Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
Southern African Journal of Critical Care (Online)
versão On-line ISSN 2078-676X
versão impressa ISSN 1562-8264
South. Afr. j. crit. care (Online) vol.36 no.1 Pretoria Jan./Jul. 2020
http://dx.doi.org/10.7196/sajcc.2020.v36i1.398
ARTICLE
Decision-making in the ICU: An analysis of the ICU admission decision-making process using a '20 Questions' approach
P D GopalanI, II; S PershadIII, IV; B J PillayV
IMB ChB, FCA (SA), Critical Care (HPCSA), PhD; OrcID 0000-0002-3816-1171; Discipline of Anaesthesiology and Critical Care, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IIMB ChB, FCA (SA), Critical Care (HPCSA), PhD; OrcID 0000-0002-3816-1171; Intensive Care Unit, King Edward VIII Hospital, Durban, South Africa
IIIMB ChB, FCS (SA), Critical Care (HPCSA); Discipline of Anaesthesiology and Critical Care, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IVMB ChB, FCS (SA), Critical Care (HPCSA); Intensive Care Unit, Inkosi Albert Luthuli Central Hospital, Durban, South Africa
VMA (Clin Psychology), PhD; OrcID 0000-0003-1555-0753; Department of Behavioural Medicine, School of Nursing and Public Health, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND: Deciding to admit a patient into the intensive care unit (ICU) is a high-stakes, high-stress, time-sensitive process. Elucidating the complexities of these decisions can contribute to a more efficient, effective process
OBJECTIVES: To explore physicians' strategic thought processes in ICU triage decisions and identify important factors
METHODS: Practitioners (N=29) were asked to decide on ICU referrals of two hypothetic cases using a modified '20 Questions' approach. Demographic data, decisions when full information was available, feedback on questions, rating of factors previously identified as important and influence of faith and personality traits were explored
RESULTS: Of the 735 questions asked, 95.92% were patient related. There were no significant differences in interview variables between the two cases or with regard to presentation order. The overall acceptance rate was 68.96%. Refusals were associated with longer interview times (p=0.014), as were lower ICU bed capacity (p=0.036), advancing age of the practitioner (p=0.040) and a higher faith score (p=0.004). Faith score correlated positively with the number of questions asked (p=0.028). There were no significant correlations with personality trait stanines. When full information was available, acceptances for Case A decreased (p=0.003) but increased for Case B (p=0.026). The net reclassification improvement index was -0.138 (p=0.248). Non-subspecialists were more likely to change their decisions (p=0.036
CONCLUSION: Limiting information to what is considered vital by using a '20 Questions' approach and allowing the receiving practitioner to create the decision frame may assist with ICU admission decisions. Practitioners should consider the metacognitive elements of their decision-making
Keywords: decision-making, ICU admission, ICU admission decisions, ICU triage, 20 Questions.
Critical care resources are limited, especially in low- to middle-income countries.[1] Appropriate and efficient use of these resources is mandatory to ensure maximal benefit, and selecting patients who will derive the greatest benefit is crucial. Various factors interact in decision processes for admission to the intensive care unit (ICU), and identification of the most important factors will allow for a more streamlined and appropriate process.[2]
Referrals for admission to the ICU are usually via verbal or written submission of presumed relevant patient data. Based on these data and other ICU factors, such as bed availability, the ICU team may add more data by evaluating the patient themselves. There is a tendency for junior staff to amass patient data with the hope that senior staff will accurately interpret and make sense of it. Unfortunately, the presentation of such a volume of data by junior staff may confuse decision-making.
Streamlining the ICU referral processes with pro-forma data capture tools (e.g. referral forms) limits the laborious nature of referrals.[3] Refinement of such tools may improve the decision-making process. However, the exploration of patient data has identified numerous factors,[4,5] but the importance of their inclusion in the decision process remains contentious.
Various approaches have been used to understand the important factors in ICU decision-making. Many studies adopted interviews with practitioners,[6] others used detailed case scenarios directing practitioners to make decisions, and some collected patient data and extracted the factors that affect patient admission.[7] Novel approaches may better elucidate the complexities of this process.
Ashby's Law stipulates that the minimum information needed to give an accurate answer is exactly the information needed to specify the problem. The application of this law is an extrapolation from cybernetics, where the law of requisite variety applies.[8] If the question has a lot of variety, the answer will have similar variety. Enough information must be presented to reach an appropriate solution. Too little information may result in inappropriate answers; too much information, with its consequent variety, may serve to confuse and so also lead to inappropriate answers.
The framing of decisions has been described as part of the psychology of choice.[9] This 'framing effect' presents a cognitive bias, where one reacts in different ways to the same choice. A 'decision frame' is defined by an individual's formulation of the problem, as well as their norms, habits and personal characteristics, such as religious orientation. In 'positive framing', risk is avoided, whereas 'negative framing' seeks out risk. How a patient is presented by a referring doctor may alter the decision. Changing the approach to allow the receiving practitioner to frame the problem may allow for a different decision-making process. Such 'reframing' creates a new 'decision frame' - that is, from the perspective of the receiving practitioner - and is subject to a different set of characteristics and biases. In addition, any system that drives reflection on the decision-making process will enhance an awareness and understanding of one's own thought processes (metacognition).
In the game '20 Questions', a player chooses an object that others need to guess through asking a series of strategic questions;[10] only yes/no answers are allowed. The player wins if the object is not guessed correctly within 20 questions. The game encourages deductive reasoning and creativity, with key assumptions that the object exists in the minds of all players and has been correctly and similarly classified by all participants. Using a '20 Questions' approach may allow for incorporation of Ashby's Law and the framing effect into a decision-making process.
We postulate that using a modified version of the '20 Questions' approach may provide insight into the strategic thought processes that practitioners use to make high-stakes triage decisions, thereby identifying factors considered important for a referral.
Methods
All 29 critical care practitioners affiliated with the Discipline of Critical Care at the University of KwaZulu-Natal (UKZN) participated in the study. These practitioners are all actively involved in clinical critical care and responsible for ICU admission and triage decisions. The sample included intensivists, critical care fellows-in-training and other specialists, from both the private and public sectors. Participation was voluntary. Ethical approval was obtained from the Biomedical Research Ethics Committee at the UKZN (ref. no. UKZN BREC BE 337/18).
Study design
Two ICU case referrals (Case A and Case B) were created as generic representations for general ICU outcome prognostication (see supplementary file: http://sajcc.org.za/public/sup/389.pdf). Case A was designed with a poorer prognosis to suggest that acceptance into the ICU would likely be refused. Case B had a better prognosis, and so was more likely to be accepted into the ICU. To allow for adjustment and calibration of case information, the entire study procedure was piloted with two practitioners who did not take part in the study.
Study procedure
Study participants were recruited by email and completed an online questionnaire (Survey Monkey, USA). Consent and demographic data, including practitioner age, sex and race, were documented as part of the questionnaire. The full nature of the study was not shared with participants at this stage to prevent forethought about the questions to be asked.
A telephonic interview was subsequently conducted at an appointed time with each participant, during which the two cases were discussed consecutively. The order of case presentation was randomised using a random number generator. Participants were told that they were being called for an ICU referral. No further patient information was volunteered. Participants were asked to pose up to 20 questions seeking specific data to help them decide on the referral. One investigator posed as the referring doctor. Another acted as administrator, tracking the questions. Each question was fully answered. Clarifications were not regarded as separate questions. The number of questions posed was recorded, with periodic feedback to the participant. An admission decision could be made at any point in the interview, thereby terminating the game. If no decision was reached after 20 questions, additional questions could be asked until a decision was made. All interviews were recorded. The process was repeated for the second case during the same call. Participants were asked to maintain confidentiality in respect of study and case details.
A follow-up questionnaire explored additional areas. Participants were required to decide on acceptance or refusal of both cases, but with all data now available as included in the supplementary file (http://sajcc.org.za/public/sup/389.pdf). Feedback on the 20 questions and rating of the importance of previously identified factors affecting ICU admission[6] were explored via a Likert scale (1=strongly disagree; 2=disagree; 3=agree; 4=strongly agree). For statistical analysis, we grouped all affirmative answers together ('strongly agree' and 'agree') and all negative answers together ('strongly disagree' and 'disagree'). To explore the strength of religious orientation, we used the Abbreviated Santa Clara Strength of Religious Faith Questionnaire,[11] which poses five faith-related questions, scored 1 - 4. Total scores could therefore range between 5 (low strength) and 20 (high strength). It is a reliable, easy-to-use and valid self-report measure developed as an all-purpose tool for use in diverse settings with diverse populations.[12]
Each participant completed an online personality evaluation using the Basic Traits Inventory (BTI) (JvR Psychometrics, South Africa (SA)).[13] The BTI, developed to assess personality in the SA context, consists of 193 items grouped under five categories: extraversion, neuroticism, conscientiousness, openness to experience, and agreeableness. A sixth category, social desirability (13 items), is included throughout the test. Items are rated on a five-point Likert scale (1=strongly disagree; 5=strongly agree). The validity of the BTI has been shown across various cultures.[14] Results are reported in stanines across six domains.
Data analysis
Two investigators independently coded the interview responses, with an independent moderator being available to assist when consensus on an issue could not be reached. Interview variables recorded included: case allocation (A or B), number of questions, nature of each question, number of queries, nature of each query, case outcome (decision to accept or refuse), and time taken for interview (from start of questioning until decision). A question, defined as an enquiry on a specific factor or aspect of a factor, counted towards one of the 20 allowed questions. A query was defined as any enquiry expressing doubt or requesting further information to establish the validity or accuracy of a question or factor. This may have been an elaboration to add more detail concerning what had already been said, or a clarification to make a statement more understandable.
Statistical analysis was performed using the software SPSS (version 25) (IBM Corp., USA). Pearson's and Spearman's correlations, f-tests, χ2 tests and point-biserial tests were used as appropriate. Interview variables (outcome, queries, questions and time) were used to compare cases with regard to prognosis, order and decision. Admitted and refused cases were compared. Associations between practitioner characteristics and interview variables were explored. Comparisons were made between outcomes of the '20 Questions' interview and those of the post-interview questionnaire using the net reclassification improvement (NRI) index[15](MathWorks Inc., USA).[16] A significance level of p<0.05 was used.
Results
The demographic profile of the study participants is described in Table 1. All 29 practitioners who were approached completed the study.
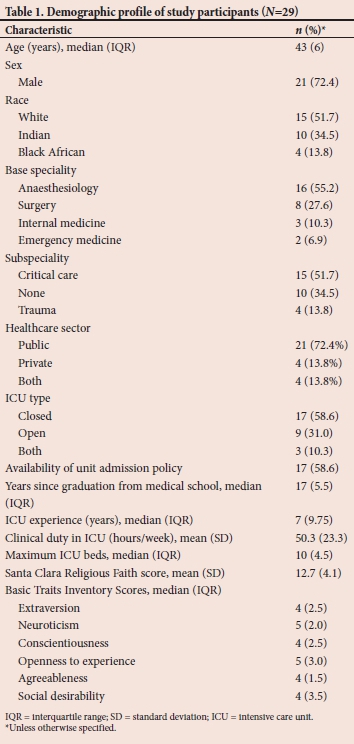
Table 2 presents a comparison of the outcomes and interview variables according to case label and order of presentation after the '20 Questions' telephonic interview. The overall acceptance across the two cases was 68.96% («=40/58). Case A was accepted by 55.17% (n=16) of the participants and Case B by 82.76% (n=24) of the participants.
Further analysis of decisions during the follow-up interview, in which full case information was available, revealed that acceptance of Case A decreased to 27.59% (n=8) and acceptance of Case B increased to 96.55% (n=28). These changes were significant for both Case A (p=0.003) and Case B (p=0.026) individually, but not for a comparison of outcome changes between the two cases (p=0.289). All decision changes were in favour of our predictions. Compared with when full case information was available, the NRI index for the '20 Questions' approach was -0.138 (p=0.248).
Comparing the profiles of participants who changed their decision (n=10) with those of participants who did not (n=19) showed that non-subspecialists were more likely to change their decisions (p=0.036). Two participants changed their decisions for both cases. There was also a trend for female participants to change their decisions (p=0.05). There were no associations with other variables.
Table 3 reflects associations between variables of the '20 Questions' interview and participant profiles. The mean time for refusals was significantly greater than for acceptances (372 s v. 276 s, p=0.038). There was a significant difference between outcomes based on the '20 Questions' interview and when full case information was available (p=0.000). A higher faith score correlated with a greater number of questions (p=0.028). Longer interview times correlated with advancing age (p=0.040), a smaller maximum number of ICU beds (p=0.036) and a higher faith score (p=0.004). There were no significant correlations with the six BTI stanines.
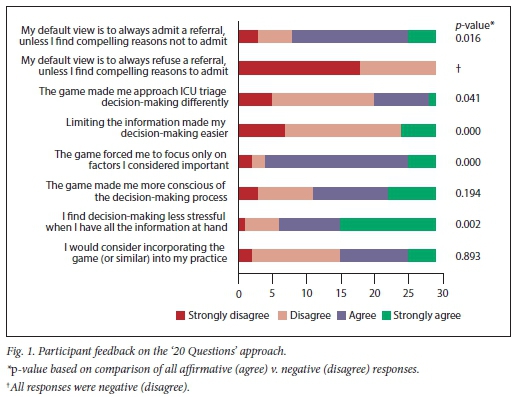
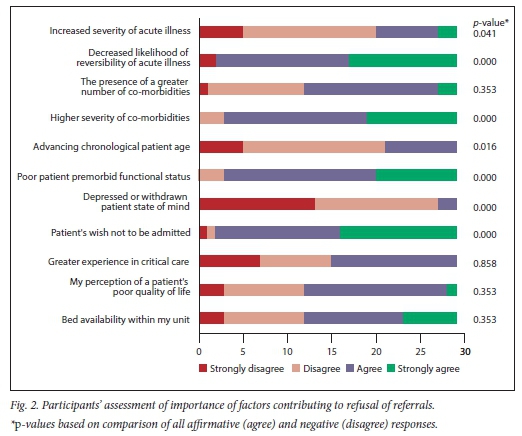
Responses to the post-interview questionnaire, in which participants were asked to rate issues related to the '20 Questions' approach to decision-making are reflected in Fig. 1. All participants indicated their default view would never be to refuse a patient referral. Responses rating the importance of selected previously identified factors are shown in Fig. 2.
The actual questions were subsequently categorised as patient-related, physician-related or environment-related (Table 4). A total of 735 questions were posed by 29 participants across 58 patient cases, resulting in a median (and associated interquartile range (IQR)) of 13.5 (5). The majority of questions (95.92%) related to the patient. Sublevel coding was applied to patient-related factors, as shown in Table 4.
Discussion
The ICU admission decision is a high-stakes, high-stress and time-sensitive process. Traditional methods of research and analysis have relied on observation of actual case referrals,[17] simulated situations,[18] or surveys.[19] We describe the novel use of a '20 Questions'-type approach to better explore the complexities of this process. Our rationale centred around (i) the game's ability to promote deductive reasoning while limiting information to only what was considered vital,[8] and ( ii) the propensity to allow reframing of the clinical case from the perspective of the receiver (critical care practitioner) rather than the sender (referring doctor).[9]
The conventional '20 Questions' game created a pressured situation for a high-stakes decision given the limitation of information that was imposed. The game therefore needed to be modified to make it relevant to our setting. We chose telephonic interviews over face-to-face interviews to minimise the effect of non-verbal factors and opted to give complete answers, including clarifications. We believe this better explored the process and allowed relevant factors to emerge, rather than being merely a test of the participant's skill in playing the game. We also allowed the game to extend beyond 20 questions.
Feedback on decision outcomes affects future decision processes. In a non-medical setting, people become 'regret averse' in subsequent decisions.[20] Any type of comparative judgement leads to a comparative judgement mindset, which is transferred to, and influences, a subsequent decision-making process.[21] The influence of a preceding decision on a subsequent one has not been explored in the critical care domain. As our two cases were interrogated in the same telephonic conversation, we were concerned that a learning effect could influence the process and outcome of the second case; first-case presentation was therefore randomised. Our analysis of case label versus case order revealed no differences (Table 2), suggesting no influence of the '20 Questions' approach.
Case A and Case B were set up with different prognoses to allow for different decisions. Correspondence between participants' outcomes and our expectations varied. The higher-than-expected proportion of participants who accepted Case A in the '20 Questions' interview (55.2%) may suggest an inappropriate set-up of the case, incomplete interrogation, or a bias to default to acceptance when incomplete information is available. When full case information was available, outcomes better matched our predictions (refusal of Case A = 72.41%; acceptance of Case B = 96.55%). Although the decision change was significant within a case, there was no difference when the decision changes were compared across the two cases. This result suggests that the case set-up (including the expected prognosis) did not affect changes in decisions.
Other investigators have also demonstrated varied correspondence between practitioners' admission decisions and the expected decisions. Dahine et al.[22]found 53 - 61% correspondence using five cases. In another study, 30% of physicians admitted a simulated patient with poor prognosis to the ICU.[23] Among physicians who estimated survival probability as <1%, 17.2% would still have admitted the patient.[24]
We chose an NRI index to distinguish between the outcomes derived after the '20 Questions' interview and when full case information was available. The overall index of -0.138 indicates a net reclassification in favour of the non-event (refusal), but the change was not significant. The direction of reclassification may imply that in the face of uncertainty, more information is needed for a refusal decision. However, the right balance between too little and too much information must be sought. The restriction of information in the '20 Questions' interview was largely self-imposed. The median (IQR) number of questions was 13.5 (5), suggesting that the interview could have continued beyond the actual observed termination point. None of the participants invoked the allowance to proceed beyond 20 questions. Participants who changed their decisions thus failed to elicit all information they considered important.
Non-subspecialists were more likely to change their decision during the follow-up interview. Their willingness to change may be explained by their greater degree of uncertainty, with a resultant lack of confidence in their decisions. Although the decision-making process has been noted to be different for experts and non-experts in various contexts,[25-27] decision changes in our study were associated only with subspecialist status and not years of experience. The registration status of subspecialist qualifications and its accompanying effect on decisionmaking is a likely explanation. Female participants showed a trend towards decision changes (p=0.050). The influence of gender on ICU decision-making has previously been identified. Sagy et al.[28] reported that a female patient treated by a female physician was associated with the lowest likelihood of ICU admission compared with other combinations.
We expected to observe differences in interview variables between Case A and Case B. Given the poorer prognosis, a greater degree of interrogation was expected for Case A to attain higher certainty before refusing admission. No significant differences were noted.
Non-medical literature shows that decision processes leading to agreement differ from those that do not lead to agreement.[29] We postulated that there would be more queries and questions, and a longer decision time, for refusals than for acceptances. This assumption was on the basis of the perceived need for greater certainty before refusing a patient. A longer decision time was indeed noted for refusals, but no significant differences were observed with regard to queries or questions. This was unexpected and may indicate that the queries and questions were much longer, or that the interaction was more deliberate with longer periods of reflection.
The role of personal and cultural characteristics of intensivists in ICU admission decision-making has not been clearly elucidated in the existing literature. We explored relationships between practitioner characteristics and interview variables as part of strategic decision-making. Physicians' religious beliefs have previously been identified as a factor affecting the ICU admission decision.[30,31] In our study, participants with a higher faith score posed more questions and their interviews lasted longer, suggesting their need for greater certainty. Older participants also engaged in longer interviews. We expected older, more experienced practitioners to be more focused with their questioning, therefore requiring fewer questions and less time. The unexpected finding may be a reflection of such practitioners seeking higher certainty or it may be a result of their more considered strategic decision-making process. Practitioners whose ICUs had a lower maximum bed capacity also took longer to reach a decision. A possible explanation is that greater certainty is needed when capacity is limited. No significant associations were found between interview variables and race or gender. We could not find any existing literature that relates a practitioner's race profile to ICU decisions in general or admission decisions in particular.
With regard to the effect and utility of a '20 Questions' approach (Fig. 1), the majority of the participants agreed that their default position was to admit a referred patient, consistent with the prevailing view by medical practitioners that all lives should be saved. None of the participants indicated that their default position was to refuse, which may be attributed to some participants believing that they did not have a specific default position and therefore assessed each case independently. This does not account for bias that may often be implicit.[32] The majority of the participants indicated that limiting information did not make decision-making easier; instead, decision-making was deemed less stressful when all information was available. The routine practice of having a standard battery of questions appears to support the observation that a perceived comfort is derived from having all the information available. The majority of participants agreed that the '20 Questions' interview forced them to focus on factors they considered important. The implication is that the emergent factors and themes would all be important and appropriate. However, factors of varying importance emerged. In addition, only a small proportion of practitioners were willing to consider incorporating such a system into their clinical practice. These anomalies reflect a 'thought-deed discordance',[6] which is supported by the majority of the participants indicating that decision-making was less stressful when full information was at hand. The feedback responses emphasise the need for practitioners to focus on the metacognitive elements of decision-making, thereby enhancing their awareness and understanding of their strategic decision processes.
The effect of personality traits on ICU triage has not been clearly elucidated. Personality traits may predispose one to a specific approach to reasoning and so may be a predictor of decision-making behaviour for gathering information, to revise beliefs or to address uncertainty.[33] Aspects of personality and religious beliefs influence the attitudes of ICU personnel when making decisions to forego life-sustaining treatments.[34] We were not able to demonstrate any relationship between personality and patient or interview variables. The role of physician personality in ICU triage decisions needs further exploration.
Emerging questions and themes were consistent with previously identified factors.[6] It was unclear whether questions were asked out of habit or for their true value in deciding. For example, participants enquired about a patient's age in 75.86% of cases, whereas questions about a patient's wishes were included only in 10.34% of cases.
Study limitations
Assumptions made during the '20 Questions' interview may have affected physicians' understanding of answers. This was minimised by modifying the yes/no response of the conventional game to full answers. The study explored only some of the factors involved in the decision-making process, and many others affect the final decision, including ICU factors (e.g. bed status), practitioner-related factors (e.g. bias) and factors external to the ICU environment (e.g. transport). These may not necessarily have emerged, as practitioners may have made assumptions about these despite a context being described. The study focused only on a localised sample of practitioners primarily involved in critical care. The identified factors from this cohort may therefore not be generalisable.
Conclusion
Using a modified '20 Questions' approach, we explored the strategic thought processes used by practitioners to make complex, high-stakes triage decisions. Reframing referrals from the perspective of the receiving practitioner was useful. The approach encouraged deductive reasoning while limiting information. Factors of varying importance emerged. The results emphasise the need for practitioners to focus on the metacognitive elements of decision-making, and novel approaches may be necessary to better elucidate the complexities of decisions regarding ICU admission to allow for a more efficient and effective process.
Declaration. None.
Acknowledgements. None.
Author contributions. All authors contributed equally to the study and manuscript development.
Funding. None.
Conflicts of interest. None.
References
1. Scribante J, Bhagwanjee S. National audit of critical care resources in South Africa: Unit and bed distribution. S Afr Med J 2007;97(12):1311-1314. [ Links ]
2. Gordon K, Allorto N, Wise R. Analysis of referrals and triage patterns in a South African metropolitan adult intensive care service. S Afr Med J 2015;105(6):491-495. https://doi.org/10.7196/samj.9007 [ Links ]
3. Ramos JGR, Perondi B, Dias RD, et al Development of an algorithm to aid triage decisions for intensive care unit admission: A clinical vignette and retrospective cohort study. Crit Care 2016;20:81. https://doi.org/10.1186/s13054-016-1262-0 [ Links ]
4. Nates JL, Nunnally M, Kleinpell R, et al. ICU admission, discharge, and triage guidelines: A framework to enhance clinical operations, development of institutional policies, and further research. Crit Care Med 2016;44(8):1553-1602. https://doi.org/10.1097/CCM.0000000000001856 [ Links ]
5. Orsini J, Butalaa A, Ahmada N, Llosa A, Prajapati R, Fishkin E. Factors influencing triage decisions in patients referred for ICU admission. J Clin Med Res 2013;5(5):343-349. https://doi.org/10.4021/jocmr1501w [ Links ]
6. Gopalan PD, Pershad S. Decision-making in ICU - a systematic review of factors considered important by ICU clinician decision makers with regard to ICU triage decisions. J Crit Care 2019;50:99-110. https://doi.org/10.1016/j.jcrc.2018.11.027 [ Links ]
7. Gopalan PD, De Vasconcellos K. Factors influencing the decisions to admit or refuse patients into a South African tertiary intensive care unit. S Afr Med J 2019;109(9):645-651. https://doi.org/10.7196/samj.2019.v109i9.13678 [ Links ]
8. Ashby WR. An Introduction to Cybernetics. London: Chapman & Hall, 1956. [ Links ]
9. Tversky A, Kahneman D. The framing of decisions and psychology of choice. Science 1981;211(4481):453-458. [ Links ]
10. Walsworth MT. Twenty Questions: A short treatise on the game to which are added a code of rules and specimen games for the use of beginners. New York: Holt, 1882. [ Links ]
11. Plante TG, Vallaeys CL, Sherman AC, Wallston KA. The development of a brief version of the Santa Clara Strength of Religious Faith Questionnaire. Pastoral Psychol 2002;50(5):359-368. https://doi.org/10.1023/a:1014413720710 [ Links ]
12. Plante TG. The Santa Clara Strength of Religious Faith Questionnaire: Assessing faith engagement in a brief and nondenominational manner. Religions 2010;1:3-8. https://doi.org/10.3390/rel1010003 [ Links ]
13. Taylor N, De Bruin GP. Manual of the Basic Traits Inventory. Johannesburg: JvR Psychometrics, 2006. [ Links ]
14. Meiring D, Van de Vijver AJR, Rothmann S, Barrick MR. Construct, item, and method bias of cognitive and personality tests in South Africa. S Afr J Ind Psychol 2005;31(1):1-8. https://doi.org/10.4102/sajip.v31i1.182 [ Links ]
15. Pencina MJ, DAgostino Sr RB, D'Agostino Jr RB, Vasan RS. Evaluating the added predictive ability of a new marker: From area under the ROC curve to reclassification and beyond. Statist Med 2008;27:157-172. https://doi.org/10.1002/sim.2929 [ Links ]
16. MathWorks. Matlab. https://www.mathworks.com/products/matlab.html (accessed 15 February 2019). [ Links ]
17. Charlesworth M, Mort M, Smith AF. An observational study of critical care physicians' assessment and decision-making practices in response to patient referrals. Anaesthesia 2017;72:80-92. https://doi.org/10.1111/anae.13667 [ Links ]
18. Barnato AE, Mohan D, Downs J, Bryce CL, Angus DC, Arnold RM. A randomized trial of the effect of patient race on physician ICU and life-sustaining treatment decisions for an acutely unstable elder with end-stage cancer. Crit Care Med 2011;39(7):1663-1669. https://doi.org/10.1097/CCM.0b013e3182186e98 [ Links ]
19. Ramos JGR, Passos RdH, Baptista PBP, Forte DN. Factors potentially associated with the decision of admission to the intensive care unit in a middle-income country: A survey of Brazilian physicians. Rev Bras Ter Intensiva 2017;29(2):154-162. https://doi.org/10.5935/0103-507x.20170025 [ Links ]
20. Raeva D, Van Dijk E, Zeelenberg M. How comparing decision outcomes affects subsequent decisions: The carry-over of a comparative mind-set. Judgm Decis Mak 2011;6(4):343-350. [ Links ]
21. Xu AJ, Wyer Jr RS. The comparative mind-set: From animal comparisons to increased purchase intentions. Psychol Sci 2008;19(9):859-864. https://doi.org/10.1111/j.1467-9280.2008.02169.x [ Links ]
22. Dahine J, Mardini L, Jayaraman D. The perceived likelihood of outcome of critical care patients and its impact on triage decisions: A case-based survey of intensivists and internists in a Canadian, quaternary care hospital network. PLoS ONE 2016;11(2):e0149196 https://doi.org/10.1371/journal.pone.0149196 [ Links ]
23. Barnato AE, Hsu HE, Bryce CL, et al. Using simulation to isolate physician variation in ICU admission decision making for critically ill elders with end-stage cancer: A pilot feasibility study. Crit Care Med 2008;36(12):3156-3163. https://doi.org/10.1097/CCM.0b013e31818f40d2 [ Links ]
24. McNarry AF, Goldhill DR. Intensive care admission decisions for a patient with limited survival prospects: A questionnaire and database analysis. Intensive Care Med 2004;30:325-330. https://doi.org/10.1007/s00134-003-2072-9 [ Links ]
25. Dew N, Read S, Sarasvathy SD, Wiltbank R. Effectual versus predictive logics in entrepreneurial decision-making: Differences between experts and novices. J Bus Venturing 2009;24:287-309. https://doi.org/10.1016/j.jbusvent.2008.02.002 [ Links ]
26. Cuthbert L, Duboulay B, Teather D, Teather B, Sharples M, Duboulay G. Expert/novice differences in diagnostic medical cognition - a review of the literature. University of Sussex. Cognitive Science Research Paper. CSRP 1999:508. [ Links ]
27. McCormack C, Wiggins MW, Loveday T, Festa M. Expert and competent non-expert visual cues during simulated diagnosis in intensive care. Front Psychol 2014;5:949. https://doi.org/10.3389/fpsyg.2014.00949 [ Links ]
28. Sagy I, Fuchs L, Mizrakli Y, et al. The association between the patient and the physician genders and the likelihood of intensive care unit admission in hospital with restricted ICU bed capacity. QJM 2018;111(5):287-294. https://doi.org/10.1093/qjmed/hcy017 [ Links ]
29. Tuncel E, Mislin A, Kesebir S, Pinkley RL. Agreement attraction and impasse aversion: Reasons for selecting a poor deal over no deal at all. Psychol Sci 2016;27(3):312-321. https://doi.org/10.1177/0956797615619200 [ Links ]
30. Einav S, Soudry E, Levin PD, Grunfeld GB, Sprung CL. Intensive care physicians' attitudes concerning distribution of intensive care resources: A comparison of Israeli, North American and European cohorts. Intensive Care Med 2004;30:1140-1143. https://doi.org/10.1007/s00134-004-2273-x [ Links ]
31. Giannini A, Consonni D. Physicians' perceptions and attitudes regarding inappropriate admissions and resource allocation in the intensive care setting. Br J Anaesth 2006;96(1):57-62. https://doi.org/10.1093/bja/aei276 [ Links ]
32. Saposnik G, Redelmeier D, Ruff CC, Tobler PN. Cognitive biases associated with medical decisions: A systematic review. BMC Med Inform Decis Mak 2016;16(1):138. https://doi.org/10.1186/s12911-016-0377-1 [ Links ]
33. Bensi L, Giusberti F, Nori R, Gambetti E. Individual differences and reasoning: A study on personality traits. Br J Psychol 2010;101:545-562. [ Links ]
34. Ntantana A, Matamis D, Savvidou S, et al. The impact of healthcare professionals' personality and religious beliefs on the decisions to forego life sustaining treatments: An observational, multicentre, cross-sectional study in Greek intensive care units. BMJ Open 2017;7:e013916. https://doi.org/10.1136/bmjopen-2016-013916 [ Links ]
 Correspondence:
Correspondence:
P D Gopalan
gopalan@ukzn.ac.za
Accepted 12 November 2019
Contribution of study
The study used a novel approach to explore physicians' decision-making process for admitting a patient to the intensive care unit (ICU). Understanding the main factors that influence the decision-making process will allow for streamlining the referral process, more effective selection of patients most likely to benefit from ICU treatment, and prevent inappropriate admissions into the ICU. The findings can also help to improve data capture tools and encourage practitioners to critically reflect on their decision-making processes.














