Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
Southern African Journal of Critical Care (Online)
versão On-line ISSN 2078-676X
versão impressa ISSN 1562-8264
South. Afr. j. crit. care (Online) vol.33 no.1 Pretoria Jul. 2017
http://dx.doi.org/10.7196/SAJCC.2017.v33i1.281
ARTICLE
Lived experiences of Rwandan ICU nurses caring for patients with a do-not-resuscitate order
E NankundwaI; P BrysiewiczII
IRN, M Critical Care & Trauma Nursing; School of Nursing and Midwifery, School of Medicine and Health Sciences, University of Rwanda, Kigali, Rwanda
IIPhD; School of Nursing and Public Health, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND. Do not resuscitate (DNR) is the policy and practice of deliberately not attempting to resuscitate a person whose heart has stopped beating. Research on nursing care for patients designated with DNR orders has been conducted since the late 1980s; however, no study appears to have been carried out in the Rwandan setting.
PURPOSE. The purpose of this study was to explore the lived experiences of nurses caring for a patient with a DNR order in an intensive care unit (ICU) in Kigali, Rwanda, in order to suggest nursing recommendations.
METHODS. Using a phenomenological approach, two semi-structured interviews were conducted with each participant to explore their lived experiences of caring for patients with DNR orders. The sample comprised six nurses from an ICU in a large tertiary-level hospital in Kigali, Rwanda.
RESULTS. The data were organised into categories based on a review of the data from the interviews of the six participants. The categories were: feeling emotional distress; barrier to optimal care; and not part of decision-making.
CONCLUSION. DNR orders are a fairly new concept in Rwanda and the practice of DNR orders in ICU is very demanding for the staff, especially the ICU nurses. Additional education about DNR orders as well as policies to guide its implementation could assist ICU nurses in their difficult work.
Do not resuscitate (DNR) is the policy and practice of deliberately not attempting to revive a person whose heart has stopped beating, i.e. to withhold resuscitation.[1] The DNR decision does not signify abandonment of the patient, but is rather part of the actions that favour the patient's wellbeing in order to make a peaceful death possible.[2] DNR can in fact play an active role in patient care although its interpretation can modify the therapeutic approaches to patient care. This may lead to inadequate treatment,[3] and may cause the healthcare team to do less than their best for the patient, which may lead to abandonment of the patient.[4] End-of-life decisions are complex for any healthcare worker, especially for the intensive care unit (ICU) nurse, as they have to shift the treatment from aggressive life-saving therapy to end-of-life care. [5] It has been shown that many doctors and nurses feel unprepared to facilitate end-of-life decision-making and are unclear regarding some of the legal aspects of the DNR order.[6]
The decision to not resuscitate is difficult to reach, therefore a DNR order should be based on a proper agreement between all the members of the healthcare team, the patient, and their family, where possible. The procedure of this decision-making must be clear and well documented, although communication about DNR can be challenging and highly stressful. Many studies illustrate that nurses, patients and family involvement in this decision making process is low, with the doctor as the major decision-maker.[7,8] Nurses' voices are often absent in such end-of-life decision-making.[3,7] It is recommended that the DNR decision is made involving the whole team looking after the patient and it should then be written clearly in the patients' notes, and regularly reviewed.[9]
Rwanda is a small country located in East Africa. After the genocide in 1994, the country experienced many challenges involving access to quality healthcare and lack of human resources. Intensive care medicine or critical care services are poorly developed, or at best still in their infancy. Special ICUs, such as neurological and neonatal ICUs, are still a novel concept and there is a severe lack of experienced and specially trained medical and nursing staff in the ICUs.[10] Research conducted regarding DNR policies has shown that in some low- and middle-income countries like Rwanda, guidelines to support the DNR decision and end-of-life care do not exist or their development is still in the early stages.[7,8,11] In Rwanda, people tend to deny death, believing that medical science can cure any patient. Death is often seen as a failure of the healthcare system, rather than a natural aspect of life. This belief affects all healthcare professionals, including nurses, because they consider that if a patient is in hospital the purpose is to restore life and not allow them to die.[12]
Research on nursing care for patients designated with DNR orders has been conducted since the late 1980s; however, no study appears to have been carried out in the Rwandan healthcare setting, although DNR orders are commonly used in some of the hospitals. This study may provide more information about the practice of DNR orders from the perspective of the nurses working in the ICU and may add to a limited body of knowledge. The purpose of the study was to explore the lived experiences of nurses caring for a patient with a DNR order in an ICU in Kigali, Rwanda.
Methods
Using a phenomenological approach,[10] two in-depth individual interviews were conducted with each participant to explore their lived experiences of providing care to patients with a DNR order in the ICU. The use of this approach allowed the researchers to gain a deeper understanding of the participants' experiences.
Research setting
The study was conducted with nurses working in the seven-bedded ICU of a 200-bed tertiary hospital in Kigali, Rwanda. The ICU at the hospital is a medical-surgical unit, receiving both adult and paediatric patients. The ICU receives patients with life-threatening conditions directly into the ICU or from other departments within the hospital. At the time of this research study, hospital records indicated that ~20 patients were admitted to the ICU monthly.
Study sample
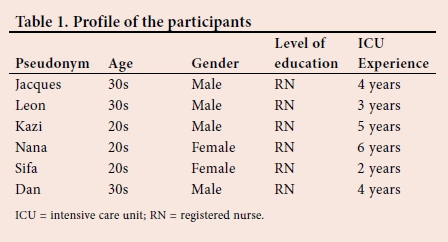
Purposive sampling was used to include nurses working in the ICU in the research setting, who were registered with the Rwanda Nursing Council, had at least 6 months' experience in the ICU, and expressed interest in participating in the study.
The final decision about sample size was based on evidence of data saturation, which was said to have occurred when no new information of significance was obtained and the participants started to repeat facts which were already submitted by other participants during the interviews.1131 In the current study six participants were interviewed.
Data collection
Following ethical approval and permission from the university research committee and the hospital administration, the researcher facilitated access to the participants through their ICU unit manager. Interviews were held with the cooperation of the unit manager in a quiet, distraction-free venue close to the ICU, between August and September 2011.
Two semi-structured individual interviews were conducted with each participant and lasted ~25 - 30 minutes. The interviews were conducted in either English or Kinyarwanda, depending on the preference of the participant, and the researcher was fluent in both languages. The interview started with the following question: 'Please can you tell me about your most recent experience of nursing a patient with a DNR order in the ICU?' Further questions were then asked as to whether the DNR order influenced the nursing care in any way, and if the participants had any nursing recommendations for the use of the DNR order in an ICU.
All interviews were recorded with the permission of the participants. The second interviews were then used to verify the findings from the first interview. The researcher was known to the participants, as she had previously worked in the units. This was found to facilitate access to the participants, build rapport, and did not appear to negatively influence the data-collection process. However, it may have influenced the participants' responses as they may have provided answers that they thought the researcher wanted to hear.
Data analysis
All interviews were transcribed into written English text by the researcher and a language expert from a local university checked the transcripts for accuracy. The data were then manually analysed using Giorgi's phenomenological approach[14] The researchers read and reread the interviews several times to get a sense of the whole. The text was divided into units and then transformed into meaning by selecting descriptive quotations from the text. The meanings were then grouped together and developed into categories to create a general description of the nurses' experience.[14]
Trustworthiness
Credibility was achieved through prolonged engagement as the researcher had previously developed a rapport with the participants while working with them as a student, after which she spent 2 months collecting the data. This helped to ensure that rich, useful data were collected. All the potential participants approached were given the opportunity to refuse participation in the study, so that those interviewed were willing and interested to participate. It was emphasised to the participants that they should be frank in telling their stories and that there was no correct answer. Frequent debriefing sessions were held between the researchers to discuss the developing ideas and interpretations, and to challenge assumptions. Feedback was provided to the participants regarding the categories emerging from the data in order to obtain their reactions and to explore whether the interpretations were a good representation of their reality.1151 In an attempt to ensure dependability, the researchers described the decision-making processes and the context of the research study in detail. Transferability was ensured by providing a sufficiently detailed description of the research process to aid the reader in deciding if the findings could be transferred to a similar context. Confirmability was ensured by undertaking an audit trail and providing information regarding the path that the researchers took and how they arrived at their interpretations.[15]
Ethical considerations
Permission to conduct the study was obtained from the ethics research committee at the University of Rwanda, as well as the hospital where data collection took place. Participation was voluntary and written informed consent was obtained from all participants, who were informed of their right to withdraw from the research at any time. Confidentiality was assured through use of pseudonyms so that data could not be traced back to individuals. The data were kept in a secure place, available only to the research team.
Results
The data were organised into categories based on a review of the data obtained from the interviews of the six participants (Table 1). Three categories emerged from the data:
• feeling emotional distress
• barrier to optimal care
• not part of decision-making.
Feeling emotional distress
The participants referred to the emotional distress they experienced while providing care to a DNR patient. They viewed the DNR orders as permitting death to occur and giving permission to terminate a patient's life. One of the participants said:
'When the decision are made [itj is ... too hard and painful ... eeeeh ...
I can't believe it because it is like he said the death is coming up and
we can't do anything . to the patient.' (Dan)
Another said:
'Watching their death is a very difficult experience ...eeeeeeh ... and when you know that patient with cardiac arrest will not receive CPR.' (Leon)
Participants felt despair while caring for the DNR patients because there was no longer anything they could do for the patient:
When we consider that restore [restoring) to health is no longer possible for patient with DNR we feel desperation and disappointed.'
(Nana)
'When a patient is designated with a DNR order, I feel not comfortable to discover that really there is no hope that the patient will recover ... he is really departed.' (Sifa)
A participant also went further to explain feeling a moral conflict with the DNR decision, i.e. whether to act on the decision or not. He said: 'As nurses, our moral[s] may be in conflict with the decision because we are left with the decision of whether to initiate the CPR or not, many times we attempt the CPR ... and believe that those patients can recover.' (Dan)
'I'm worrying about them ... because withdrawing ... looks like killing [the] patient.' (Leon)
Barrier to optimal care
The participants described how the presence of a DNR order became a barrier to providing optimal care for the patient. Participants felt that patients with a DNR order could receive less intensive care and some of the daily nursing activities would not be performed as well as usually done.
A participant said:
'Yeah ... It can influence the nursing care for instance, vital sign monitoring are not well performed. You can't do pressure area care to prevent bed sores. You can't feed him via nasogastric tube. Sometimes we can't concentrate on urine output, or fluid intake . Yeah . It continue[s] to affect some range of nursing care.' (Dan)
Participants mentioned that DNR orders resulted in the patient being abandoned by the staff:
Another factor influencing nurse's care for DNR patients is that the decision make(s) the patient abandoned, so the effect is that (the) patient receive(s) less attention. (Jacques)
'Yeah . there is a change . patients without a DNR will be treated differently.' (Leon)
Another participant mentioned:
'I think there is a general feeling that DNR have a negative impact on care. I personally was unable to care for the patient because I could not ignore the medical doctor for making this decision.' (Jacques)
Not part of decision-making
Participants explained that the doctors were the ones who made the end-of-life DNR decisions and nurses were expected to adhere to these decisions, whether they agreed with them or not. Participants explained:
'Usually the decision is made by doctors and nurses are the one[s] to implement it.
(Nana)
This lack of involvement was mentioned by two other participants: 'Most of the time we are not part of the discussion and the views of nurses are ignored. The doctors are the one who make this order.'
(Jacques)
'Normally physician, anesthesiologist, and neurosurgeons, after patient assessment make the decision; nurses are not included in the discussion, it's very painful.'
(Dan)
The participants went further to explain that the DNR decisions were not always documented or were unclear in the patients' files. This lack of documentation created problems at times:
'Sometime we apply resuscitation measures wrongly because it is not written in the patient records.'
(Leon)
A participant explained a possible reason for why the DNR order was not documented:
' Listen . the doctors fear to write do not resuscitate . I think its Rwandan culture. We ... I always feel God may be the one who can decide about life and dying ... they are not sure about the decision and think: How can I make this decision? Perhaps he will survive.' (Dan)
Discussion
In this study, participants described their emotional distress in response to DNR orders for patients in their care. Studies have shown that when the DNR decision is written it is followed by the real probability of death, and this makes nurses feel morally discouraged, with feelings of stress, frustration, anger, sadness, helplessness, and moral distress. Moral distress is associated with the powerlessness of the nurse to influence the end-of-life decisions, especially when they believe that the care provided to the patient is in conflict with patients' families' wishes, or that the nurse is powerless to carry out what they believe to be right.[16,17] To address this issue, ethical education in nursing practice is essential for nurses working in ICUs, where ethical decision-making is needed on a regular basis.[18]
Some healthcare providers consider that DNR orders result in the patient being abandoned and some doctors perceive that patients with a DNR order receive less attention from the nurses. This was confirmed in a study describing the medical handover from the night staff team, where patients with DNR orders were not recorded, as the team had decided that these patients did not need to be assessed and treated like other patients.[19] Petri? et al.ll]agreed that the DNR order is akin to organising death. In contrast, a systematic review showed that DNR orders were found to be associated with lower quality of care, but an increased quality of life.[20] Following the clear decision of DNR, the care of the patient becomes calmer and the nurses then have more time to be with the patient and family, with more active communication, instead of focusing on technical medical tasks.[18,21]
The nurses in the current study described how they were not part of the DNR decision-making process. This was in agreement with the findings of another study,[22] which highlighted the dissatisfaction of nurses during the DNR decision-making process due to inadequate collaboration, including failure to consider nurses' opinions. As a consequence, the nurse then feels uncomfortable and frustrated because they feel that the doctors do not listen to their concerns.[23] Miscommunication between nurses and doctors may affect the relationship with patients, particularly in instances where they have different opinions about the plan of care. Our results illustrate that discussion and decision-making regarding DNR orders were directed by the doctors; the nurses' input was limited. Many researchers agree that DNR decisions are usually made by physicians alone.[24] Moreover, another study has shown that doctors avoid discussion and the involvement of nurses and patients' families in this process for fear of destroying hope and the therapeutic relationship.1211 Nurses who deliver terminal care in an ICU must plan the key interventions to improve the quality of care. Nurses believe that they know the patient best, but are often not solicited by the doctors when making decisions regarding care.[25]
Several studies agree that DNR orders are often not recorded and that doctors wait until the patient shows definite signs of deterioration, or until the patient is clearly dying, to do so. It may then be too late to complete the process of adequate collaborative discussion and documentation.14,7,81 Pettersson et al.[21]state that the lack of a clear decision regarding a DNR order, or inadequate reporting and documentation of this order, creates obstacles to providing high-quality nursing care and could result in unintended CPR.
Study recommendations
Implementation of training related to DNR orders is needed for all health professionals working in ICU, specifically regarding how to collaborate as a team regarding these decisions. The rationale for DNR orders needs to be better articulated and understood by all healthcare professionals working in the ICU. Additional information on how to cope with such stressful situations also needs attention. In addition, nurses need training on how to communicate with the rest of the healthcare team and the patients' families about DNR decisions. The nursing care of a patient with a DNR order at the end of life should be incorporated into the curriculum of nurses at all levels of nursing education. Policies to guide DNR orders in ICU should be developed and implemented to assist all healthcare professionals.
Study limitations
This research was conducted in the ICU of one tertiary hospital in Rwanda, and thus only reflects the experience of nurses working there. The presence of the researcher could have influenced the participants' responses, in that the participants may have provided answers in accordance with what they thought the researcher wanted to hear.
Conclusion
DNR orders are a fairly new concept in Rwanda and the practice of DNR orders in ICU is very demanding for the staff, especially the ICU nurses. Additional education about DNR orders as well as policies to guide their implementation could assist the ICU nurses in their difficult work.
Acknowledgements. None.
Author contributions. Both EN and PB (research supervisor) contributed to all aspects of the study and writing of the manuscript. EN collected the data.
Funding. None.
Conflict of interest. None.
References
1. Petris A, Cimpoeşu D, Costache I, Rotariu I. Do not resuscitate decision: Ethical issues during cardiopulmonary resuscitation. Rev Rom Bioet 2011;9(2):99-108. [ Links ]
2. Rudnick A, Wada K. Introduction to bioethics in the 21st century. In: Rudnick A, ed. Bioethics in the 21st Century. InTech, 2011. http://dx.doi.org/10.5772/19392 [ Links ]
3. Coffey A, McCarthy G, Weathers E, et al. Nurses' preferred end-of-life treatment choices in five countries. Int Nurs Rev 2013;60(3):313-319. https://dx.doi.org/10.1111/inr.12024 [ Links ]
4. Bach V, Ploeg J, Black M. Nursing roles in end-of-life decision making in critical care settings. West J Nurs Res 2009;31(4):496-512. https://dx.doi.org/10.1177/0193945908331178 [ Links ]
5. Sham CO, Cheng YW, et al. Do-not-resuscitate decision: The attitudes of medical and non-medical students. J Med Ethics 2007;33(5):261-265. https://doi.org/10.1136/jme.2005.014423 [ Links ]
6. Shanawani H, Wenrich MD, Tonelli MR, Curtis R. Meeting physicians responsibilities in providing end-of-life care. Chest 2008;133(3):775-786. https://doi.org/10.1378/chest.07-2177 [ Links ]
7. Miller S, Dorman S. Resuscitation decisions for patients dying in the community: a qualitative interview study of general practitioner perspectives. Palliat Med 2014;28(8):1053-1061. https://dx.doi.org/10.1177/0269216314531521 [ Links ]
8. Chen YY, Gordon NH, Connors AF, Garland A, Chang SC, Youngner SJ. Two distinct do-not- resuscitate protocols leaving less to the imagination: An observational study using propensity score matching. BMC Med 2014;12:146. https://dx.doi.org/10.1186/s12916-014-0146-x [ Links ]
9. Cardozo M. What is a good death? Issues to examine in critical care. Br J Nurs 2005;14(20):1050-1060. https://doi.org/10.12968/bjon.2005.14.20.20046 [ Links ]
10. Munyiginya P, Brysiewicz P, Mill J. Critical care nursing practice and education in Rwanda. S Afr J Crit Care 2016;32(2):55-57. https://dx.doi.org/10.7196/SAJCC.2016.v32i2.272 [ Links ]
11. Cohn S, Fritz ZB, Frankau JM, Laroche CM, Fuld JP. Do Not Attempt Cardiopulmonary Resuscitation orders in acute medical settings: a qualitative study. QJM 2013;106(2):165-177. https://dx.doi.org/10.1093/qjmed/hcs222165-177 [ Links ]
12. Searight HR, Gafford J. Cultural diversity at the end of life: Issues and guidelines for family physicians. Am Fam Physician 2005;71(3):515-522. https://doi.org/10.4135/9781452204819.n6 [ Links ]
13. Onwuegbuzie AL, Leech NL. Sampling designs in qualitative research: Making the sampling process more public. Qual Rep 2007;12(2):238-254. [ Links ]
14. Dowling M. From Husserl to van Manen. A review of different phenomenological approaches. Int J Nurs Stud 2007;44:131-142. https://dx.doi.org/10.1016/j.ijnurstu.2005.11.026 [ Links ]
15. Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Educ Inform 2004;22(2):63-75. https://doi.org/10.3233/efi-2004-22201 [ Links ]
16. Shoorideh FA, Ashktorab T, Yaghmaei F, Alavi Majd H. Relationship between ICU nurses' moral distress with burnout and anticipated turnover. Nurs Ethics 2015;22(1):64-76. https://dx.doi.org/10.1177/0969733014534874 [ Links ]
17. Browning AM.CNE article: Moral distress and psychological empowerment in critical care nurses caring for adults at end of life. Am J Crit Care 2013,22(2):143-151. https://dx.doi.org/10.4037/ajcc2013437 [ Links ]
18. Park YR, Kim JA, Kim K. Changes in how ICU nurses perceive the DNR decision and their nursing activity after implementing it. Nurs Ethics 2011;18(6):802-813. https://dx.doi.org/10.1177/0969733011410093 [ Links ]
19. Fritz Z, Fuld J. Ethical issues surrounding do not attempt resuscitation orders: Decisions, discussions and deleterious effects. J Med Ethics 2010;36(10):593-597. https://dx.doi.org/10.1136/jme.2010.035725 [ Links ]
20. Brinkman-Stoppelenburg A, Rietjens JAC, van der Heide A. The effects of advance care planning on end-of-life care: A systematic review. J Palliat Med 2014;28(8):1000-1025. https://dx.doi.org/10.1177/0269216314526272 [ Links ]
21. Pettersson M, Hedstrom M, Hoglund AT. Striving for good nursing care: Nurses' experiences of do not resuscitate orders within oncology and hematology care. Nurs Ethics 2014;21(8):902-915. https://dx.doi.org/10.1177/0969733014533238 [ Links ]
22. Ferrand E, Lemaire F, Regnier B, et al. Discrepancies between perceptions by physicians and nursing staff of intensive care unit end-of-life decisions. Am J Respir Crit Care 2003;167(10):1310-1315. https://dx.doi.org/10.1164/rccm.200207-752OC [ Links ]
23. Martin B, Koesel N. Nurses' role in clarifying goals in the intensive care unit. Crit Care Nurses 2010;30(3):63-72. https://dx.doi.org/10.4037/ccn2010511 [ Links ]
24. Vermoch K, Anason B. Understanding global end-of-life care practices: IHF 2014 research project. World Hosp Health Serv 2015;51(4):4-10. [ Links ]
25. Espinosa L, Young A, Symes L, Haile B, Walsh T. ICU nurses' experiences in providing terminal care. Crit Care Nurs Q 2010;33(3):273-281. https://dx.doi.org/10.1097/CNQ.0b013e3181d91424 [ Links ]
 Correspondence:
Correspondence:
P Brysiewicz
brysiewiczp@ukzn.ac.za