Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
Southern African Journal of Critical Care (Online)
On-line version ISSN 2078-676X
Print version ISSN 1562-8264
South. Afr. j. crit. care (Online) vol.36 n.1 Pretoria Jan./Jul. 2020
http://dx.doi.org/10.7196/sajcc.2020.v36i1.447
REVIEWS
INVITED REVIEW
The role of laboratory testing in hospitalised and critically ill COVID-19-positive patients
S OmarI; D BakerII; R SiebertIII; I JoubertIV; B LevyV; F ParukVI; P D GopalanVII
IMB ChB, FC Path (Chem) SA, DA (SA), Cert Crit Care (SA); OrcID 0000-0001-8494-1518; Intensive Care Unit, Division of Critical Care, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand and Chris Hani Baragwanath Academic Hospital, Johannesburg, South Africa
IIMB ChB, FRCP (London); Department of Adult Critical Care, Livingstone Tertiary Hospital and Faculty of Health Sciences, Walter Sisulu University, Port Elizabeth, South Africa
IIIMB ChB, FCP (SA), Cert Crit Care (SA) (Phys); Life Groenkloof Hospital, Tshwane, South Africa
IVMB ChB, FCA (SA), Critical Care (HPCSA); OrcID 0000-0003-2864-0045; Division of Critical Care, Department of Anaesthesia and Perioperative Medicine, Groote Schuur Hospital and University of Cape Town, South Africa
VMB ChB, FCA (SA), Cert Crit Care (SA); Intensive Care, Netcare Rosebank Hospital, Johannesburg South Africa
VIMB ChB, FCOG (SA), Cert Crit Care (SA), PhD (Clinical Medicine); Critical Care Department, Steve Biko Academic Hospital and University of Pretoria, South Africa
VIIMB ChB, FCA (SA), Critical Care (HPCSA), PhD; OrcID 0000-0002-3816-1171; Discipline of Anaesthesiology and Critical Care, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
The COVID-19 pandemic has placed healthcare resources around the world under immense pressure. South Africa, given the condition of its healthcare system, is particularly vulnerable. There has been much discussion around rational healthcare utilisation, ranging from diagnostic testing and personal protective equipment to triage and appropriate use of ventilation strategies. There has, however, been little guidance around use of laboratory tests once COVID-19 positive patients have been admitted to hospital. We present a working guide to rational laboratory test use, specifically for COVID-19, among hospitalised patients, including the critically ill. The specific tests, the reasons for testing, their clinical usefulness, timing and frequency are addressed. We also provide a discussion around evidence for the use of these tests from a clinical perspective.
Keywords: COVID-19, coronavirus disease, SARS-CoV-2, laboratory tests, diagnostics.
Within a tew months of the World Health Organization declaring a global pandemic, there have been several million recorded cases of coronavirus disease 2019 (COVID-19) worldwide.[3] The broad clinical spectrum -from mild to lite-threatening disease - highlights the importance of determining which groups develop severe diseased[4,5] The use of SOFA (sequential organ failure assessment) scores and additional laboratory data appears to have value in the assessment, prognostication and management of COVID-19 patients.[4] Laboratory tests used for COVID-19-positive patients have been briefly addressed in the literature.!61 We aim to further describe the clinical utility of these tests which will assist the clinician in their effective use. The role of diagnostic tests for severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is beyond the scope of this paper.
Clinical staging
A clinically useful staging system has been proposed, and is shown in Table 1.[7] The model proposes an initial clinical stage attributed to the virus itself, which is subsequently followed by characteristically different stages evolving in relation to the host response. Laboratory features play an important part of the entire clinical picture and help to identify the disease stage.P] This staging creates the platform to adjudge severity, disease progression, the level of care required, and also provides insights regarding the timing of stage-specific unique therapies such as targeting the virus in the initial stages and focusing on the role of exaggerated host immune response in the latter stages.
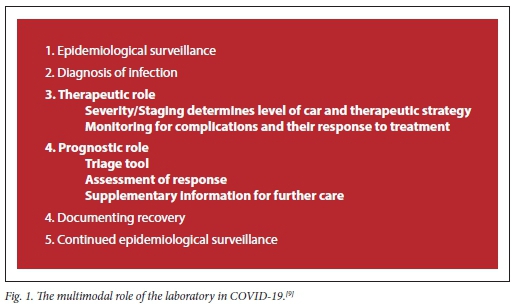
Laboratory role
The role of the laboratory in COVID-19 extends from epidemiological surveillance to patient management (Fig. 1). We deal specifically with the role of laboratory tests during the assessment and management of overt disease among COVID-19-positive patients who have disease severe enough to require hospitalisation, including critically ill patients.
The National Institute for Communicable Diseases guidelines suggest keeping broad local and clinically relevant differential diagnoses for patients presenting with severe illness (all hospitalised patients).[10] Blood cultures and assessment for other causes of community-acquired pneumonia, e.g. mycobacterial infection, Pneumocystis jirovecii pneumonia, influenza and other relevant atypical infections are suggested.
Discussion
Several laboratory tests may provide information for staging/severity and possible therapeutic interventions, prognostic information and monitoring. Timely identification of at-risk patients may enable prompt escalation of care. De-escalation may also enhance appropriate resource utilisation.
The white blood cell count, inclusive of neutrophil and lymphocyte counts, lactate dehydrogenase, alanine aminotransferase, aspartate aminotransferase, total bilirubin, troponin, D-dimer and procalcitonin (PCT) levels are associated with increased odds of ICU admission^11] In a separate study that included 140 COVID-19 patients, increased C-reactive protein (CRP), D-dimer and PCT levels were associated with greater severity of disease.[12] Other laboratory abnormalities demonstrated to be associated with poor outcomes include albumin, serum creatinine (sCr) and prothrombin time (PT/INR).[11]
Coagulation appears to have a role in COVID-19, with >70% of non-survivors shown to demonstrate overt disseminated intravascular coagulation (DIC).[13] These patients had significantly elevated Z>dimers, PT and fibrin degradation products when compared with survivors. A D-dimer value above 1 mg/L at admission was associated with increased mortality.[4] Activated partial thromboplastin time, although higher, did not reach statistical significance. Elevated D-dimers may be used as an indication for admission, and monitored daily until improvement begins. The relevance of additional daily testing of PT, fibrinogen and platelet counts in the case of an elevated D-dimer value is to monitor for worsening of the coagulopathy.[14] In the analysis of 449 patients with severe COVID- 19, those with a sepsis-induced coagulopathy score >4 and who were treated with heparin had a 24% lower mortality than those who were not treated.[15] The investigators also found a 20% reduction in mortality when heparin was used in patients with a D-dimer above 3 mg/L. Coagulation studies may therefore be useful for determining severity, progression (adaptive haemostasis to DIC and multiorgan failure), prognosis and guiding therapy.[16] Thromboelastography provides a point-of-care result, and this evaluation of coagulation factors, fibrinogen, platelet function and fibrinolysis has been recommended in some guidelines.[17]
Procalcitonin has not been found to be elevated initially among COVID-19 patients. An increase likely mirrors bacterial superinfection, and may be associated with a worse outcome.[11,18] A progressive increase may also occur with a dysregulated inflammatory response.[19]
Urine analysis performed on day 1 after admission also revealed a relationship between both urine protein and urine glucose and severity of disease. Patients with hypertension, diabetes and/or urinary tract infections were excluded from this study.[20]
Electrolyte abnormalities are significant among patients with severe COVID-19. Sodium (Na+), potassium (K+) and calcium (Ca2+) were found to be low in these patients.[21] Hypokalaemia, reported to be low in as many as 60% of cases,[22] is likely the most relevant, as it has both clinical and pathophysiological significance. Clinically,
hypokalaemia is associated with a worsening of cardiac complications and acute respiratory distress syndrome. The SARS-CoV-2 virus attaches to the angiotensin-converting enzyme receptor 2 (ACE-2). This enables viral entry into the alveolar cell, but also down-regulates the ACE-2 receptor, causing an increase in angiotensin II. This may explain K+ loss and hypokalaemia at a renal level. Gastrointestinal symptoms, including diarrhoea, have been described in ~one-third of COVID-19 patients.[23] Monitoring will therefore enable appropriate fluid and electrolyte management. Monitoring of urea, creatinine and electrolytes is important for the assessment of severity/prognostication and therapeutic management.
Cardiac biomarkers including troponins and B-type natriuretic peptide (pro-BNP) may also be of value. Myocarditis with impaired systolic function has been reported in patients with COVID-19. Both troponins and pro-BNP values are elevated.[24] Abnormal troponin results were detected in 22.6% of 5 700 hospitalised patients.[25]
Identification of the cytokine storm, a clinical picture that has much in common with macrophage activation syndrome/haemophagocytic lymphohistiocytosis has been observed, but is largely lung-centric. Identification thereof may be key to timely therapeutic interven-tions.[26,27] This complication may be recognised by increases in CRP, ferritin, D-dimers and liver transaminases, as well as a shift from a predominant pulmonary disease state to one with multisystem complications/involvement. Interleukin-6 (IL-6) has been shown to correlate with qualitative serum viral loads (SARS-CoV-2 viraemia).[28] High CRP levels were significantly associated with the development of severe disease. The receiver operator curve reflected good accuracy for predicting severe disease (area under curve = 0.84).[29]
Arterial blood gas analysis is particularly useful for determination of the PaO2//FiO2 ratios, calculation of the alveolar arterial gradient (A-aDO2) and the oxygenation index.[4,23] Blood gas information is valuable throughout hospitalisation, from the initial triage to the point of removal of supplementary oxygenation support.
The suggestions made above are time-limited. As our understanding of this disease rapidly unfolds, additional tests may be introduced or the use of currently recommended tests may be amended. Local experts should be consulted when available and modifications to these suggestions should be anticipated.
Declaration. None.
Acknowledgements. None.
Author contributions. All authors contributed to the design and approach of the article, literature review and analysis, article drafting, final approval and submission.
Funding. No funding required for the write up of this article. Funding for article processing charges will be sought from the Critical Care Society of Southern Africa.
Conflicts of interest. None.
References
1. Johns Hopkins Coronavirus Resource Center. COVID-19 map. https://coronavirus.jhu.edu/map.html (accessed 8 May 2020). [ Links ]
2. Kakodkar P, Kaka N, Baig M. A comprehensive literature review on the clinical presentation, and management of the pandemic coronavirus disease 2019 (COVID-19). Cureus 12(4): e7560. https://doi.org/10.7759%2Fcureus.7560 [ Links ]
3. Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Bio-Medica Atenei Parm 2020;91(1):157-160. https://doi.org/10.23750/abm.v91i1.9397 [ Links ]
4. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020;395(10229):1054-1062. https://doi.org/10.1016/s0140-6736(20)30566-3 [ Links ]
5. Zheng F, Tang W, Li H, Huang Y-X, Xie Y-L, Zhou Z-G. Clinical characteristics of 161 cases of corona virus disease 2019 (COVID-19) in Changsha. Eur Rev Med Pharmacol Sci 2020;24(6):3404-3410. https://doi.org/10.26355/eurrev_202003_20711 [ Links ]
6. Favaloro EJ, Lippi G. Recommendations for minimal laboratory testing panels in patients with COVID-19: Potential for prognostic monitoring. Semin Thromb Hemost 2020;46(3):379-382. https://doi.org/10.1055/s-0040-1709498 [ Links ]
7. Siddiqi HK, Mehra MR. COVID-19 illness in native and immunosuppressed states: A clinical-therapeutic staging proposal. J Heart Lung Transplant 2020;39(5):405-407. https://doi.org/10.1016%2Fj.healun.2020.03.012 [ Links ]
8. Gandhi RT, Lynch JB, del Rio C. Mild or moderate COVID-19. N Engl J Med 2020;(4):24 https://doi.org/10.1056/NEJMcp2009249 [ Links ]
9. Lippi G, Plebani M. The critical role of laboratory medicine during coronavirus disease 2019 (COVID-19) and other viral outbreaks. Clin Chem Lab Med 2020 25;58(7):1063-1069. [ Links ]
10. The National Institute for Communicable Diseases of South Africa. Guidelines for case finding, diagnosis, management and public health response in South Africa. https://www.nicd.ac.za/ (accessed 1 May 2020). [ Links ]
11. Lippi G, Plebani M. Laboratory abnormalities in patients with COVID-2019 infection. Clin Chem Lab Med 2020;58(7):1131-1134. [ Links ]
12. Zhang J-J, Dong X, Cao Y-Y, et al Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy 2020;00:1-12. https://doi.org/10.1111/all.14238 [ Links ]
13. Tang N, Li D, Wang X, Sun Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 2020;8(4):844-847. https://doi.org/10.1111/jth.14768 [ Links ]
14. Thachil J, Tang N, Gando S, et al. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost 2020;18(5):1023-1026. https://doi.org/10.1111/jth.14810 [ Links ]
15. Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost 2020;18(5):1094-1099. https://doi.org/10.1111/jth.14817 [ Links ]
16. Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood 2020;(4):27. https://doi.org/10.1182/blood.2020006000 [ Links ]
17. Song JC, Wang G, Zhang W, et al. Chinese expert consensus on diagnosis and treatment of coagulation dysfunction in COVID-19. Mil Med Res 2020;7(1):19. https://doi.org/10.1186/s40779-020-00247-7 [ Links ]
18. Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, et al. Clinical, laboratory and imaging features of COVID-19: A systematic review and meta-analysis. Travel Med Infect Dis 2020;34:101623. https://doi.org/10.1016/j.tmaid.2020.101623 [ Links ]
19. Samsudin I, Vasikaran SD. Clinical utility and measurement of procalcitonin Clin Biochem Rev 2017;38(2):59-68. [ Links ]
20. Liu R, Ma Q Han H, et al. The value of urine biochemical parameters in the prediction of the severity of coronavirus disease 2019. Clin Chem Lab Med 2020;58(7):(epub 20 April 2020). https://doi.org/10.1515/cclm-2020-0220 [ Links ]
21. Lippi G, South AM, Henry BM. Electrolyte imbalances in patients with severe coronavirus disease 2019 (COVID-19). Ann Clinical Biochem 2020;57(3):262-265 https://doi.org/10.1177/0004563220922255 [ Links ]
22. Chen Dong, Li X, Song Qifa, Hu C, Su F, Dai J. Hypokalemia and clinical implications in patients with coronavirus disease 2019 (COVID-19). Infect Dis 2020:(epub 29 April 2020). https://doi.org/10.1101/2020.02.27.20028530 [ Links ]
23. Pan L, Mu M, Yang P, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: A descriptive, cross-sectional, multicenter study. Am J Gastroenterol 2020;115(5):766-773. https://doi.org/10.14309/ajg.0000000000000620 [ Links ]
24. Zeng JH, Liu YX, Yuan J, et al. First case of COVID-19 complicated with fulminant myocarditis: A case report and insights. Infection 2020;1-5. https://doi.org/10.1007/s15010-020-01424-5 [ Links ]
25. Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5 700 patients hospitalized with COVID-19 in the New York City area. JAMA 2020;323(20):2052-2059. https://doi.org/10.1001/jama.2020.6775 [ Links ]
26. McGonagle D, Sharif K, O'Regan A, Bridgewood C. The role of cytokines including interleukin-6 in COVID-19-induced pneumonia and macrophage activation syndrome-like disease. Autoimmun Rev 2020:(epub 3 April 2020). https://doi.org/10.1016/j.autrev.2020.102537 [ Links ]
27. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA 2020:(epub ahead of print). https://doi.org/10.1001/jamainternmed.2020.0994. [ Links ]
28. Chen X, Zhao B, Qu Y, et al. Detectable serum SARS-CoV-2 viral load (RNAaemia) is closely associated with drastically elevated interleukin-6 (IL-6) level in critically ill COVID-19 patients. medRxiv 2020(1):2020.02.29.20029520. https://doi.org/10.1101/2020.02.29.20029520 [ Links ]
29. Wang G, Wu C, Zhang Q, et al. C-reactive protein level may predict the risk of COVID-19 aggravation. Open Forum Infect Dis 2020:(epub 29 April 2020). https://doi.org/10.1093/ofid/ofaa153 [ Links ]
 Correspondence:
Correspondence:
S Omar
shahedicu@gmail.com
Accepted 25 May 2020














