Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
Southern African Journal of Critical Care (Online)
On-line version ISSN 2078-676X
Print version ISSN 1562-8264
South. Afr. j. crit. care (Online) vol.33 n.1 Pretoria Jul. 2017
http://dx.doi.org/10.7196/SAJCC.2017.v33i1.279
ARTICLE
Obstetric patients admitted to the intensive care unit of Dr George Mukhari Academic Hospital, Ga-Rankuwa, South Africa
M Motiang
MB ChB, MMed (Anaesth); Department of Intensive Care, Sefako Makgatho Health Science University, Pretoria, South Africa
ABSTRACT
BACKGROUND. Pregnancy is a natural physiological process that normally ends uneventfully. However, there are instances where admission to an intensive care (ICU) is required.
OBJECTIVES. To determine the spectrum of disease requiring ICU admission in obstetric patients, condition on discharge, maternal mortality, and the cause of maternal death.
METHODS. A retrospective study of all pregnant and postpartum patients admitted from January 2008 to December 2011 was conducted. Outcome measures were the spectrum of disease, ICU interventions, and maternal outcomes.
RESULTS. In total, 210 patients were reviewed. The mean age was 28.15 (standard deviation (SD) 6.97) years. Twelve (5.7%) patients were admitted at a mean (SD) gestational age of 25.33 (6.56) weeks, 94.2% (n=198) were postpartum, and 88.6% (n=186) were post-caesarean section. Pre-existing cardiac disease (44.3%, n=93), eclampsia and preeclampsia (20%, n=42), obstetric haemorrhage (16.2%, n=34), and pulmonary oedema (6.2%, n=13) were the most common causes of admission. Sixty-one percent (n=128) of patients received ventilatory support. The median length of ICU stay was 24 hours (range 1 - 17 days). Eighty-seven percent (n=183) of the patients were haemodynamically stable. Maternal mortality was 9% (n=19).
CONCLUSION. Cardiac disease in pregnancy was the most common diagnosis in patients admitted to our ICU, followed by eclampsia and preeclampsia. Most of the patients (87.1%) were haemodynamically stable and needed minimal intervention, as confirmed by their short periods of stay in ICU. Although the mortality rate in our institution was higher than that observed in developed countries, it was lower than rates reported in other South African studies. This study has found that many of the patients were admitted to ICU for monitoring purposes only and did not require ICU level of care.
Pregnancy represents a unique alteration in physiology that usually proceeds to its completion without complication. However, there are instances where complications, sometimes life-threatening, can occur that require intensive care with invasive monitoring and mechanical ventilation.[1]
Critically ill obstetric patients are significantly different from the average patient admitted to the intensive care unit (ICU). They present a challenge to the critical-care physician, owing to their unique physiology and the specific medical disorders that sometimes occur during pregnancy and the peripartum period.[2] The challenges faced in the treatment of these patients are even greater owing to the fact that two lives are simultaneously endangered.
Pregnant patients account for a small number of ICU admissions in developed countries (<2%) but they can reach up to 10% or more in developing countries.[3] Studies conducted in South Africa (SA) indicate admission rates of 6.7 - 13.6%.[4,5] The most common causes of admission to ICU for obstetric patients are eclampsia, severe pre-eclampsia, haemorrhage, anaesthetic complications, congenital and valvular heart disease, cardiomyopathy, and puerperal infections.[4-8] The overall maternal mortality rate in ICU varies from 0 - 38%. Local studies have reported a mortality rate in the range of 21 - 38%.[4-6]
In view of the aforementioned, a retrospective study was undertaken at Dr George Mukhari Academic Hospital (DGMAH), Ga-Rankuwa, SA. DGMAH is a tertiary hospital that receives 32% of obstetric referrals from neighbouring provinces. The aim was to determine the spectrum of diseases requiring ICU admission in obstetric patients, condition on discharge, maternal mortality, and the cause of maternal death.
Methods
The study was conducted at DGMAH, a 22-bed multidisciplinary ICU academic centre in Ga-Rankuwa, SA. The hospital is affiliated to Sefako Makgatho Health Sciences University. The ICU beds at DGMAH serve all surgical disciplines, internal medicine, obstetrics and gynaecology, as well as the paediatrics wards. An average of 720 patients are admitted to this ICU per annum; obstetrics patients represent 11.6% of all ICU admissions, which accounts for 0.92% of all deliveries. Thirty-two percent of obstetrics patients are referrals from nearby provinces like North West, Limpopo and Mpumalanga. A retrospective study of all pregnant and postpartum patients admitted to this multidisciplinary ICU over a 4-year period, from 1 January 2008 to 31 December 2011, was conducted. The study was approved by the Medunsa Research and Ethics Committee (MREC) of the university (ref. no. MREC/ M/31/2013:IR). Data were collected from the acuity book, which is used to record all daily admissions to ICU. Further data were extracted from the standard ICU flow chart, TPH254 (81/524737), as well as from the medical records section of the hospital. The data included basic demographic data, obstetric and medical history (weeks of gestation, mode of delivery, pre-existing medical conditions), diagnosis, length of stay in the ICU, length of stay on mechanical ventilation, haemodynamic stability, ICU outcome, condition on discharge, and cause of death. The reasons for ICU admission were sorted in descending order according to the frequency of occurrence. For each reason, a 95% confidence interval (CI) was calculated for the percentage of occurrence. Data analysis was performed usig Statistical Analysis System release 9.2 (SAS Institute Inc., USA).
Results
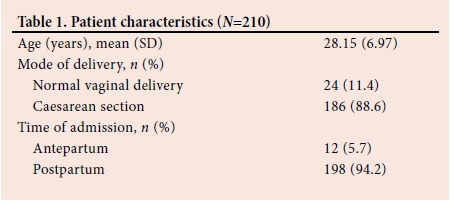
A total of 248 obstetric patients were admitted during the study period, of whom 210 had complete medical records. Fifteen percent (n=38) of the patients were excluded from the study due to incomplete records. The demographic characteristics of the participants are shown in Table 1. The mean age was 28.15 (standard deviation (SD) 6.97) years. Twelve (5.7%) patients were admitted at a mean (SD) gestational age of 25.33 (6.56), 94.2% (n=198) were postpartum, and 88.6% (n=186) were post-caesarean section.
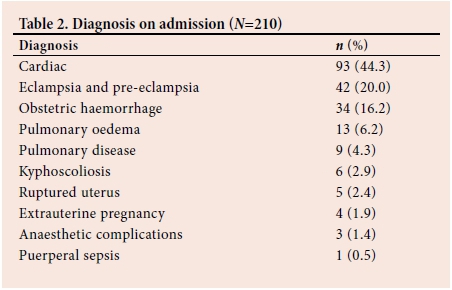
Pre-existing cardiac disease 44.3% (n=93/210), eclampsia-preeclampsia 20% (n=42), obstetric haemorrhage 16.2% (n=34) and pulmonary oedema 6.2% (n=13) were the most common causes of admission. Of the 93 patients who had pre-existing cardiac disease, mixed mitral valve disease accounted for 52% (n=48). The remaining 13.3% (n=28) of patients were admitted because of extrauterine pregnancy, a ruptured uterus, puerperal sepsis, pulmonary disease, anaesthetic complications, and kyphoscoliosis (Table 2).
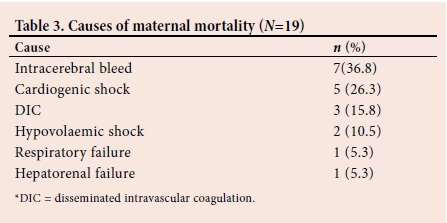
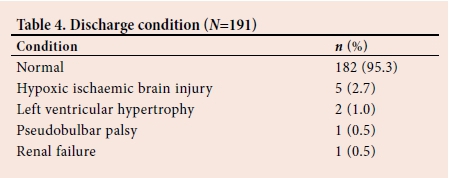
Eighteen (8.6%) women had an associated medical illness, other than cardiac, prior to pregnancy, with HIV infection being the most common (7.1%; n=15), followed by epilepsy. Sixty-one percent (n=128) of patients received ventilatory support, for a median (range) period of 1 (1 - 13) day. The median length of ICU stay was 24 hours (range 1 - 17 days). Eighty-seven percent (n=183) of the patients were haemodynamically stable. Maternal mortality was 9% (n=19). The major cause of death was intracerebral haemorrhage (36.8%; n=7), followed by cardiogenic shock (26.3%; n=5) (Table 3). A total of 191 (90.6%) patients were discharged, of whom 182 (95.3%) were in a stable condition. Five patients suffered hypoxic ischaemic brain injury, two had left ventricular hypertrophy, one developed pseudobulbar palsy, and the other suffered renal failure. Hypoxia developed as a result of difficult intubation in the operating room (n=2) and convulsions in eclampsia (n=3). Hypoxic ischaemic brain injury had been confirmed by computed tomography scans. All five patients were discharged with a tracheostomy mask. The patient who developed renal failure had to be dialysed (Table 4).
Discussion
Cardiac disease in pregnancy was the most common reason for admission in our patients, with mixed mitral disease as the predominant lesion, followed by peripartum cardiomyopathy. This is in agreement with the findings of Trikha and Singh.[8] In a study conducted in Belgium, it was found that pre-existing and acquired cardiopathies are the main reason for admission to an ICU in a developed country, and have surpassed hypertensive disorders and haemorrhage.[9] The second most common reason for admission was eclampsia and preeclampsia (20.0%), followed by obstetric haemorrhage (16.2%).
Afessa et al.[10] investigated the clinical course and outcome of critically ill obstetric patients treated in an ICU. They reported that obstetric patients with pre-existing medical problems were more likely to require intensive care support than those without pre-existing medical conditions. We had 48.6% patients with cardiac and pulmonary problems requiring ICU support.
A study undertaken at Tygerberg Hospital, Cape Town, SA, demonstrated a significant reduction in maternal deaths when patients were managed in an obstetric critical care unit.[11] Tygerberg Hospital is one of only two hospitals in SA that have a dedicated obstetric ICU in the public health sector. The first unit was opened at Groote Schuur Hospital in Cape Town, SA, with reported benefits in terms of continuity of care provided before and after delivery, as well as intensive observation that allowed for prevention or early recognition and treatment of complications.[12]
Our study had 198 (94.3%) patients admitted postpartum, 88.6%
of them post caesarean section. In a 5-year review of obstetrics patients requiring critical care, 66% of the women admitted were postpartum. This is likely related to the significant haemodynamic changes which occur in the postpartum period, including 65% increase in cardiac output, acute blood loss at delivery and a decrease in plasma protein oncotic pressure, which may exacerbate symptoms in patients with underlying cardiovascular or pulmonary dysfunction.[13] One hundred and eighty-three (87.1%) of our patients were, however, haemodynamically stable. Most of the patients were referred to ICU owing to a high risk for cardiovascular compromise due to pre-existing cardiac lesions.
Kilpatrick et al.[13] reported on a relatively small number of obstetric patients that required ICU admission. Pre-eclampsia was the single most common precipitating factor, accounting for 33% of obstetric diagnoses. They concluded that if expertise with insertion and monitoring of central venous and arterial lines were available in the labour and delivery units, relatively few women would require transfer to the ICU.[13] Pre-eclampsia and eclampsia accounted for 20% of admissions in our study.
In a study by Karnad et al.,[14] obstetric disorders accounted for 80% of their ICU admissions. Pulmonary oedema owing to valvular heart disease was one of the most common medical disorders. In our study, 6.2% of the patients with pre-eclampsia also had pulmonary oedema. Karnad et al.[14] reported a mortality rate of 21.6%, attributed to inadequate utilisation of prenatal services as well as a delay of more than 24 hours between the onset of acute illness and ICU admission.
In this study, 61% (n=128) of patients received ventilatory support for a maximum of 13 days and a median of 1 day. Other studies have reported ventilatory support of their patients in the range of 18.6% to 67%.[1,3,10,15-18]
The median length of ICU stay in this study was 24 hours, up to a maximum of 17 days. The patient who was hospitalised for 17 days was eventually discharged with a tracheostomy mask. She had suffered hypoxic brain injury following an eclamptic convulsion.
Between 2011 and 2013, the five most common causes of maternal deaths in SA were non-pregnancy-related infections (mainly HIV infection), obstetric haemorrhage, complications of hypertension in pregnancy, medical and surgical disorders, and pregnancy-related sepsis. There has been a 25% reduction in deaths due to HIV infections, most likely due to an efficient screening and treatment programme.[19] A study by Chweneyagae et al [7] found HIV infection to be the most important condition contributing to maternal death in SA.
Our maternal mortality was 9% over a period of 4 years. Seven (36.8%) patients died due to an intracerebral bleed in eclampsia. This may indicate failure to lower the blood pressure timeously and judiciously, as well as a lack of obstetric emergency training skills. Pre-eclampsia-eclampsia also accounted for the highest number of deaths in a study conducted in a tertiary hospital in the Limpopo Province, SA.[4] In order to reduce maternal mortality, Moran et al.[20] concluded that interventions to scale up emergency obstetrics skills training must happen alongside interventions to strengthen other components of the health system. This involves training healthcare workers in essential steps in the management of obstetric emergencies (ESMOE), team training using emergency obstetric simulation training (ESOT) and having appropriate policies and standard operating procedures in place.
Ntuli et al.[4] reported a mortality rate of 34.8%, which was higher than the mortality rate observed in our study, and that reported at King Edward VIII Hospital in Durban, SA,[5] but similar to the findings at Johannesburg Hospital, SA.[6] They[4] attributed this to lack of proper antenatal care, limited specialist obstetric and critical care specialist support, and poor transport.
Our mortality rate was low compared with other SA studies,[4-6] but relatively high when compared with developed countries. Australia reported a 0% mortality over a period of 8 years.[21]
Conclusion
Cardiac disease in pregnancy was the most common diagnosis in patients admitted to our ICU, followed by eclampsia and preeclampsia. Most of the patients (87.1%) were haemodynamically stable and needed minimal intervention, as confirmed by their short periods of stay in ICU.
Even though the mortality rate in our institution was higher than that observed in developed countries, it was lower than rates reported in other SA studies. This study has found that many of the patients were admitted to ICU for monitoring purposes only and did not require ICU level of care, whereas other SA units admitted patients with higher acuity of illness.
It is therefore recommended that proper screening of ICU referrals be conducted before admission, with a view to sparing ICU beds for the most deserving patients. Healthcare workers involved in obstetrics should also undergo training in ESMOE.
Acknowledgements. The author would like to thank Prof. HS Schoeman for statistical analysis and Prof. CT Sehoole for review of different drafts of this article.
Author contributions. MM conceptualised the study and wrote the manuscript.
Funding. None.
Conflict of interest. None.
References
1. Collop NA, Sahn SA. Critical illness in pregnancy. An analysis of 20 patients admitted to a medical intensive care unit. Chest 1993;103(5):1548-1552. https://doi.org/10.1378/chest.103.5.1548 [ Links ]
2. Soubra SH, Guntupalli KK. Critical illness in pregnancy: An overview. Crit Care Med 2005;33(10):S248-S255. https://doi.org/10.1097/01.ccm.0000183159.31378.6a [ Links ]
3. Vasquez DN, Estenssoro E, Canales HS, et al. Clinical characteristics and outcomes of obstetric patients requiring ICU admission. Chest 2007;131:718-724. https://doi.org/10.1378/chest.06-2388 [ Links ]
4. Ntuli TS, Ogunbanjo G, Nesengani S, Maboya E, Gibango M. Obstetric intensive care admissions at a tertiary hospital in Limpopo Province, South Africa. S Afr J Crit Care 2015;31(1):8-10. https://doi.org/10.7196/SAJCC.164 [ Links ]
5. Platteau P, Engelhardt T, Moodley J, Muckart JJ. Obstetric and gynaecological patients in an intensive care unit: A 1 year review. Trop Doctor 1997;27(4):202-206. https://doi.org/10.1177/004947559702700406 [ Links ]
6. Taylor R, Richards GA. Critically ill obstetric and gynaecological patients in the intensive care unit. S Afr Med J 2000;90(11):1140-1144. [ Links ]
7. Chweneyagae D, Delis-Jarrosay N, Farina Z, et al. The impact of HIV infection on maternal deaths in South Africa. S Afr J Obstet Gynaecol 2012;18(3):70-76. https://doi.org/10.7196/sajog.581 [ Links ]
8. Trikha A, Singh PM. The critically ill obstetric patient - recent concepts. Indian J Anaesth 201;54(5):421-427. https://doi.org/10.4103/0019-5049.71041 [ Links ]
9. De Greve M, Van Mieghem T, Van Den Berghe G, Hanssens M. Obstetric admissions to the intensive care unit in a tertiary hospital. Gynecol Obstet Invest 2016;81(14):315-320. https://doi.org/10.1159/000431224 [ Links ]
10. Afessa B, Green B, Delke I, Koch K. Systemic inflammatory response syndrome, organ failure, and outcome in critically ill obstetric patients treated in an ICU. Chest 2001;120(4):1271-1277. https://doi.org/10.1378/chest.120.4.1271 [ Links ]
11. Langenegger E. The impact of a new South African obstetric critical care unit at Tygerberg Hospital: A comparison of patient outcomes before and after. Int J Gynecol Obstet 2012;119(Suppl 3):S396-S397. https://doi.org/10.1016/s0020-7292(12)60814-5 [ Links ]
12. Johanson R, Anthony J. Obstetric intensive care at Groote Schuur Hospital, Cape Town. J Obstet and Gynaecol 1995;15(3):174. https://doi.org/10.3109/01443619509015490 [ Links ]
13. Kilpatrick SJ, Matthay MA. Obstetric patients requiring critical care; a five year review. Chest 1992; 101(5):1407-1412. https://doi.org/10.1378/chest.10L5.1407 [ Links ]
14. Karnad DP, Lapsia V, Krishnan A, Salvi VS. Prognostic factors in obstetric patients admitted to an Indian intensive care unit. Crit Care Med 2004;32(6):1294-1299. https://doi.org/10.1097/01.ccm.0000128549.72276.00 [ Links ]
15. Zwart JJ, Dupuis JRO, Richters A, Ory F, van Roosmalen J. Obstetric intensive care unit admission: A 2-year nationwide population-based cohort study. Intensive Care Med 2001;36(2):256-263. https://doi.org/10.1007/s00134-009-1707-x [ Links ]
16. Leung NYW, Lau AC, Chan KK, Yan WW Clinical characteristics and outcomes of obstetric patients admitted to intensive care unit: A 10-year retrospective review. Hong Kong Med J 2010;16(1):18-25. [ Links ]
17. Lataifeh I, Amarin Z, Zayed F, Al-Mehaisen L, Alchalab H, Khader Y. Indications and outcome for obstetric patients' admission to intensive care unit: A 7-year review. J Obstet Gynaecol 2010;30(4):378-382. http://dx.doi.org/10.3109/01443611003646298 [ Links ]
18. Gupta S, Naithani U, Doshi V, Bhargava V, Vijay BS. Obstetric critical care: A prospective analysis of clinical characteristics, predictability, and fetomaternal outcome in a new dedicated obstetric intensive care unit. Indian J Anaesth 2011;55(2):146-153. http://dx.doi.org/10.4103/0019-5049.79895 [ Links ]
19. National Committee for Confidential Enquiry into Maternal Deaths. Saving Mothers 2011-2013: Sixth report on the confidential enquiries into maternal deaths in South Africa - short report. http://www.doh.gov.za (accessed 29 November 2016). [ Links ]
20. Moran NF, Naidoo M, Moodley J. Reducing maternal mortality on a countrywide scale: The role of emergency obstetric training. Best Pract Res Clin Obstet Gynaecol 2015;29(8):1102-1118. [https://dx.doi.org/10.1016/j.bpobgyn.2015.08.002] [ Links ]
21. Siram S, Robertson MS. Critically ill obstetric patients in Australia: A retrospective audit of 8 years' experience in a tertiary intensive care unit. Crit Care Resusc 2008;10(2):120-124. [ Links ]
 Correspondence:
Correspondence:
M Motiang
mammie@telkomsa.net














