Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
Southern African Journal of Critical Care (Online)
versão On-line ISSN 2078-676X
versão impressa ISSN 1562-8264
South. Afr. j. crit. care (Online) vol.34 no.1 Pretoria Jul. 2018
http://dx.doi.org/10.7196/sajcc.2017.v34i1.343
ARTICLE
Early mobilisation practices of patients in intensive care units in Zimbabwean government hospitals - a cross-sectional study
C TadyanemhanduI; H van AswegenII; V NtsieaIII
IMSc Physiotherapy; Department of Physiotherapy, School of Therapeutic Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIPhD; Department of Physiotherapy, School of Therapeutic Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIIPhD; Department of Physiotherapy, School of Therapeutic Sciences, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND. Recent evidence shows that early mobilisation of patients in an intensive care unit (ICU) is feasible, safe and associated with improvement in patients' clinical outcomes. However, its successful implementation is dependent on several factors, which include ICU structure and organisational practices.
OBJECTIVES. To evaluate the structure and organisational practices of Zimbabwean government hospital ICUs and to describe early mobilisation practices of adult patients in these units.
METHODS. A cross-sectional survey was conducted in all government hospitals in Zimbabwe. Data collected included hospital and ICU structure, adult patient demographic data and mobilisation activities performed in the ICU during the 24 hours prior to the day of the survey.
RESULTS. A total of five quaternary level hospitals were surveyed, with each hospital having one adult ICU. Four of the units were open-type ICUs. The majority of the units (n=3; 60%) reported that they had a permanent physiotherapist who covered their unit, but none of the physiotherapists worked solely in the ICU. The nurse-to-patient ratio across all units was 1:1. None of the units utilised a standardised sedation scoring system or a standardised outcome measure to assess patient mobility status. Only one ICU (20%) had a patient eligibility guideline for early mobilisation in place. Across the ICUs, 40 patients were surveyed. The median (interquartile range) age was 33 (23.3 - 38) years and 24 (60%) were mechanically ventilated. Indications for admission into the ICU included acute respiratory failure (n=12; 30%) and postoperative care (n=10; 25%). Mobilisation activities performed in the previous 24 hours included turning the patient in bed (n=39; 97.5%), sitting over the edge of the bed (n=10; 25%) and walking away from the bedside (n=2; 5%). The main reason listed for treatment performed in bed was patients being sedated and unresponsive (n=13; 32.5%).
CONCLUSION. Out-of-bed mobilisation activities were low and influenced by patient unresponsiveness and sedation, staffing levels and lack of rehabilitation equipment in ICU.
In the past, critically ill patients receiving mechanical ventilation were often managed with deep sedation and bed rest during the early stages of their intensive care unit (ICU) admission.[1] However, evidence of the strong association between prolonged sedation, bed rest and poor long-term patient outcomes has contributed to a shift in ICU clinical practice. Current research is focused on ways of reducing sedation and promoting early mobilisation; however, this is mostly described in high-income countries.[1-7]
Although literature indicates that early mobilisation is safe and feasible in critically ill adult patients,[8] not all units have adopted an early mobilisation programme as standard practice for every ICU patient.[9] Point prevalence studies in Australia and New Zealand, Germany and the USA reported very low early mobilisation practices, with standing and higher levels of mobilisation rarely occurring, especially in mechanically ventilated patients with endotracheal tubes.[10-12] A discrepancy between reported and actual delivery in clinical practice has been highlighted in relation to early mobilisation of patients [12] and successful implementation is dependent on several factors related to the organisation of ICU services. These include the type of ICU, staffing, administration, admission criteria and policies.[13] With this background, the present study aimed to investigate the structure and organisational practices in Zimbabwean government hospitals' ICUs and to describe early mobilisation practices of adult patients in these units.
Methods
Study design and study setting
Prior to commencement of the study, institutional review board approval was obtained from all government hospitals in Zimbabwe. Thereafter, permission to conduct the study was obtained from the Joint Research Ethics Committee for the University of Zimbabwe College of Health Sciences and Parirenyatwa Group of Hospitals (JREC REF: 377/15), the Medical Research Council of Zimbabwe (ref. no. MRCZ/A/2040) and the University of the Witwatersrand Human Research Ethics Committee (Medical) (ref. no. M150927).
A cross-sectional survey design was used. There are currently five government hospitals with ICUs in Zimbabwe and all were invited to participate in the survey.
Study participants
Only information about adult patients who were in an ICU on the day of the survey at each hospital was recorded. Paediatric and neonatal ICU patients were not included in this survey.
Data collection procedure
A survey questionnaire was developed using information obtained from two of the point prevalence studies referred to earlier.[10,11] The questionnaire consisted mostly of closed-ended questions. The questionnaire was sent to three experts in the field of critical care to ensure content validity and face validity. Suggested changes were implemented and the final version of the questionnaire was recirculated to the experts to obtain agreement on content. Thereafter the questionnaire was uploaded to REDCap for data collection during the survey.
Data collection was done by one person (CT) in each of the five hospitals at a pre-arranged time on different days during the period of June 2016 to August 2016. On the day of the survey, information about the hospital and the organisation and structure of each included ICU was obtained from the nursing head of shift through an informal interview. Information sought included type of hospital, number of adult ICUs in the hospital, name of ICU, description of the ICU, bed capacity, average monthly patient admissions over the last three months, ratio of ICU staff to patients, whether multidisciplinary ward rounds were held routinely, type of beds and chairs in the unit, availability of clinical guidelines for patient management, availability of mobility equipment, type of patients admitted in the unit, staff who were routinely involved in mobilisation of patients and which procedures, if any, were implemented in the ICU to promote early mobilisation. The type of ICU was defined as 'open' or 'closed'. Closed ICUs were defined as those that required patient transfer to or mandatory patient co-management by an intensivist, and open ICUs as units where patient care was provided by a variety of doctors.
The variables for which data were collected from patients' ICU charts and files included demographic (age, gender) and clinical information (admission diagnosis, cause of condition, reason for ICU admission, number of days in ICU, number of days on mechanical ventilation, Acute Physiology and Chronic Health Evaluation (APACHE) II score, Sequential Organ Failure Assessment (SOFA) score and comorbidities) and mobilisation practices performed on patients in ICU by clinical staff in the previous 24 hours of their ICU stay. Activities screened for and recorded included: (i) remained in bed with treatment mostly in a supine position; (ii) turned in bed during treatment; (iii) passive range of motion exercises; (iv) active-assisted exercises; (v) active exercises; (vi) sitting up in bed; (vii) sitting up over the edge of the bed; (viii) sitting out of bed in a chair; (ix) standing upright next to the bed; (x) stepping (marching) by the bedside; and (xi) walking away from the bed side. The ICU physiotherapist was interviewed firstly regarding their workload and secondly to clarify reasons why some patients might not have been mobilised in the 24-hour period prior to the survey. Potential barriers which were listed in the questionnaire were mentioned when physiotherapists were interviewed, and the reasons which were not included in the questionnaire were recorded under 'other'. The last section of the survey questionnaire recorded adverse events which occurred as a direct result of mobilisation.
Data analysis
The data obtained were nominal, ordinal and ratio in nature. Data were captured from REDCap onto an Excel spreadsheet. Statistical Package for Social Sciences (SPSS) version 24 for Windows was used to analyse data. Descriptive statistics were used to present the data. Continuous variables were summarised as mean and standard deviation for normally distributed data or median and interquartile range. Categorical variables were summarised as frequencies and percentages. X and Fisher's exact tests were used to test relationships between categorical data. A p-value <0.05 was deemed statistically significant. All qualitative interview data obtained from open-ended questions during informal interviews were summarised into themes and the items within each theme were summarised using frequencies and percentages.
Results
Hospital and ICU structure
Table 1 summarises information obtained regarding government hospitals and their ICU characteristics. Of the 5 hospitals, 3 had separate adult and paediatric ICUs and 2 of the hospitals only had 1 unit for both adult and paediatric patients. The majority of the units were open-type settings (n=4; 80%) and all of the 5 units were mixed medical and surgical ICUs. The median (interquartile range (IQR)) bed capacity of the units on the day of the survey was 7 ( 6 - 8.5) patients and the median (IQR)) monthly admission rate was 39 (23.5 - 45.5) patients. The nurse-to-patient ratio across all units was 1:1. There was an average of 1 - 3 intensive care-trained registered nurses per shift together with student nurses. The number of physiotherapists covering the units ranged between 1 and 2 per hospital. The majority of the units (n=3; 60%) reported that they had a permanent physiotherapist who covered their unit but none of the physiotherapists worked solely in the ICUs. A permanent physiotherapist was defined as a therapist who always covered the adult ICU and other specific wards or areas and did not rotate through other areas. The 3 physiotherapists who were covering 3 of the units were all senior physiotherapists with more than 5 years of experience. The remaining 2 units had 2 physiotherapists covering each unit. For one of these units, both physiotherapists were senior but, in the other unit, one was senior and the other junior. The physiotherapist to patient ratio ranged across units from 1:4 to 1:9 depending on the ICU bed capacity.
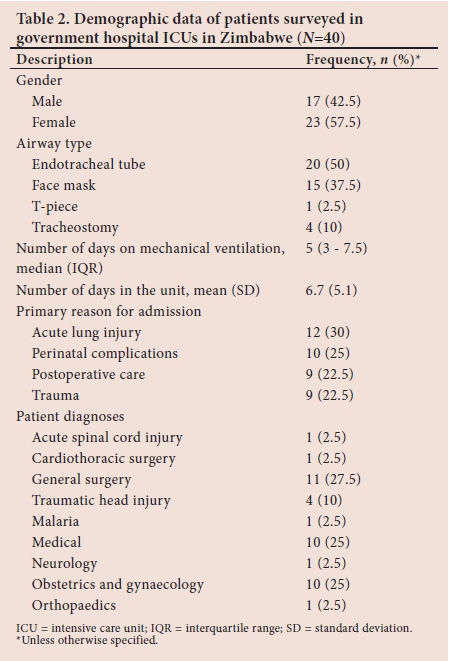
Demographic details of patients in the units on the day of the survey
Across the 5 units, 40 patients were surveyed. Table 2 summarises the demographic information of ICU patients on the day of the survey. The median (IQR) age of the patients was 33 (23.3 - 38) years, the majority were female (n=23; 57.5%), and 24 (60%) were mechanically ventilated with a median (IQR) duration of ICU stay of 5 (3 - 8) days. A total of 39 patients (97.5%) had stayed in the unit for more than 24 hours and 27 patients (67.5%) had stayed in the unit for more than 5 days on the day of the survey. The method of ventilation for the majority of patients was via endotracheal tube (ETT) (n=20; 83.3%). Indications for admission into ICU included acute respiratory failure (n=12; 30%) and postoperative care (n=10; 25%) (Table 2). No APACHE II or SOFA scores were recorded for patients in any of the ICUs surveyed as this did not form part of routine patient care in these units at the time.
Current mobilisation practices
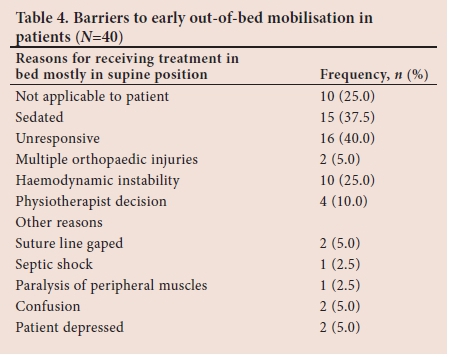
Table 3 summarises the types of mobilisation activities that were performed with patients in the previous 24 hours. These activities included turning the patient in bed (n=39; 97.5%), standing the patient next to the bed (n=4; 10%), marching on the spot (n=3; 7.5%) and walking away from the bedside (n=2; 5%). The highest level of mobilisation achieved by the majority of patients was turning in bed (n=23; 57.5%), with only 2 of the patients (5%) achieving walking on the day prior to the survey (Table 3). Out of bed mobilisation, which included activities starting from sitting over the edge of the bed and progressing to walking, was done with 10 (25%) patients. Two of the patients mobilised out of bed were on mechanical ventilation.
The most common barriers to mobilisation are summarised in Table 4. These included patients who were sedated and unresponsive (n=13; 32.5%) and those with haemodynamic instability (n=10; 25%) (Table 4). Other reasons why physiotherapists decided not to mobilise patients out of bed included gaping of a surgical suture site, paralysis of peripheral muscles due to Guillain-Barré syndrome and, lastly, patients who were depressed. Adverse events related to mobilisation were orthostatic hypotension when sitting over the edge of the bed (n=1; 2.5%) and a large volume of puss oozing from an incision site when a patient was standing next to the bed (n=1; 2.5%).
ICU culture to promote early mobilisation
All the ICUs surveyed indicated that they had discipline-specific unit rounds every day but only 2 units (40%) reported that multidisciplinary rounds were held daily in their units with physiotherapists always participating. All ICUs reported that nurses and physiotherapists were responsible for patient mobilisation. None of the ICUs had structured protocols in place regarding patient management (for example, using a standardised sedation scoring system) but some had guidelines related to documentation of patient goals, setting daily sedation goals for patients and assessment of patients' mobility status. Only one unit had guidelines for patient eligibility for early mobilisation. Regarding equipment available in the units, all (N=5) had standard chairs with arm and back rests, oxygen cylinders, electronic hospital beds and ambubags, but the availability of portable ventilators (n=2; 40%) was limited. None of the ICUs reported having rehabilitation equipment available such as walking frames, sliding boards, transfer boards, hoists, standing hoists, tilt tables, standing frames or cycle ergometers.
Factors associated with mobilisation activities
Table 5 summarises factors that had a relationship with mobilisation activities performed with patients in the ICU. Factors that were found to have a significant relationship with out-of-bed patient mobilisation were a closed type of ICU setting (p=0.0003), permanent physiotherapy cover in the unit (p=0.03), physiotherapist attendance of multidisciplinary ward rounds (p=0.01), patients ventilated via a face mask (p=0.01), and patients not sedated (p=0.005).
Discussion
Inactivity, deconditioning and muscle weakness is associated with critical illness.[10] Early out-of-bed mobilisation, that includes walking at or away from the bedside, initiated in ICU for patients who are intubated and receiving mechanical ventilation is advocated to reduce the onset of muscle weakness and to improve patient outcomes.[1,2,10,11] Results from this cross-sectional study show that patients in ICU in government sector hospitals in Zimbabwe perform a range of mobilisation activities during their stay. The majority of these activities were performed in bed and therefore the incidence of out-of-bed activities was low (25%), with only 5% of patients walking away from the bedside. In this mixed cohort of medical and surgical patients, the majority who mobilised out of bed received oxygenation through a face mask. Factors significantly associated with out-of-bed mobilisation activities were: a closed ICU setting, permanent physiotherapy cover in the unit, physiotherapy attendance at multidisciplinary ward rounds and no patient sedation. No other surveys have reported on mobilisation practices in Zimbabwean hospital ICUs to date.
Similarities were found between our results and those reported by other point prevalence studies on early mobilisation of patients in ICU.[10-12] Cohorts that were investigated in Australia, New Zealand, Germany and the USA also consisted of patients with medical and surgical conditions.[10-12] Low incidences of out-of-bed mobilisation were reported by Jolley et al.[12] and Nydahl et al.[11] (16% and 24%, respectively), similar to our finding of a 25% mobilisation rate. The incidence of out-of-bed mobility for those ventilated through an ETT was low in the current cohort of patients (5%) and similarly low incidences were reported by Berney et al.[10] and Nydahl et al.[11] (10% and 0.2%, respectively). This low incidence of mobilisation for those with ETT may be explained by the more frequent use of sedation in these patients, their shorter ICU length of stay and the fact that they might be more unstable from a cardiovascular point of view.[11] In the absence of data related to severity of illness (APACHE II scores) and level of morbidity in ICU (SOFA scores) for the current cohort of patients, it is not known whether they were more sick and therefore managed predominantly in bed.
More than one-third of the patients in the present study were managed in bed due to sedation and unresponsiveness. This finding may be supported by the fact that none of the units who participated in this study reported having protocols in place to manage patient sedation or pain levels, and only one unit had eligibility criteria in place to monitor patient readiness for mobilisation. Jolley et al[12] reported that the presence of delirium was negatively associated with out-of-bed mobilisation. Use of bedside sedation scales may move the ICU team away from use of deep and prolonged sedation towards continuous targeted light sedation with drugs that are relatively short acting and easier to titrate.[7] Evidence suggests that early mobilisation of patients is not delivered to all patients who might benefit from it due to unavailability of objective criteria that indicates that it is safe to initiate mobilisation.[1] It has been suggested that stepwise protocols be implemented in ICU to assist clinicians in prescribing mobilisation activity based on patients' cognitive levels and physical capacity in order to prioritise mobilisation activities as part of routine clinical service delivery.[10] However, Nydahl et al.[11] reported that 75% of participating units had protocols in place for monitoring levels of patient sedation and pain and that 71% had protocols in place for early mobilisation of patients in ICU. Despite the presence of these clinical protocols, more than half of their participants were managed in bed.[11] It is thus fair to conclude that the culture of early mobilisation of patients in ICU has not been universally adopted by clinicians in Zimbabwean government hospital settings or elsewhere in the world. Since there is underutilisation of guidelines by the ICU teams in Zimbabwean ICUs, there is a need to explore further the attitude and beliefs of clinicians about use of clinical practice guidelines in patient care and the factors associated with their acceptance and use.
Other factors that may influence mobilisation activities performed with patients with critical illness in Zimbabwean ICUs is the staff to patient ratio and level of availability of rehabilitation and transfer equipment in these units. In this study, we report that one nurse provides care for one patient and that one physiotherapist provides care for up to 9 patients in some ICUs. All units reported that nurses and physiotherapists were responsible for mobilisation of patients. This is in contrast to the high ICU staffing levels reported in Germany where the mean nurse to patient ratio is 2.4 and physiotherapist to patient ratio is 9.7.[11] In the German study, nurses and physiotherapists were mostly involved in mobilisation of patients, with physicians assisting at times. Most of the participating units reported having transfer and lifting devices available as well as rehabilitation equipment such as tilt tables and walkers.[11] In the current study, none of the units had transfer or rehabilitation equipment available. Therefore, the low staffing levels and lack of readily available equipment in Zimbabwean government ICUs are likely to impact the frequency with which mobilisation activities are performed in these units.
Patients were mobilised out of bed in units which had permanent physiotherapy cover, not rotating through the other wards. Possible advantages of having a permanent physiotherapist in a unit is that it promotes standardisation of practices, improvement in knowledge of the physiotherapist in ICU-related issues and sustainability of intervention programmes. If the physiotherapist is permanently based in the unit, this may promote formulation of practice guidelines which can be implemented as compared to when physiotherapists have to rotate from one area to the other after a period of only three to four months, which is standard practice in Zimbabwean government hospitals. The unit that had an eligibility criteria guideline for patient mobilisation was an open type of ICU, but the physiotherapist was permanently based in that unit. Closed-type ICU settings may more readily result in standardisation of practice since all decisions related to patient management are generally made by one intensivist, and through multidisciplinary ward rounds best patient management is discussed by the whole team. The knowledge and attitude of the intensivist towards early mobilisation becomes a key component in the closed type of ICU as the intensivist serves as the champion leader in the implementation of the intervention in the unit. In contrast, all participating units in the Australia and New Zealand survey were closed units and yet no patients on mechanical ventilation for longer than 48 hours stood, sat out of bed or walked in the unit on the day of the survey.[10] This supports the notion that the culture of early mobilisation of patients with critical illness is not yet adopted by all clinicians who work in ICU.
The barriers to mobilisation of patients out of bed listed by participants in the current study are similar to those reported by Nydahl et al.[11] in relation to haemodynamic instability, sedation, unresponsiveness and unstable fractures. Patient weakness was mentioned as a barrier to mobilisation in this study as well as the Australia and New Zealand point prevalence study.[10] Two barriers to mobilisation reported in this study, that have not been reported by others, are gaping open of a surgical suture site and patient depression. Emotional stress, defined as depression, anxiety, or hostility, is common in critical illness and may be due to multiple physical, psychological and environmental factors associated with a busy ICU.[14] Depression, anxiety and hostility might also decrease if patients perceive movement as an improvement in clinical status.[14] A review of meta-analyses on the effect of exercise on anxiety and depression was recently published.[15] This review included 48 207 people and results showed that exercise therapy had a large effect size on reducing levels of depression experienced.[15] Clinicians should be trained on patient screening and safety related to out-of-bed mobilisation activities in ICU to reduce perceived barriers to exercise and mobilisation and improve clinical service delivery.[11] The low rate of adverse events reported in our survey (5%) was consistent with the 5% reported by Berney et al.[10]All adverse events reported were minor in nature.
The study had some limitations. Data collection was based on review of patient notes and clarifying with the attending nurse or physiotherapists on the mobilisation practices done and reasons why some patients were not mobilised. There might be bias in the documentation of the information by clinicians, with some information not written down and bias in answering questions which assessed potential barriers. All participants were, however, informed that the survey data collected would be anonymous. This was done in an attempt to reduce reporting bias. All point prevalence studies on mobilisation activities in ICU to date have used patient record review to collect data and all reported similar findings to ours regarding low out-of-bed mobilisation activities.[10-12] The study design itself has been reported to be a limitation by Berney et al.[10] as it may not represent actual clinical practice. Future studies should focus on carrying out prospective evaluation of mobilisation practices in ICU and should determine the factors associated with uptake of already developed mobilisation guidelines in clinical practice.
Conclusion
Out-of-bed mobilisation activities in Zimbabwean government hospital ICUs were low and influenced by patient unresponsiveness and sedation, absence of clinical protocols for patient management, low staffing levels in ICU and unavailability of rehabilitation equipment. Standardisation of practice through adoption of already existing guidelines for patient management may be key to improve service delivery to all patients in ICU. There is a need for implementation of quality improvement projects in these units with the overarching goal of making changes that result in better patient outcomes through provision of well-established clinical interventions and better professional development.
Acknowledgements. The authors would like to thank all the hospitals that participated in the survey and a special acknowledgement goes to the ICU staff and the patients who made the project successful.Author contributions. All authors contributed equally to the preparation of the manuscript.Funding. This work was supported by the Fogarty HIV Implementation Science Research Training Program (University of Zimbabwe) and the Medical Faculty Research Endowment Fund (WITS University). The funding sources had no role in study design, data collection, data analysis, data interpretation, in writing the report, nor in the decision to submit the article for publication.Conflicts of interest. None.
Acknowledgements. The authors would like to thank all the hospitals that participated in the survey and a special acknowledgement goes to the ICU staff and the patients who made the project successful.
Author contributions. All authors contributed equally to the preparation of the manuscript.
Funding. This work was supported by the Fogarty HIV Implementation Science Research Training Program (University of Zimbabwe) and the Medical Faculty Research Endowment Fund (WITS University). The funding sources had no role in study design, data collection, data analysis, data interpretation, in writing the report, nor in the decision to submit the article for publication.
Conflicts of interest. None.
References
1. Hodgson CL, Stiller K, Needham DM, et al. Expert consensus and recommendations on safety criteria for active mobilization of mechanically ventilated critically ill adults. Crit Care 2014;18(6):658. https://doi.org/10.1186/s13054-014-0658-y [ Links ]
2. Bailey P, Thomsen GE, Spuhler VJ, et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med 2007;35(1):139-145. https://doi.org/10.1097/01.CCM.0000251130.69568.87 [ Links ]
3. Bourdin, G, Barbier, J, Burle, JF, et al. The feasibility of early physical activity in intensive care unit patients: A prospective observational one-center study. Respir Care 2010;55(4):400-407. [ Links ]
4. Balas MC, Burke WJ, Gannon D, et al. Implementing the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle into everyday care: Opportunities, challenges, and lessons learned for implementing the ICU Pain, Agitation, and Delirium Guidelines. Crit Care Med 2013;41(9):S116-S127. https://doi.org/10.1097/CCM.0b013e3182a17064. [ Links ]
5. Carrothers KM, Barr J, Spurlock B, et al. Contextual issues influencing implementation and outcomes associated with an integrated approach to managing pain, agitation, and delirium in adult ICUs. Crit Care Med 2013;41(9):S128-S135. https://doi.org/10.1097/CCM.0b013e3182a2c2b1. [ Links ]
6. Harrold ME, Salisbury LG, Webb SA, et al. Early mobilisation in intensive care units in Australia and Scotland: A prospective, observational cohort study examining mobilisation practices and barriers. Crit Care 2015;19(1):336. https://doi.org/10.1186/s13054-015-1033-3 [ Links ]
7. Vincent JL, Shehabi Y, Walsh TS, et al. Comfort and patient-centred care without excessive sedation: The eCASH concept. Intensive Care Med 2016;42(6):962-971. https://doi.org/10.1007/s00134-016-4297-4 [ Links ]
8. Cameron S, Ball I, Cepinskas G, et al. Early mobilization in the critical care unit: A review of adult and pediatric literature. J Crit Care 2015;30(4):664-672. https://doi.org/10.1016/j.jcrc.2015.03.032 [ Links ]
9. Barber EA, Everard T, Holland AE, et al. Barriers and facilitators to early mobilisation in intensive care: A qualitative study. Aust Crit Care 2014;28(4):177-182. https://doi.org/10.1016/j.aucc.2014.11.001 [ Links ]
10. Berney SC, Harrold M, Webb SA, et al. Intensive care unit mobility practices in Australia and New Zealand: A point prevalence study. Crit Care Resus 2013;15(4):260. [ Links ]
11. Nydahl P, Ruhl AP, Bartoszek G, et al. Early mobilization of mechanically ventilated patients: A 1-day point-prevalence study in Germany. Crit Care Med 2014;42(5):1178-1186. https://doi.org/10.1097/CCM.0000000000000149 [ Links ]
12. Jolley SE, Moss M, Needham DM, et al. Point prevalence study of mobilization practices for acute respiratory failure patients in the United States. Crit Care Med 2017;45(2):205-215. https://doi.org/10.1097/CCM.0000000000002058 [ Links ]
13. Bakhru RN, McWilliams DJ, Wiebe DJ, et al. Intensive care unit structure variation and implications for early mobilization practices. An international survey. Ann Am Thorac Soc 2016;13(9):1527-1537. https://doi.org/10.1513/AnnalsATS.201601-078OC [ Links ]
14. Klein K, Mulkey M, Bena JF, et al. Clinical and psychological effects of early mobilization in patients treated in a neurologic ICU: A comparative study. Crit Care Med 2015;43(4):865-873. https://doi.org/10.1097/CCM.0000000000000787 [ Links ]
15. Wegner M, Helmich I, Machado S, et al. Effects of exercise on anxiety and depression disorders: Review of meta-analyses and neurobiological mechanisms. CNS Neurol Disord Drug Targets 2014;13(6):1002-1014. https://doi.org/10.2174/1871527313666140612102841 [ Links ]
 Correspondence:
Correspondence:
C Tadyanemhandu
cathytadya@gmail.com
Accepted 15 March 2018














