kunin C. Guidelines for improving the use of antimicrobial agents in hospitals: A statement by the Infectious Diseases Society of America. J Infect Dis 1988;157(5):869-876. https://doi.org/10.1093/infdis/157.5.869 [ Links ]
5. Avorn J, Barrett J, Davey P. Antibiotic resistance: Synthesis of recommendations by expert policy groups. Geneva: WHO, 2001. [ Links ]
6. Dellit T, Owens R, McGowan J, et al. Guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis 2007;44(2):159-177. https://doi.org/10.1086/510393 [ Links ]
7. Manning M, Pfeiffer J, Larson E. Combating antibiotic resistance: The role of nursing in antibiotic stewardship. Am J Infect Control 2016;44(12):1454-1457. https://doi.org/10.1016/j.ajic.2016.06.023 [ Links ]
8. Schellack N, Pretorius R, Messina A. 'Esprit de corps': Towards collaborative integration of pharmacists and nurses into antimicrobial stewardship programmes in South Africa. S Afr Med J 2016;106(10):973-974. https://doi.org/10.7196/SAMJ.2016.v106i10.11468 [ Links ]
9. Rout J, Brysiewicz P. Exploring the role of the ICU nurse in the antimicrobial stewardship team at a private hospital in KwaZulu-Natal, South Africa. South Afr J Crit Care 2017;33(2):46-50. https://doi.org/10.7196/SAJCC.2017.v33i2.331 [ Links ]
10. Padigos J, Ritchie S, Lim G. Nurses have a major role to play in antimicrobial stewardship. Kai Tiaki Nurs New Zealand 2018;23(11):16-18. [ Links ]
11. Olans R, Olans R and DeMaria A. The critical role of the staff nurse in antimicrobial stewardship - unrecognised, but already there. Clin Infect Dis 2016;62(1):84-89. https://doi.org/10.1093/cid/civ697 [ Links ]
12. Castro-Sánchez E, Bennasar-Veny M, Smith M, et al. European Commission guidelines for the prudent use of antimicrobials in human health: A missed opportunity to embrace nursing participation in stewardship. Clin Microbiol Infect 2018;24(8):914-915. https://doi.org/10.1016/j.cmi.2018.02.030 [ Links ]
13. Charani E, Smith I, Skodvin B, et al. Investigating the cultural and contextual determinants of antimicrobial stewardship programmes across low-, middle- and high-income countries: A qualitative study. PLoS ONE 2019;14(1):e0209847. https://doi.org/10.1371/journal.pone.0209847 [ Links ]
14. Olans R, Nicholas P, Hanley D, et al. Defining a role for nursing education for staff nurse participation in antimicrobial stewardship. J Contin Educ in Nurs 2015;46(7):318-321. http://dx.doi.org/10.3928/00220124-20150619-03 [ Links ]
15. Monsees E, Tamma P, Cosgrove S, et al. Integrating bedside nurses into antibiotic stewardship: A practical approach. Infect Control Hosp Epidemiol 2019;40(5):579-584. https://doi.org/10.1017/ice.2018.362 [ Links ]
16. Sumner S, Forsyth S, Collette-Merrill K, et al. Antibiotic stewardship: The role of clinical nurses and nurse educators. Nurse Educ Today 2018;60:157-160. https://doi.org/10.1016/j.nedt.2017.10.011 [ Links ]
17. Castro-Sánchez E, Drumright L, Gharbi M, et al. Mapping antimicrobial stewardship in undergraduate medical, dental, pharmacy, nursing and veterinary education in the United Kingdom. PLoS One 2016;11(2):e0150056. https://doi.org/10.1371/journal.pone.0150056 [ Links ]
18. Ellen M, Hughes F, Shach R. How nurses can contribute to combating antimicrobial resistance in practice, research and global policy. Int J Nurs Stud 2017;71:A1-A3. https://doi.org/10.1016/j.ijnurstu.2017.02.023 [ Links ]
19. Rout J, Essack S, Brysiewicz P. Are nursing infusion practices delivering full-dose antimicrobial treatment? J Antimicrob Chemother 2019;74(12):3418-3422. https://doi.org/10.1093/jac/dkz365 [ Links ]
20. Royal College of Nursing. Antimicrobial resistance. RCN position on the nursing contribution. London: RCN, 2014. https://www.nric.org.uk/node/52607. [ Links ]
21. American Association of Nurses. White paper: Redefining the antibiotic stewardship team: Recommendations from the American Nurses Association/Centers for Disease Control and Prevention Workgroup on the Role of Registered Nurses in Hospital Antibiotic Stewardship Practices. Maryland: AAN, 2017. https://www.cdc.gov/antibiotic-use/healthcare/pdfs/ANA-CDC-whitepaper.pdf (accessed 30 July 2018). [ Links ]
22. Joanna Briggs Institute. Methodology for JBI scoping reviews. Joanna Briggs Institute reviewer's manual. Adelaide: JBI, 2015. https://nursing.lsuhsc.edu/JBI/docs/ReviewersManuals/Scoping-.pdf [ Links ]
23. Arksey H, O'Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Meth 2005;8(1):19-32. https://doi.org/10.1080/1364557032000119616 [ Links ]
24. Levac D, Colquhoun H, O'Brien K. Scoping studies: Advancing the methodology. Implement Sci 2010;5(1):1-9. https://doi.org/10.1186/1748-5908-5-69 [ Links ]
25. Tricco A, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern 2018;169(7):467-473. https://doi.org/10.7326/M18-0850 [ Links ]
26. Pham M, Rajic A, Greig J, et al. A scoping review of scoping reviews: Advancing the approach and enhancing the consistency. Res Synth Methods 2014;5(4):371-385. https://doi.org/10.1002/jrsm.1123 [ Links ]
27. Peters M, Godfrey C, Khalil H, et al. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc 2015;13(3):141-146. https://doi.org/10.1097/XEB.0000000000000050 [ Links ]
28. Cacchione P. The evolving methodology of scoping reviews. Clin Nurs Res 2016;25(2):115-119. https://doi.org/10.1177/1054773816637493 [ Links ]
29. Peters M, Godfrey C, McInerney P, et al. Guidance for the conduct of JBI scoping reviews. JBI Reviewer's Manual, 2017. https://wiki.joannabriggs.org/display/MANUAL/Chapter+11%3A+Scoping+reviews (accessed 20 June 2018). [ Links ]
30. Nathwani D. Antimicrobial prescribing policy and practice in Scotland: Recommendations for good antimicrobial practice in acute hospitals. J Antimicrob Chemother 2006;57(6):1189-1196. https://doi.org/10.1093/jac/dkl137 [ Links ]
31. Strategy for the Control of Antimicrobial Resistance in Ireland. SARI Annual Report. 2007. https://www.hpsc.ie/a-z/microbiologyantimicrobialresistance/strategyforthecontrolofantimicrobialresistanceinirelan dsari/sariannualreports/File,3202,en.pdf (accessed 30 July 2018). [ Links ]
32. Drew R, White R, MacDougall C, et al. Insights from the Society of Infectious Diseases Pharmacists on antimicrobial stewardship guidelines from the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Pharmacotherapy 2009;29(5):593-607. https://doi.org/10.1592/phco.29.5.593 [ Links ]
33. Strategy for the Control of Antimicrobial Resistance in Ireland. Guidelines for antimicrobial stewardship in hospitals in Ireland. 2009. https://www.hpsc.ie/a-z/microbiologyantimicrobialresistance/infectioncontrolandhai/guidelines/File,4116,en.pdf (accessed 30 July 2018). [ Links ]
34. Duguid M, Cruikshank M. Antimicrobial stewardship in Australian hospitals. Australian Commission on Safety and Quality in Healthcare 2011. https://www.safetyandquality.gov.au/sites/default/files/migrated/Antimicrobial-stewardship-in-Australian-Hospitals-2011.pdf (accessed 30 July 2018). [ Links ]
35. Spellberg B, Blaser M, Guidos R, et al. Combating antimicrobial resistance: Policy recommendations to save lives. Clin Infect Dis 2011;52(Suppl 5):S397-S428. https://doi.org/10.1093/cid/cir153 [ Links ]
36. Teng C, Lee W, Yeo C, et al. Guidelines for antimicrobial stewardship training and practice. Ann Acad Med Singapore 2012;41(1):29-34. [ Links ]
37. Public Health England. Antimicrobial prescribing and stewardship competencies. London: PHE, 2013. https://www.gov.uk/government/publications/antimicrobial-prescribing-andstewardshipcompetencies (accessed 30 July 2018). [ Links ]
38. National Department of Health. Antimicrobial resistance national strategy framework 2014 -2024. Pretoria: NDoH, 2014. https://www.health-e.org.za/.../2015/.../Antimicrobial-Resistance-National-Strategy-Fram (accessed 30 July 2018). [ Links ]
39. Ministry of Health. Protocol on antimicrobial stewardship program. Putrajaya: MoH, 2014. www.moh.gov.my/.../554756755a584a69615852686269394859584a706379425159 (accessed 30 July 2018). [ Links ]
40. National Department of Health. Implementation plan for the antimicrobial resistance strategy framework in South Africa: 2014 -2019. Pretoria: NDoH, 2015. www.health.gov.za/.../antimicrobial-resistance?...implementation-plan-for-the-antimic... (accessed 30 July 2018). [ Links ]
41. Department of Health. Antimicrobial stewardship policy. Canberra: DoH, 2015. http://www.safetyandquality.health.wa.gov.au/home/index.cfm (accessed 30 July 2018). [ Links ]
42. World Health Organization. Global action plan on antimicrobial resistance. Geneva: WHO, 2015. http://www.emro.who.int/health-topics/drug-resistance/global-action-plan.html (accessed 5 November 2017). [ Links ]
43. Communicable and Infectious Disease Steering Committee (CIDSC). Task group on antimicrobial use stewardship - executive summary. Ottawa: Pan-Canadian Health Public Network, 2016. http://www.phn-rsp.ca/pubs/anstew-gestan/pdf/pub-eng.pdf (accessed 30 July 2018). [ Links ]
44. Barlam T, Cosgrove S, Abbo L, et al. Implementing an antibiotic stewardship program: Guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis 2016;62(10):e51-e77. https://doi.org/10.1093/cid/ciw118 [ Links ]
45. National Department of Health. Antimicrobial resistance - background document. Pretoria: NDoH, 2016. https://www.fidssa.co.za/Content/Documents/AMR_Background_document_FINAL_March15.pdf (accessed 30 July 2018). [ Links ]
46. National Department of Health. A practical guide to antimicrobial stewardship in South Africa. Pretoria: NDoH, 2016. http://www.health.gov.za/index.php/antimicrobial-resistance (accessed 30 July 2018). [ Links ]
47. De With K, Allerberger F, Amann S, et al. Strategies to enhance rational use of antibiotics in hospital: A guideline by the German Society for Infectious Diseases. Infection 2016;44(3):395-439. https://doi.org/10.1007/s15010-016-0885-z [ Links ]
48. HealthCare CAN and National Collaborating Centre for Infectious Diseases. Putting the pieces together: A national action plan on antimicrobial stewardship. 2016. www.healthcarecan.ca/.../Putting%20the%20Pieces%20Together%20-%20Final%20V (accessed 30 July 2018). [ Links ]
49. Healthcare Infection Control Practices Advisory Committee. Antibiotic stewardship statement for antibiotic guidelines - recommendations from HIPAC. Atlanta: CDC, 2016. https://www.cdc.gov/hicpac/pdf/antibiotic-stewardship-statement.pdf (accessed 30 July 2018). [ Links ]
50. Levy Hara G, Kanj S, Pagani L, et al. Ten key points for the appropriate use of antibiotics in hospitalised patients: A consensus from the Antimicrobial Stewardship and Resistance Working Groups of the International Society of Chemotherapy. Int J Antimicrob Agents 2016;48(3):239-246. https://doi.org/10.1016/j.ijantimicag.2016.06.015 [ Links ]
51. Morgan D, Croft L, Deloney V, et al. Choosing wisely in healthcare epidemiology and antimicrobial stewardship. Infect Control Hosp Epidemiol 2016;37(7):755-760. https://doi.org/10.1017/ice.2016.61 [ Links ]
52. National Institute for Health and Care Excellence. Antimicrobial stewardship. London: NICE, 2016. https://www.nice.org.uk/guidance/qs121/resources/antimicrobial-stewardship-pdf-75545353537477 (accessed 30 July 2018). [ Links ]
53. American Society of Health-System Pharmacists. A hospital pharmacists guide to antimicrobial stewardship. Bethesda: ASHP, 2017. https://www.scribd.com/document/312641269/Stewardship-White-Paper (accessed 30 July 2018). [ Links ]
54. Canadian Nurses Association. Antimicrobial resistance in Canada. Brief for the Standing Committee on Health. Ottawa: CAN, 2017. https://www.cna-aiic.ca/~/media/cna/page-content/pdf-en/antimicrobial-resistance-in-canada-brief-for-the-standing-committee-on-health.pdf?la=en (accessed 30 July 2018). [ Links ]
55. Department of Health. Australia's first national antimicrobial resistance strategy 2015-2019 progress report. Canberra: DoH, 2017. https://www.amr.gov.au/australias-response/national-amr-strategy (accessed 30 July 2018). [ Links ]
56. European Commission. EU guidelines for the prudent use of antimicrobials in human health. Brussels: EU, 2017. https://ec.europa.eu/health/amr/sites/amr/files/amr_guidelines_prudent_use_en.pdf (accessed 30 July 2018). [ Links ]
57. European Federation of Nurses Associations. Nurses are frontline combating antimicrobial resistance. Brussels: EFNA, 2017. http://www.efnweb.be/wp-content/uploads/EFN-AMR-Report-Nurses-are-frontline-combating-AMR-07-11-2017.pdf (accessed 30 July 2018). [ Links ]
58. International Council of Nurses. Position statement. Antimicrobial resistance. Geneva: ICN, 2017. https://www.icn.ch/sites/default/files/inline-files/PS_A_Antimicrobial_resistance.pdf (accessed 30 July 2018). [ Links ]
59. National Department of Health. Guidelines on implementation of antimicrobial stewardship in South Africa: One health approach & governance. Pretoria: NDoH, 2017. www.health.gov.za/.../antimicrobial-resistance?...antimicrobial-stewardship-guidelines... (accessed 30 July 2018). [ Links ]
60. The Joint Commission. New antimicrobial stewardship standard. 2017. https://www.jointcommission.org/assets/1/6/New_Antimicrobial_Stewardship_Standard.pdf_(accessed 30 July2018). [ Links ]
61. Australian Commission on Safety and Quality in Health Care. Antimicrobial stewardship in Australian health care. Sydney: ACSQHC, 2018. https://www.safetyandquality.gov.au/our-work/healthcare-associated-infection/antimicrobial-stewardship/book/ (accessed 30 July 2018). [ Links ]
62. Hawkey P, Warren R, Livermore D, et al. Treatment of infections caused by multidrug-resistant Gram-negative bacteria: Report of the British Society for Antimicrobial Chemotherapy/Healthcare Infection Society/British Infection Association Joint Working Party. J Antimicrob Chemother 2018;73(Suppl 3):iii2-iii78. https://doi.org/10.1093/jac/dky027 [ Links ]
63. Manning M, Septimus E, Dodds Ashley W, et al. Antimicrobial stewardship and infection prevention-leveraging the synergy: A position paper update. Am J Infect Control 2018;46(4):364-368. https://doi.org/10.1016/j.ajic.2018.01.001 [ Links ]
64. World Health Organization. WHO Competency Framework for Health Workers' Education and Training on Antimicrobial Resistance. Geneva: WHO, 2018. https://www.who.int/hrh/resources/WHO-HIS-HWF-AMR-2018.1/en/ (accessed 10 September 2019). [ Links ]
65. Centers for Disease Prevention and Control. The core elements of hospital antibiotic stewardship programs. Atlanta: CDC, 2019. https://www.cdc.gov/antibiotic-use/core-elements/hospital.html (accessed 30 January 2020). [ Links ]
66. Department of Health. Guidelines for the prevention and containment of antimicrobial resistance in South African hospitals. Pretoria: NDoH, 2019. https://www.fidssa.co.za/Content/Documents/2019SAGuidelineAMRHospitals.pdf (accessed 30 January 2020). [ Links ]
67. Lucas L. The evolution of organisations and the development of appropriate knowledge structures. J Knowl Manag 2010;14(2):190-201. [ Links ]
68. Science Council. Definition of a professional body. https://sciencecouncil.org/about-science/our-definition-of-a-professional-body/. (accessed 10 September 2018). [ Links ]
69. Ohl C, Luther V. Health care provider education as a tool to enhance antibiotic stewardship practices. Infect Dis Clin N Am 2014;28(2):177-193. https://doi.org/10.1016/j.idc.2014.02.001 [ Links ]
70. Edwards R, Drumright L, Kieran M, et al. Covering more territory to fight resistance: Considering nurses' role in antimicrobial stewardship. J Infect Prev 2011;12(1):6-10. https://doi.org/10.1177/1757177410389627 [ Links ]
71. Pulcini C, Binda F, Lamkang A, et al. Developing core elements and checklist items for global hospital antimicrobial stewardship programmes: A consensus approach. Clin Microbiol Infect 2018;25(1):20-25. https://doi.org/10.1016/j.cmi.2018.03.033 [ Links ]
72. Broom A, Broom J, Kirby E, et al. Nurses as antibiotic brokers: Institutionalised praxis in the hospital. Qual Health Res 2016;27(13):1924-1935. https://doi.org/10.1177/1049732316679953 [ Links ]
73. Olans R, Olans R, Witt D. Good nursing is good antibiotic stewardship. Am J Nurs 2017;117(8):58-63. https://doi.org/10.1097/01.NAJ.0000521974.76835.e0 [ Links ]
74. Ashiru-Oredope D, Budd E, Bhattacharya A, et al. Implementation of antimicrobial stewardship interventions recommended by national toolkits in primary and secondary healthcare sectors in England: TARGET and Start Smart Then Focus. J Antimicrob Chemother 2016;71(5):1408-1414. https://doi.org/10.1093/jac/dkv492 [ Links ]
75. Manning M, Pogorzelska-Maziarz M. Health care system leaders' perspectives on infection preventionist and registered nurse engagement in antibiotic stewardship. Am J Infect Control 2018;46(5):498-502. https://doi.org/10.1016/j.ajic.2017.10.024 [ Links ]
76. Acute Communicable Disease Control. Survey ofhospital nursing roles in antimicrobial stewardship. Special Studies Report. ACDC 2016;29-34. http://publichealth.lacounty.gov/acd/pubs/reports/SurveyofHospitalNursingRolesin AntimicrobialStewardship.pdf (accessed 10 September 2018). [ Links ]
77. Cavadid C, Sakamoto S, Terashita D, et al. Bedside registered nurse roles in antimicrobial stewardship: A survey of acute-care hospitals in Los Angeles County. Infect Control Hosp Epidemiol 2017;38(10):1263-1265. https://doi.org/10.1017/ice.2017.166 [ Links ]
78. Berrevoets M, ten Oever J, Sprong T, et al. Monitoring, documenting and reporting the quality of antibiotic use in the Netherlands: A pilot study to establish a national antimicrobial stewardship registry. BMC Infect Dis 2017;17(1):1-8. https://doi.org/10.1186/s12879-017-2673-5 [ Links ]
79. Charani E, Holmes A. Antibiotic stewardship - twenty years in the making. Antibiotics (Basel) 2019;8(1):7. https://doi.org/10.3390/antibiotics8010007 [ Links ]
80. Charani E, Holmes A. Antimicrobial stewardship programmes: The need for wider engagement. BMJ Qual Saf 2013;22(11):885-887. https://doi.org/10.1136/bmjqs-2013-002444 [ Links ]
81. Ladenheim D, Rosenbert D, Hallam C, et al. Antimicrobial stewardship: The role of the nurse. Nurs Stand 2013:28(6):46-49. https://doi.org/10.7748/ns2013.10.28.6.46.e7802 [ Links ]
82. Pollack L, Srivasan A. Core elements of hospital antibiotic stewardship programs from the Centers for Disease Control and Prevention. Clin Infect Dis 2014;59(3):S97-S100. https://doi.org/10.1093/cid/ciu542 [ Links ]
83. Dyar O, Huttner B, Schouten J, Pulcini C on behalf of ESCMID Study Group for Antimicrobial stewardship. What is antimicrobial stewardship? Clin Microbiol Infect 2017;23(11):793-798. https://doi.org/10.1016/j.cmi.2017.08.026 [ Links ]
84. Plachouras D, Iosifidis E, Quattrocchi A, et al. European Centre for Disease Prevention and Control. ECDC Technical Report. Proposals for EU guidelines on the prudent use of antimicrobials in humans. Sweden: ECDC, 2017. https://www.ecdc.europa.eu/en/publications-data/proposals-eu-guidelines-prudent-use-antimicrobials-humans (accessed 10 September 2018). [ Links ]
85. Ladenheim D. Role of nurses in supporting antimicrobial stewardship. Nurs Stand 2018;33(6):55-58. https://doi.org/10.7748/ns.2018.e11245 [ Links ]
86. Norris A, Shrestha N, Allison G, et al. 2018 Infectious Diseases Society of America Clinical Practice Guideline for the Management of Outpatient Parenteral Antimicrobial Therapy. Clin Infect Dis 2019;68(1):e1-e35. https://doi.org/10.1093/cid/ciy745 [ Links ]
87. Manning M. Antibiotic stewardship for staff nurses. Am Nurse Today 2016;11(5):12-14. [ Links ]
88. Wiley K, Villamizar H. Resistance policy and the stewardship role of the nurse. Policy Polit Nurs Pract 2019;20(1):8-17. https://doi.org/10.1177/1527154418819251 [ Links ]
89. World Health Organization. WHO Global Strategy for Containment of Antimicrobial Resistance. Geneva: WHO, 2001. https://www.who.int/drugresistance/WHO_Global_Strategy.htm/en/ (accessed 30 September 2019). [ Links ]
90. Edwards R, Loveday H, Drumright L, et al. Should nurses be more involved in antimicrobial management? J Infect Prev 2011;12(1):4-5 https://doi.org/10.1177/1757177410392025 [ Links ]
91. Monsees E, Popejoy L, Jackson M, et al. Integrating staff nurses in antibiotic stewardship: Opportunities and barriers. Am J Infect Control 2018;46(7):737-742. https://doi.org/10.1016/j.ajic.2018.03.028 [ Links ]
92. Kirby E, Broom A, Overton K, et al. Reconsidering the nursing role in antimicrobial stewardship: A multisite qualitative interview study. BMJ Open 2020;10(10):e042321. https://doi.org/10.1136/bmjopen-2020-042321 [ Links ]
93. Courtenay M, Burnett E, Castro-Sánchez E, et al. Preparing nurses for COVID-19 response efforts through involvement in antimicrobial stewardship programmes. J Hosp Infect 2020; (epub ahead of print). https://doi.org/10.1016/j.jhin.2020.06.011 [ Links ]
94. Rawson T, Moore L, Castro-Sánchez E, et al. COVID-19 and the potential long-term impact on antimicrobial resistance. J Antimicrob Chemother 2020;75(7):1681-1684. https://doi.org/10.1093/jac/dkaa194 [ Links ]
95. Charani E, Castro-Sánchez E, Holmes A. The role ofbehavior change in antimicrobial stewardship. Infect Dis Clin North Am 2014;28(2):169-175. https://doi.org/10.1016/j.idc.2014.01.004 [ Links ]
 Correspondence:
Correspondence:
J Rout
joanrout@worldonline.co.za
Accepted 23 April 2021.
Contributions of the study. The present study was undertaken to fill the gap in the literature on clinical nurses' contribution in antimicrobial stewardship. The findings of the review largely demonstrate that multidisciplinary antimicrobial stewardship guidelines fail to view the bedside nurse as a contributor within antimicrobial stewardship strategies.














