Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
Southern African Journal of Critical Care (Online)
On-line version ISSN 2078-676X
Print version ISSN 1562-8264
South. Afr. j. crit. care (Online) vol.36 n.1 Pretoria Jan./Jul. 2020
http://dx.doi.org/10.7196/sajcc.2020.v36i1.399
ARTICLE
The accuracy of the FAST stroke assessment in identifying stroke at initial ambulance call into a South African private emergency call centre
K CrauseI; W StassenII, III
IBEMC; Department of Emergency Medical Care, University of Johannesburg, South Africa
IIBTEMC, MPhil EM, PhD; OrcID 0000-0002-1486-4446; Department of Emergency Medical Care, University of Johannesburg, South Africa
IIIBTEMC, MPhil EM, PhD; OrcID 0000-0002-1486-4446; Division of Emergency Medicine, University of Cape Town, South Africa
ABSTRACT
BACKGROUND: Stroke is a potentially life-threatening, time-dependent event, and one of the leading causes of mortality and lasting morbidity in South Africa (SA). It is of vital importance that Emergency Medical Services (EMS) call-takers accurately recognise stroke symptoms and prioritise time as well as adequate care. EMS call-takers are the first link in stroke care and improving call-taker recognition of stroke signs and symptoms can drastically improve patient outcome. The Newcastle Face Arm Speech Time (FAST) test is a mnemonic aimed at improving diagnostic accuracy of stroke
OBJECTIVE: To assess the use of the FAST test at a call-taker level to raise early suspicion of stroke and appropriately allocate resources to increase awareness of time and decrease delays on scene
METHODS: A retrospective diagnostic study to determine the accuracy of the FAST mnemonic at identifying stroke when applied at EMS call-taker level. The outcome of the FAST assessment was compared with EMS stroke diagnosis for cases of a private SA EMS over a three-month period (N=146
RESULTS: Using FAST, call-takers were able to identify stroke with a sensitivity of 87.5% and a specificity of 17.4% (positive predictive value 34%, negative predictive value 74%). This yielded an overall accuracy of 40.41%
CONCLUSION: FAST is a useful screening tool for identifying stroke at call-taker level. FAST has acceptable sensitivity when used as a screening tool; however, specificity and diagnostic effectiveness are lacking. Further studies should be considered to determine call-taker as well as general public knowledge of stroke risk factors and presentation
Keywords: stroke, emergency medical services, Emergency Medical Dispatch.
Sub-Saharan Africa (sSA) is experiencing an epidemiological transition caused by a combination of lifestyle and dietary changes, urbanisation, and demographic as well as social transitions.[1,2] The incidence and burden of non-communicable diseases and risk factors for cardiovascular disease are on the rise in most low- and middle-income countries (LMICs), including South Africa (SA).[2,3] The incidence of cardiovascular disease (CVD) in sSA is increasing significantly, and between 1990 and 2013 mortality rates associated with CVD increased by 81%.[3] In 2013 the largest proportion of deaths associated with CVD in sSA was attributed to stroke.[3]
Globally, LMICs carry a disproportionately high CVD and stroke burden.[2,4] Hypertension (a risk factor for stroke) has an extremely high incidence in SA, where it largely remains poorly managed due to low awareness and poor compliance to treatment.[5] According to the 2016 South African Demographic and Health Survey,[6] 46% and 44% of SA women and men, respectively, above 15 years of age suffer from hypertension. In addition, a large proportion of the SA population suffer other risk factors, including tobacco use, obesity, diabetes and physical inactivity.[6,7] Therefore, stroke is one of the leading causes of mortality and lasting morbidity in SA,[7] leading to an estimated 25 000 deaths per year.[8]
With an increase in stroke prevalence it is imperative to improve care of those affected. Stroke is extremely time sensitive and time to definitive management directly correlates to patient outcome.[9] Delays in treatment and transport to adequate treatment centres negatively affect patient outcome and lasting morbidity.[10] In contrast, early recognition, diagnosis and transport to adequate treatment facilities have been linked to improved patient outcome.[11]
Stroke leads to cerebral infarct, and time increases risk of infarct progression to healthy tissue.[12,13] Further insult and secondary neuronal injury (such as hypoxia) can accelerate the progression of the infarct.[14] The only definitive management strategies for ischaemic stroke are reperfusion and endovascular thrombectomy.[9, 15] However, as time progresses these strategies become less effective and pose greater risk.[9] The effectiveness of tissue plasminogen activators (tPA) and patient outcome decreases over time.'161 Research suggests that these strategies are most effective within 3 to 4.5 hours from time of onset (up to 6 hours for endovascular thrombectomy combined with early tPA administration).[9,12] A delay in recognition leads to a cascade of delays in hospital arrival, diagnostic testing and imaging, stroke evaluation and a delay to definitive management.[15,17] Therefore, it is crucial to improve early diagnosis of stroke and decrease time to definitive management at appropriate facilities.
Emergency Medical Services (EMS )providers play a key role in avoiding delays and minimising time to care. By improving and prioritising early recognition, accurate diagnosis, and time-sensitive transport to definitive care, delays can be minimised.[18] A Spanish study determined the frequency and difference in time to definitive management between EMS and non-EMS-transported stroke patients.[17] EMS-transported patients underwent reperfusion strategies 3.7 times more frequently and had shorter onset to reperfusion times. In addition to decreased time to definitive management, EMS can also avoid secondary neuronal injury, namely hypoxia, hypotension and hypoglycaemia, which accelerate infarct progression.[14]
An increase in EMS contact centre recognition of stroke could improve the frequency of appropriate EMS transport as well as minimising delays in call and dispatch times.[10] SA research shows that EMS providers can accurately recognise and diagnose stroke.[19] However, there is a paucity of research into call-taker recognition of stroke signs and symptoms. Increasing the accuracy of stroke recognition by call-takers is vital in reducing treatment times and improving patient outcome, as call-taker recognition is the critical first link in stroke care.[20]
The Newcastle Face Arm Speech Time (FAST) test is a mnemonic aimed at improving accurate diagnosis of stroke.[18] FAST was developed in 1998 and attempts to accurately diagnose stroke while decreasing time of assessment and time spent on the scene.[18] It assesses facial droop, arm drift and slurred speech as indicators of stroke, with a sensitivity of 97%,[2]· and emphasises the importance of time and rapid transport to definitive care. Using the FAST mnemonic at call-taker level to raise an early suspicion of stroke and allocating resources appropriately, can significantly increase awareness of time and decrease delays on scene.[10] Furthermore, a positive FAST assessment at call-taker level can be used to raise suspicion and notify stroke centres of an incoming patient in advance of arrival. By notifying stroke centres or hospitals in advance the receiving facility can prepare for patient arrival by preparing adequate and relevant staff, such as a neurologist, as well as equipment needed for screening and treatment.[15] In Singapore implementation of prenotification and patient prioritisation resulted in 48.2% of stroke patients having a door-to-needle time of less than 60 minutes compared with 19.4% before implementation.[16] In March 2017 FAST was implemented as standard questioning at call-taker level, at a private EMS Call Centre in SA, for patients with suspected stroke.
Objective
To determine the accuracy of a positive FAST outcome in identifying stroke at call-taker level.
Methods
A retrospective diagnostic study to determine the accuracy of the FAST mnemonic at identifying stroke at call-taker level. Ethical approval with waiver of consent was obtained from the Research Ethics Committee of the Faculty of Health Sciences at the University of Johannesburg (ref. no. REC-01-74-2018). Institutional permission was obtained from the private ambulance service to access and analyse data.
Setting
This study took place in the Emergency Contact Centre of a private SA EMS service with a national footprint. The service mainly transports patients with medical insurance and sometimes patients without medical insurance who utilise government healthcare services. The Contact Centre receives ~1 500 calls per day and dispatches an ambulance to ~125 suspected strokes per month.
Procedure
Patients with suspected stroke (as identified by the selection of 'Stroke' as dispatch call category) were included over a three-month period from 1 December 2017 to 28 February 2018.
Based on the description of the patient by the caller, a call-taker will select the category of 'Stroke' on a computer-aided dispatch system. Once selected, the caller is asked whether the patient is awake, talking or breathing. Hereafter, the computer-aided dispatch system prompts the call-taker to apply the FAST assessment, based on three standardised questions:
1. Have the patient smile. Does the face look uneven?
2. Have the patient raise both arms. Does one arm drift down?
3. Is the patient unable to speak or does the patient's speech sound abnormal?
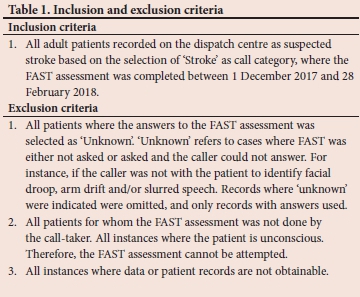
Hereafter, the inclusion and exclusion criteria were applied (Table 1), and EMS diagnosis extracted and obtained from the dispatch system's reporting interface. Data were extracted into an Excel (Microsoft Corp., USA) spreadsheet. Using the unique identifying call number, patient report forms (PRFs) were obtained to determine the EMS diagnosis of stroke. EMS diagnosis of stroke was selected as the standard for comparison as this signifies the initiation of the stroke pathway of care, and a previous study has demonstrated acceptable diagnostic accuracy of SA prehospital providers in identifying stroke.[19] The EMS diagnosis of stroke on arrival was then compared with the specific outcome (or answers) of the FAST assessment.
The outcome of the FAST assessment was compared with the EMS diagnosis, and the accuracy was calculated based on specificity, sensitivity, negative and positive predictive values, and percent (positive) agreement using standard equations.
Results
During the study period, all calls made to the private EMS call centre under the category 'Stroke' were considered for inclusion (N=520). However, based on the exclusion criteria, 72% (n=374) of the calls were excluded and the remaining 28% (n=146) of cases were included in the study for analysis (Fig. 1).

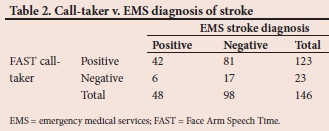
Call-taker FAST assessment was able to identify EMS stroke diagnosis with a sensitivity of 87.5% (95% CI 74.8 - 95.3) and specificity of 17.4% (95% CI 10.4 - 26.3) (Table 2). These results correspond to a positive predictive value (PPV) and negative predictive value (NPV) of 34% (95% CI 31.07 - 37.4) and 74% (95% CI 54.4 - 87.0), respectively. FAST can identify stroke with an overall accuracy of 40.4% (95% CI 32.4 - 48.8).
Discussion
When applied at the level of the call-taker, FAST recognised stroke with an accuracy of 40.4%. However, accuracy should not be considered in isolation as we identified high sensitivity and NPV indicating that FAST can accurately rule stroke out. Therefore, within this context, FAST is best suited as a screening tool to raise early suspicion of stroke.
A low PPV, and the corresponding high false positive rate, supports the use of FAST for screening, evaluation and early recognition. When used as a diagnostic tool it should be used in combination with other assessments, in person and by trained personnel.[18] This recommendation is further exemplified in our results showing a higher NPV. In the context of a call centre this is desired as a negative FAST can effectively predict a non-stroke patient. While a positive FAST does not guarantee stroke diagnosis, it does raise early suspicion and can prompt further investigation, which can result in adequate resources being dispatched such as Advanced Life Support (ALS),[22] and minimise the incidence of resources being utilised unnecessarily.
When applying FAST, we found that EMS call-takers identified stroke with a sensitivity of 87.5%. This is similar to the results of another study, focusing on EMS dispatcher recognition of stroke, identifying stroke with a sensitivity of 83%.[13] However, there are significant variation in results from other studies, with sensitivities varying between 44% and 83%.[15] One explanation for this variation in the accuracies could be the use of differing stroke screens, including FAST, the Cincinnati prehospital stroke scale (CPSS), the Los Angeles prehospital stroke screen (LAPSS) and the Melbourne ambulance stroke screen (MASS), within the contact centre.[21] FAST relies on three criteria, while CPSS, LAPSS and MASS have more detailed requirements. This can take longer to perform and might require a higher level of clinical training on the part of the call-taker. FAST offers less complexity, but this does not appear to influence accuracy in the SA setting.[21] Therefore, FAST may be preferable in SA, where call-takers are generally of lower clinical qualification and large call volumes might preclude lengthy diagnostic conversations with callers.
When performed in person by trained medical professionals, FAST has a specificity of 13%.[21] This is similar to the 17% specificity reported in this study and is not a reflection of call-taker ability but rather the disadvantages inherent to the FAST stroke assessment. FAST was designed to be a simple test that is easy to use. It is meant to aid in stroke diagnosis and recognition in combination with other assessments.[18]
Of the initial sample, 189 cases were excluded due to unknown FAST responses. In these cases, the caller was either no longer with the patient, or could not answer the questions as presented by call-takers. One reason for this could be level of education and socioeconomic status of callers.[23] Local research on socioeconomic status and stroke knowledge as well as how local populations describe stroke is not available. However, a study performed in rural Spain found a correlation between stroke knowledge and level of education and income.[23] Similar results may be expected in SA, where 8.6% of citizens above the age of 20 years received no schooling and only 12.1% obtained greater than secondary education.[24] In a multilingual and multicultural SA, further research is needed to determine how socioeconomic status, education and colloquial descriptors of stroke affect bystander and call-taker recognition of stroke. In 34 cases FAST was not asked by the call-taker. This could be because stroke symptoms were not recognised by the caller or the call-taker and, therefore, FAST was not prompted. This is likely related to public awareness of stroke symptoms.[25] Hsieh et al.[22] found that caller stroke recognition and spontaneous identification of stroke symptoms led to a much higher rate of dispatcher recognition of stroke. FAST symptoms, if recognised by the caller, were mentioned spontaneously and early during the call,[26] which can significantly aid in dispatcher recognition of stroke and reduce call time. This can be improved by implementing continuous training for EMS call centre staff and by using standardised templates for call taking and stroke assessment, such as FAST.[11] Further research is needed to determine reasons for call-takers not asking the FAST assessment.
Study limitations
This study only addressed patient data from a single private ambulance service, with callers who have private medical insurance and associated affluent socioeconomic status relative to governmental EMS users. This detracts from the external validity of our results. Larger representative studies are suggested.
As the FAST assessment is provided in English in this EMS Contact Centre, future research should profile stroke descriptors and recognition stratified to language, especially in a multilingual country like SA. In this manner, locally appropriate telephonic disease recognition models can be developed.
We compared FAST diagnosis with prehospital stroke diagnosis. It is acknowledged that this does not relate to final radiographic diagnosis. We feel that this does not detract from the validity of our study concluding the use of FAST as a screening tool, as EMS diagnosis is the factor that 'activates' the stroke system regardless of the final diagnosis. Despite this, future studies should focus on comparing call-taker and prehospital diagnosis with diagnosis at discharge.
Conclusion
FAST is a useful screening tool for identifying stroke at call-taker level. There are limitations to FAST, but these can be reduced by improving public as well as call-taker knowledge on the risk factors and presentation of stroke. FAST has acceptable sensitivity when used as a screening tool. However, specificity and diagnostic applicability are lacking. It is recommended that FAST not be used as a diagnostic tool at call-taker level but rather as a screening tool to identify stroke victims and minimise time delays to adequate treatment at appropriate facilities.
Declaration. This manuscript was submitted as partial fulfilment of the requirements for a Bachelor of Health Sciences: Emergency Medical Care, at the University of Johannesburg.
Acknowledgements. None.
Author contributions. KC designed the project, collected and analysed data, and drafted and approved the final manuscript. WS conceived the project, analysed data and approved the final manuscript.
Funding. This project was funded in full by the Emergency Care Research Unit of ER24.
Conflicts of interest. None.
References
1. Owolabi MO, Mensah GA, Kimmel PL, et al. Understanding the rise in cardiovascular diseases in Africa: Harmonising H3Africa genomic epidemiological teams and tools. Cardiovasc J Afr 2014;25(3):134-136. https://doi.org/10.5830/cvja-2014-030 [ Links ]
2. Owolabi MO, Akarolo-Anthony S, Akinyemi R, et al. The burden of stroke in Africa: A glance at the present and a glimpse into the future. Cardiovasc J Afr 2015;26(2 Suppl 1):S27-S38. https://doi.org/10.5830%2FCVJA-2015-038 [ Links ]
3. Roth G, Sampson U, et al. Mortality from cardiovascular diseases in sub-Saharan Africa, 19902013: A systematic analysis of data from the Global Burden of Disease Study 2013. Cardiovasc J Afr 2015;26(2 Suppl 1):S6-S10. https://doi.org/10.5830/cvja-2015-036 [ Links ]
4. Yusuf S, Rangarajan S, Teo K, et al. Cardiovascular risk and events in 17 low-, middle-, and high-income countries. N Engl J Med 2014;371(9):818-827. https://doi.org/10.1056/nejmoa1311890 [ Links ]
5. Gómez-Olivé FX, Ali SA, Made F, et al. Regional and sex differences in the prevalence and awareness of hypertension: An H3Africa AWI-Gen study across 6 sites in sub-Saharan Africa. Glob Heart 2017;12(2):81-90. https://doi.org/10.1016/j.gheart.2017.01.007 [ Links ]
6. National Department of Health (NDoH), Statistics South Africa, South African Medical Research Council, and ICF. South African Demographic and Health Survey 2016. Pretoria: NDoH, 2019. http://www.health.gov.za/index.php/component/phocadownload/category/539-sadhs-south-africa-demographic-and-health-survey-report?download=3325:sadhs-2016-report (accessed 12 March 2019). [ Links ]
7. Maredza M, Bertram MY, Gómez-Olivé XF, Tollman SM. Burden of stroke attributable to selected lifestyle risk factors in rural South Africa. BMC Public Health 2016;16(1):143. https://doi.org/10.1186/s12889-016-2805-7 [ Links ]
8. Maredza M, Bertram MY, Tollman SM. Disease burden of stroke in rural South Africa: An estimate of incidence, mortality and disability adjusted life years. BMC Neurol 2015;15:54. https://doi.org/10.1186/s12883-015-0311-7 [ Links ]
9. Bateman K. Medical management of acute ischaemic stroke. S Afr Med J 2019;109(2):72. http://doi.org/10.7196%2FSAMJ.2019.v109i2.00008 [ Links ]
10. Caceres JA, Adil MM, Jadhav V, et al. Diagnosis of stroke by emergency medical dispatchers and its impact on the prehospital care of patients. J Stroke Cerebrovasc Dis 2013;22(8):e610-e614.https://doi.org/10.1016/j.jstrokecerebrovasdis.2013.07.039 [ Links ]
11. Jauch EC, Saver JL, Adams HP, et al. Guidelines for the early management of patients with acute ischemic stroke. Stroke 2013;44(3):870-947. [ Links ]
12. Gomez CR. Time is brain: The stroke theory of relativity. J Stroke Cerebrovasc Dis 2018;27(8):2214-2227. https://doi.org/10.1016/j.jstrokecerebrovasdis.2018.04.001 [ Links ]
13. Ramanujam P, Castillo E, Patel E, Vilke G, Wilson MP, Dunford JV. Prehospital transport time intervals for acute stroke patients. J Emerg Med 2009;37(1):40-45. https://doi.org/10.1016/j.jemermed.2007.11.092 [ Links ]
14. Kue R, Steck A. Prehospital diagnosis and management of patients with acute stroke. Emerg Med Clin North Am 2012;30(3):617-635. https://doi.org/10.1016/j.emc.2012.05.003 [ Links ]
15. Clawson JJ, Scott G, Gardett I, et al. Predictive ability of an emergency medical dispatch stroke diagnostic tool in identifying hospital-confirmed strokes. J Stroke Cerebrovasc Dis 2016;25(8):2031-2042. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.04.021 [ Links ]
16. Tan BYQ, Ngiam NJH, Sunny S, et al. Improvement in door-to-needle time in patients with acute ischemic stroke via a simple stroke activation protocol. J Stroke Cerebrovasc Dis 2018;27(6):1539-1545. https://doi.org/10.1016/j.jstrokecerebrovasdis.2018.01.005 [ Links ]
17. Olascoaga Arrate A, Freijo Guerrero MM, Fernandez Maiztegi C, et al. Use of emergency medical transport and impact on time to care in patients with ischaemic stroke. Neurologia 2016;34(2):80-88. https://doi.org/10.1016/j.nrl.2016.11.004 [ Links ]
18. Harbison J, Hossain O, Jenkinson D, Davis J, Louw SJ, Ford GA. Diagnostic accuracy of stroke referrals from primary care, emergency room physicians, and ambulance staff using the face arm speech test. Stroke 2003;34(1):71-76. https://doi.org/10.1161/01.str.0000044170.46643.5e [ Links ]
19. Nel D, Stassen W. The accuracy of Johannesburg-based ambulance personnel in identifying stroke. S Afr J Crit Care 2015;31(2):58-61. https://doi.org/10.7196/SAJCC.2015.v31i2.247 [ Links ]
20. Chenaitia H, Lefevre O, Ho V, et al. Emergency medical service in the stroke chain of survival. Eur J Emerg Med 2013;20(1):39-44. https://doi.org/10.1097/mej.0b013e32835015ac [ Links ]
21. Brandler ES, Sharma M, Sinert RH, Levine SR. Prehospital stroke scales in urban environments: A systematic review. Neurology 2014;82(24):2241-2249. https://doi.org/10.1212%2FWNL.0000000000000523 [ Links ]
22. Hsieh MJ, Chien KL, Sun JT, et al. The effect and associated factors of dispatcher recognition of stroke: A retrospective observational study. J Formos Med Assoc 2018;117(10):902-908. https://doi.org/10.1016/j.jfma.2017.10.008 [ Links ]
23. Ramírez-Moreno JM, Alonso-González R, Peral Pacheco D, et al. Effect of socioeconomic level on knowledge of stroke in the general population: A social inequality gradient. Neurol (English Ed) 2016;31(1):24-32. https://doi.org/10.1016/j.nrl.2014.06.004 [ Links ]
24. Statistics South Africa. Census 2011: Census in brief. Report No 03-01-41. Pretoria: Stats SA, 2012. http://www.statssa.gov.za/census/census_2011/census_products/Census_2011_Census_in_brief.pdf (accessed 12 March 2019). [ Links ]
25. Sundseth A, Faiz KW, R0nning OM, Thommessen B. Factors related to knowledge of stroke symptoms and risk factors in a Norwegian stroke population. J Stroke Cerebrovasc Dis 2014;23(7):1849-1855. https://doi.org/10.1016/j.jstrokecerebrovasdis.2014.02.026 [ Links ]
26. Berglund A, von Euler M, Schenck-Gustafsson K, Castren M, Bohm K. Identification of stroke during the emergency call: A descriptive study of callers' presentation of stroke. BMJ Open 2015;5(4):e007661. https://doi.org/10.1136/bmjopen-2015-007661 [ Links ]
 Correspondence:
Correspondence:
W Stassen
Willem.stassen@uct.ac.za
Accepted 17 February 2020
Contribution of study
Stroke is one of the leading causes of death and lasting morbidity in South Africa (SA) and is increasing in incidence. Early recognition of stroke at initial emergency call may expedite treatment, thus improving outcomes. This study demonstrates that the application of the FAST assessment at emergency contact centre level in SA, might be useful at identifying stroke early. Future research should investigate barriers to its use.














