Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
Southern African Journal of Critical Care (Online)
versión On-line ISSN 2078-676X
versión impresa ISSN 1562-8264
South. Afr. j. crit. care (Online) vol.30 no.2 Pretoria nov. 2014
http://dx.doi.org/10.7196/SAJCC.219
ABSTRACTS
Scientific presentations to the Congress of the Critical Care Society of Southern Africa 2014
26 - 30 November 2014
Baxter Theatre Centre, Cape Town, South Africa
The nature of involvement of physiotherapists in South Africa in the weaning of mechanically ventilated patients
D Morar,* H van Aswegen
Department of Physiotherapy, School of Therapeutic Sciences, University of the Witwatersrand, Johannesburg, South Africa *dm.physio4you@gmail.com
Background. An important goal of patient management in intensive care units (ICUs) is successful weaning of patients from mechanical ventilation (MV). Research has focused on the involvement of allied health professionals in weaning of patients from MV.
Objective. To determine the involvement of physiotherapists in South Africa (SA) in the development and implementation of weaning protocols in ICUs, and in extubation, and what modalities are used to facilitate respiratory muscle strengthening.
Methods. Physiotherapists who work in adult ICUs in SA were asked to complete a survey questionnaire. This was available on SurveyMonkey or posted at the request of some participants.
Results. A total of 425 questionnaires were distributed. Response rate was 43.3% (n=184). The majority of physiotherapists (76%) were not or seldom involved in weaning of mechanically ventilated patients in ICU. Physiotherapists were somewhat involved in extubation (16%). Physiotherapy modalities used to facilitate respiratory muscle strengthening included exercises (81%), early mobilisation out of bed (77%) and deep-breathing exercises (77%).
Conclusion. Most SA physiotherapists are not involved in weaning of patients from MV. There is a need to reconsider their role in ICUs as current practice is not in keeping with international reports.
The effect of two passive head-down diaphragm stretching manoeuvers on diaphragm length in healthy adult individuals
J Schewitz,1* R Roos,1 H Van Aswegen,1 S Manda2
1 Department of Physiotherapy, School of Therapeutic Sciences, University of the Witwatersrand, Johannesburg, South Africa;
2 Biostatistics Unit, Medical Research Council, Pretoria, South Africa *jax@schewitz.com
Background. Stretching of skeletal muscles is a physiotherapy treatment modality. Head-down tilt positions are used in cardio-pulmonary physiotherapy to facilitate sputum drainage. A head-down tilt position could potentially influence diaphragm length if applied for a sustained period of time due to likely abdominal content displacement from a caudal to a cranial position.
Objective. To determine if diaphragm length could be influenced by a head-down tilt position and if this change in length alters diaphragm function.
Methods. A quasi-experimental study was conducted in 2012 with 75 undergraduate physiotherapy students, who were consecutively sampled according to specific inclusion criteria. The experimental procedure comprised four different head-down tilt positions: 15° for 30 s, 15° for 2 min, 30° for 30 s and 30° for 2 min. Diaphragm length change was assessed with M-Mode ultrasound, and diaphragm function was recorded in terms of peak expiratory flow rate (PEFR) and thoracic expansion (TE). Dyspnoea was recorded for subjective view of participants' tolerance of the positions and vital signs for objective tolerance. Data were analysed using descriptive statistics and analysis of variance (ANOVA), a Kruskal-Wallis test and a Student's t-test.
Results. The cohort comprised 61 (80.5%) women and 14 (19.5%) men with a mean age of 20.9 (standard deviation (SD) 2.5) years and a mean body mass index of 23.1 (3.8) kg/m2. At rest, the mean TE (2.5 (0.7) cm) was less than normal and mean PEFR (423.8 (95.2) L/min) was less than the predicted PEFR (446 (95.16) L/min). The greatest change in length of diaphragm from baseline occurred at a head-down tilt position of 30° for 2 min for the left hemidiaphragm and a head-down tilt position of 30° for 30 s for the right hemidiaphragm. These changes were significant (p=0.00) for both the right and left sides. No significant change in diaphragm function occurred from baseline during the different head-down tilt positions as reflected by change in TE (p=0.54) and PEFR (p=0.98). Participants tolerated the different head-down tilt positions as no significant change in vital signs or dyspnoea occurred from baseline.
Conclusion. A change in diaphragm length is possible by applying a stretch to the muscle in a head-down tilt position, and could be incorporated in cardiopulmonary physiotherapy practice. Diaphragm function did not show an improvement when measured by PEFR and TE. Future research could investigate if a stretch to a shortened diaphragm, such as in a patient with chronic obstructive pulmonary disease, would lengthen the muscle and thereby change respiratory function.
The feasibility of an early mobilisation programme using the Physical Function in Intensive Care Unit Test tool in Zimbabwe: Prospective cohort study
C Tadyanemhandu,1* S Manie2
1 Department of Rehabilitation, College of Health Sciences, University of Zimbabwe, Harare, Zimbabwe;
2 Department of Health and Rehabilitation Sciences, Faculty of Health Sciences, University of Cape Town, South Africa *cathytadya@gmail.com
Background. Physiotherapy has been reported to be an integral part in the management of intensive care unit (ICU) patients, and research has proven that physiotherapy has a great impact on ventilatory dependency and length of stay in the ICU. The Physical Function in ICU Test (PFIT) tool has been proven to be a responsive and reliable outcome measure in ICU patients in Zimbabwe.
Objective. To determine the feasibility of an early mobilisation programme using the PFIT tool in a developing country.
Methods. A prospective cohort study was carried out at a teaching hospital ICU in Harare, Zimbabwe. Patients were recruited from the mixed adult medical-surgical ICU from November 2012 to February 2013. All patients provided written informed consent or had their next of kin consent on their behalf to participate in the study. The sample size was calculated using the pre- and postPFIT scores before and after weaning from a mechanical ventilator from the research done by Skinner et al. (2009); the expected sample size was 37. Inclusion criteria included all patients who were admitted to the ICU and high-dependency unit irrespective of ventilation method (non-invasive or invasive), aged 18 years or older, who were medically stable. The data recorded on the questionnaire included: demographics data including age, gender and diagnosis; clinical outcomes including method of ventilation, ventilator settings, duration of mechanical ventilation and length of stay in the unit; and PFIT results and vital signs measured pre and post treatment. The vital signs recorded included heart rate, blood pressure, mean arterial pressure, saturation of oxygen and respiratory rate. The modified version of the PFIT (which has the following components: sit to stand, marching on the spot, shoulder and knee muscle strength testing) was used to prescribe exercises as well as an outcome measure of functional capacity at discharge.
Results. A total of 35 patients was recruited over a period of 3 months, of which 20 (57.1%) were males, median age 29 years. The tool was implemented in 32 patients on the initial PFIT measurement. Of these, 16 (45.7%) required the assistance of two people to stand, and only 13 (37.1%) marched on the day. The initial PFIT mean score was 5.3 (standard deviation 1.8) with a minimum score of 2.0 and a maximum of 8.8. On final PFIT measurement, of the 30 patients seen, 15 (42,9) did not require any assistance to stand and 24 (68.6%) marched on the spot. The final PFIT mean score was 7.0 (1.9), with a minimum score of 3.2 and maximum of 8.8 recorded. There was a significant difference in both the initial PFIT total score (t-value=2.34, df=30, p=0.03) and the final PFIT score (t-value=3.66, df=28, p=0.001) between males and females. The most frequent barriers to exercise were sedation and cardiovascular instability. No adverse events were recorded.
Conclusion. This study showed that an early mobilisation programme using PFIT was feasible and safe in the Zimbabwe setting, as no adverse events occurred during this phase. A change in PFIT score was noted, in comparing the initial and final scores, and there was also a difference in functional capability between males and females, with males more likely to participate in functional activities.
An audit of transfers into the paediatric intensive care unit at the Red Cross War Memorial Children's Hospital: Ten years later
K Dimitriades,* B M Morrow, A C Argent
Paediatric Intensive Care Unit, Red Cross War Memorial Children's Hospital; and School of Child and Adolescent Health, University of Cape Town, South Africa *kdimitriades@gmail.com
Background. Children are transferred from various facilities into paediatric intensive care units (PICUs) for critical care, without a specialised paediatric transfer service. A previous audit in 2003 reported a high incidence of technical, clinical and critical adverse events during transfers.
Objective. To conduct a follow-up audit on interfacility transfers into PICUs, to determine practice and outcome changes.
Methods. Prospective observational study of all patients transferred into the PICU between 1 December 2013 and 30 November 2014. Ethical approval was obtained (HREC 702/13).
Results. Interim analysis at 6 months was performed on 104 transfers (median age 1.7 (interquartile range 0.3 - 10.5) months) and compared with results reported by Hatherill et al. (2003). There was a decrease in the proportion of medical transfers (from 49% to 36.5%; p=0.04) and referrals from metropolitan hospitals (from 34.7% to 18.3%; p=0.003), while referrals from academic hospitals increased from 35.1% to 50% (p=0.01). Staff categories accompanying transfers and transfer times were unchanged. The proportion of fixed-wing transfers increased from 14.4% to 24% (p=0.035), with helicopter use decreasing from 9.9% to 0% (p<0.0001). A total of 58.4% of patients were intubated for transfer in 2003 compared with 70.2% in 2014 (p=0.04). The rate of total technical (35.6 - 45.2%; p=0.1), clinical (26.7 - 26.9%; p=0.9), and critical (8.9 - 4.8%; p=0.3) adverse events remained unchanged. PICU mortality decreased from 16.8% to 8.6% (p=0.07), which may relate to improved PICU care.
Conclusion. The rate and staffing structure of interfacility transfers into PICUs have remained unchanged over a decade, and associated adverse event rates remain high. Research is needed to identify ways of improving PICU retrieval services.
Viruses in children with burns injury in the intensive care unit at the Red Cross War Memorial Children's Hospital
K Dimitriades,1 B M Morrow,1 D Hardie,2 A C Argent1
1 Paediatric Intensive Care Unit, Red Cross War Memorial Children's Hospital; and School of Child and Adolescent Health, University of Cape Town, South Africa;
2 National Health Laboratory Service and Department of Virology, Cape Town, South Africa *kdimitriades@gmail.com
Background. Children with burn injury are commonly admitted to the paediatric intensive care unit (PICU) at Red Cross War Memorial Children's Hospital, and during their admission, respiratory viruses are identified.
Objective. To investigate the role of viral infections in children with burn injury admitted to the PICU. Objectives include the prevalence of viruses, the timing of identification and the outcomes, including all-cause ICU mortality and duration of ICU stay.
Methods. A retrospective database search was performed using the PICU and laboratory database, reviewing a period of 55 months. The PICU database is approved by the University of Cape Town Human Research Ethics Committee (UCT HREC 039/11), which approved this study with waived consent (HREC703/2013).
Results. Two hundred admissions were recorded over the 55-month period in 174 children with burn injury. a prevalence of 24.1% was noted. A total of 27.9% of viruses were identified after 48 h of admission in the PICU. Children with viral infections were younger than those without (median age 18.7 months v. 33.3 months; p=0.0179) and had a longer admission (3 days v. 7 days; p=0.00001). The most commonly identified viruses included rhinovirus A, adenovirus and influenza A. A seasonal peak in burn injury and viral observations was noted over the winter months. No association was shown regarding viral identification, percentage burn and mortality.
Conclusion. Respiratory viruses are common in children admitted to the PICU with burn injury, and may affect the length of stay in the ICU. Further studies are required to examine the association between these viruses and sepsis in these children.
Medication errors in the intensive care unit: A South African perspective
D C Cruickshank,* L Brannigan
Specialised Intensive Care Unit, Life The Glynnwood Hospital, Johannesburg, South Africa *dc.cruickshanlk@lifehealthcare.co.za
Background. Critically ill patients receive almost twice as many medicines as hospital patients outside the intensive care unit (ICU), and nearly all will suffer a potentially life-threatening error at some time during their ICU stay. Literature review reveals that human factors, including stress, high workloads, knowledge deficits and performance deficits are associated with medication errors. Currently no data exist for the South African (SA) situation.
Objective. To quantify the rate of medication errors in our ICU and to see if they were comparable with those in the rest of the world.
Methods. Data were collected by a pharmacist in a 13-bed closed ICU that admits both medical and surgical patients. A total of 3 329 ICU charts were analysed from August 2013 to July 2014, and potential and actual medicine-related errors and interventions were recorded.
Results. A total of 416 (12.49%) medication-related errors took place during the period. Nursing-related errors included missed or incorrect doses; incorrect medication administered accounted for 176 (5.28%) ofthe errors.There were 240 physician-related medication errors, with dose errors 97 (2.91%) being the highest.
Conclusion. Indications are that medication errors in an SA ICU are comparable with those in other countries. Further research is required to determine the factors involved in order to develop strategies for preventing medication errors.
Alveolar proteinosis and severe nosocomial pneumonia managed with extra-corporeal membrane oxygenation to allow broncho-alveolar lavage and lung protective ventilation
L Brannigan,1* M Davidson2
1 Department of Anaesthesia and Department of Critical Care, University of the Witwatersrand; ICAN Critical Care and Anaesthesia Practice, Life The Glynnwood Hospital; Wits Donald Gordon Transplant Unit, Johannesburg, South Africa;
2 Department of Cardiothoracics, University of the Witwatersrand; Life The Glynnwood Hospital; and ARWYP Medical Centre, Johannesburg, South Africa *lliam@theicangroup.co.za
Pulmonary alveolar proteinosis is a rare condition, first described in 1958, which has autoimmune origins. A 55-year-old male patient was referred to Life The Glynnwood Hospital with biopsy-proven idiopathic pulmonary alveolar proteinosis. His condition was complicated by the fact that he developed a severe culture-positive pneumonia that made bronchoalveolar lavage at the referral institution impossible because of severe life-threatening hypoxaemia. His chest X-ray demonstrated bilateral diffuse alveolar infiltration with consolidation of the right middle lobe. He was hypoxic on fractional inspired oxygen (FiO2) of 80% and had poor lung compliance on the ventilator. He was referred because our institution has extracorporeal membrane oxygenation (ECMO) capabilities.The patient was deemed an appropriate candidate by the multidisciplinary team involved, using the South African ECMO guidelines. The patient was placed on veno-veno ECMO, which allowed for two consecutive large-volume bronchoalveolar lavage attempts, was ventilated using ultralung protective ventilation and was treated for his pneumonia on appropriate antibiotics. This case demonstrates that utilising a multidisciplinary team decision-making process for expensive technologies such as ECMO can result in the responsible, cost-effective and clinically effective utilisation of this technology.
The needs of family members accompanying patients into a trauma casualty
M Botes,* G Langley
Department of Nursing Education, University of the Witwatersrand, Johannesburg, South Africa *meghan.botes@wits.ac.za
Background. Families are not prepared for the traumatic injuries of loved ones. An emergency nurse has the important role of caring for patients and their families in this time of crisis. The needs of families in the critical care setting have been explored using the Critical Care Family Needs Inventory (CCFNI); however, little is known about the needs of families in the emergency department.
Objective. To determine the needs of family members accompanying injured patients into the emergency department, and to determine if these needs are met.
Methods. A quantitative, descriptive, contextual design study was conducted in a level 1 trauma facility at a public tertiary academic hospital in Johannesburg, South Africa. The population included family members of patients admitted to the emergency department, with a sample of 100 participants. A validated instrument based on the CCFNI was used. Five themes were explored, namely meaning, proximity, communication, comfort and support, and data were analysed using descriptive statistics. Open-ended questions were included and responses analysed using content analysis.
Results. Themes that ranked as highly important were meaning and communication, while satisfaction was highest within the theme meaning. A concerning finding was the low level of satisfaction with communication and prolonged time spent in casualty, which has a negative impact on the family's satisfaction with care. Discrimination based on nationality has become a growing concern.
Conclusion. There is a need for emergency nurses to include the care of families in their practice holistically. Needs expressed by families should inform the roles and responsibilities of emergency nurses.
Career aspirations of Baccalaureate nurses in South Africa
M B Randa,1* J D Mokoena,1 F M Tladi,2 M C Matlakala3
1 Department of Nursing Sciences, University of Limpopo (Medunsa), Pretoria, South Africa; 2 Department of Nursing Sciences, University of Limpopo (Turfloop campus), Polokwane, South Africa; 3 Department of Health Sciences, University of South Africa, Pretoria, South Africa *moreoagae@gmail.com
Background. Graduate nurse attrition continues to be a problem for healthcare delivery globally. Despite continuing training and education of student nurses, the shortage of nurses continues to be a threat to quality nursing service delivery.
Objective. To determine the career aspirations of graduate nurses in order for nursing programmes to support and nurture these graduates, which may in turn reduce attrition in the profession.
Methods. A qualitative research design was used to explore and describe the career aspirations of new Baccalaureate nurse graduates. Data were collected from self-reported narrative sketches.
Results. The study deduced that students' career aspirations included becoming nurse specialists within the profession, for example occupational health nursing, critical care nursing, midwifery and primary healthcare nursing, while others aspired to be in other professions outside the nursing profession, such as being a medical doctor, dentist, psychologist or pharmacist.
Conclusion. Career development should be an integral part of Baccalaureate student nurse education, and curriculum development should continually be informed by research data on nursing as a career, and the inherent challenges and threats.
Investigation of biofilm formation on a charged intravenous catheter relative to that on a similar but uncharged catheter
G A Richards,1,2* A J Brink,3 R McIntosh,4 H C Steel,5,6 R Cockeran5,6
1 Department of Critical Care, University of the Witwatersrand, Johannesburg, South Africa;
2 Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa;
3 Department of Clinical Microbiology, Ampath Lababoratories, Johannesburg, South Africa;
4 School of Physics, University of the Witwatersrand, Johannesburg, South Africa;
5 Medical Research Council, Inflammation and Immunity Unit, Department of Immunology, University of Pretoria, South Africa;
6 National Health Laboratory Service, Pretoria, South Africa. *guy.richards@wits.ac.za
Background. Catheter-related blood stream infections increase morbidity, mortality and costs. As such, any reduction in the rate of sepsis would be significant.
Objective. To investigate if Certofix protect catheters carry a surface charge and if this inhibits biofilm formation.
Methods. Capacitance of catheter surfaces was measured to determine if they released ions. Distilled water was passed through the catheter, and current measured as a function of voltage. Standard and charged catheters were also exposed to PBS as controls or 2 χ 106 colony-forming units/mL of six different micro-organisms for 60 or 120 min.
Results. With probes touching the inner and outer surfaces, capacitance was not voltage dependent, indicating surfaces were uncharged or carried a similar charge. When one probe penetrated the catheter wall, capacitance was weakly voltage dependent, indicating a surface charge. When the growth of detached bacteria was measured, biofilm formation was significantly reduced (p<0.05) for charged catheters for all organisms.
Conclusion. Certofix protect catheters carry a charge and this charge inhibits biofilm formation.
Knowledge, attitudes and practices regarding intensive care-trained nurses on evidence-based practice in an academic hospital in Gauteng
S Schmollgruber,* W M Kumwenda
Department of Nursing Education, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa *shelley.schmollgruber@wits.ac.za
Objective. To describe the knowledge, attitudes and practices of intensive care-trained nurses on evidence-based practice (EBP) in an academic hospital in Gauteng.
Methods. In this mixed-methods, sequential explanatory study, data were collected from intensive care unit (ICU)-trained nurses (n=100), who were purposively selected using a validated tool (Upton and Upton, 2006), to obtain quantitative results on their knowledge, attitudes and practices on EBP. This phase was followed by a focus group discussion with 12 expert ICU-trained nurses to explore the quantitative results in more depth. The quantitative and qualitative findings were combined at discussion of results.
Results. From the quantitative results, most nurses ranked 81% on knowledge towards EBP, 75% on attitudes towards EBP and 75% on practices toward EBP. The qualitative results identified three categories: perceptions, challenges and suggestions. The ICU-trained nurses were knowledgeable in their EBP understanding, but lacked knowledge in the skills of accessing evidence. Welcoming attitudes towards EBP were displayed, but ICU nurses admitted to their practices being only partially evidence based owing to challenges that included resistance to change, lack of resources, time and autonomy. The instrument was found to be reliable and valid, with a Cronbach's α of 0.94 for the entire questionnaire.
Conclusion. This study indicated that although ICU nurses were knowledgeable about EBP, they were still lacking in related skills. Therefore, we recommend capacity building of ICU-trained nurses as well as development of their EBP skills to support EBP.
Family satisfaction with care and decision making in the intensive care units
S Schmollgruber,* G Rodrigues, G Langley
Department of Nursing Education, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa *shelley.schmollgruber@wits.ac.za
Objective. To investigate families' satisfaction with care and decision-making in intensive care units (ICUs).
Methods. In this cross-sectional survey, South African families completed a modified FS-ICU 24 survey tool (Heyland et al., 2001). Data were collected on satisfaction with care and decision-making in ICUs.
Results. A total of 100 family members completed and returned the questionnaire. Satisfaction with care was rated by family members higher than satisfaction with decision-making. Overall, family members were mostly satisfied with the care provided (91%; n=91). Of the 24 items, management of patient symptoms was the most highly rated item. The least-rated item related to the waiting room, which 93% (n=93) rated as dissatisfactory. Frequency of communication, completeness of information, feeling excluded and unsupported during decision-making and rigid visiting hours were areas identified for improvement in the ICU.
Conclusion. The findings of the study suggest that deficiencies exist in the meeting of family members' needs, and are supported by existing literature on family satisfaction with care and decision-making in the ICU. Use of formal guidelines and education is recommended to increase family involvement and confidence in participating in decision-making. Educators, managers, senior nurses and other members of the multidisciplinary team should collaborate to encourage family members to become more involved in ICUs.
Strategies for the implementation of clinical practice guidelines in the intensive care unit: A systematic review
F Mpasa, P Jordan,* C Bowers
School of Clinical Care Sciences, Nelson Mandela Metropolitan University, Port Elizabeth, South Africa *portia.jordan@nmmu.ac.za
Background. Implementation strategies for the use of clinical practice guidelines (CPGs) are an integral component in bridging the gap between the best research evidence and clinical practice, especially in intensive care units (ICUs).
Objective. To conduct a systematic review of clinical practice guideline implementation strategies in ICUs.
Methods. Databases searched included CINAHL, Google Scholar, Academic Search Complete, Cochrane Register and MEDLINE via PubMed. The search identified 315 potentially relevant studies. After the process of critical appraisal, 10 randomised controlled trials were included in the systematic review. The Joanna Briggs Institute Critical Appraisal MASTARI Instrument for randomised controlled trials and data extraction tools were used to critically appraise and extract data from the 10 included randomised controlled trials.
Results. Various implementation strategies were identified, namely printed educational materials, information/educational sessions/ meetings, audit and feedback and champion/local opinion leaders, educational outreach visits, and computer or internet usage. The most frequently used strategies were collaboration/interdisciplinary teams, slide shows, teleconferences/videoconferences and discussions.
Conclusion. Various implementation strategies are available to promote the uptake of CPGs in the ICUs.
The relationship between organisational contextual factors and clinical practice guideline implementation in private critical care units
E Flippies,* P Jordan, D Venter
Nelson Mandela Metropolitan University, Port Elizabeth, South Africa *flippies86@gmail.com
Background. Organisational factors, e.g. culture, leadership and resources, should be considered when clinical practice guidelines (CPGs) are to be implemented in critical care units (CCUs).
Objective. To explore the relationship between organisational contextual factors, and CPG implementation in private CCUs.
Methods. In this positivistic, quantitative research study, the hypothesised relationship between organisational contextual factors and CPG implementation was investigated. A structured, pre-existing questionnaire, namely the Alberta Context Tool, was used to collect data from registered nurses in private critical care units. The Cronbach's coefficient alphas for the factors in the questionnaire proved to be reliable, as a score of >0.80 was obtained for all factors. Descriptive and inferential statistics were used to analyse the data.
Results. The demographic results indicated that most of the participants included in the research study were between 40 and 49 years (38%), while 47% of the participants had worked in ICUs for at least 10 years; 50% were permanently employed, 33% were in management positions and 13% were employed through a nursing agency. Except for the staffing, leadership and culture, a positive correlation was found between all the organisational factors and CPG implementation.
Conclusion. Organisational factors need to be explored when CPG implementation is considered in ICUs, as it can affect the effective uptake and utilisation of such CPGs.
Critical values for urgent clinician notification at South African intensive care units
E Schapkaitz,1 B Levy2
1 Department of Molecular Medicine and Haematology, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg South Africa;
2 ICAN Group, Johannesburg, South Africa
Background. Critical value policies are used by clinical laboratories to decide when to notify caregivers of life-threatening results. There remains, however, much debate and lack of consensus regarding the establishment of clinically relevant critical limits for intensive care units (ICUs).
Objective. To determine the critical value policies of ICU specialists for haematology tests in South Africa.
Method. An electronic survey was designed using SurveyMonkey, and distributed through the Critical Care Society of Southern Africa. Data collected included a biographical component, critical value policies and critical value reporting.
Results. There were 68 respondents from a range of specialist qualifications working in private practice (33.82%), government (39.71%) or both (26.47%). Of these, 76.47% had been in practice for >10 years. Median low and high adult critical limits for the most frequently listed tests were as follows: haemoglobin <7 g/dL and >20 g/dL, platelet count <50 χ 109/L and >1 000 χ 109/L, white cell count <2 χ 109/L and >20 χ 109/L, activated partial thromboplastin time >60 s and international normalised ratio >4. Specific critical limits for neonates were completed by 20 of the respondents. Of the respondents, 95.92% indicated that it was important to be contacted with first-time critical results, and 48.98% for repeat critical values. Preferences with respect to the person notified of the critical value were the physician who ordered the test (42.86%), the caregiver directly involved in the patient's care (24.49%) or the doctor on call (28.57%), by direct communication.
Conclusion. In addition to developing critical value policies in conjunction with laboratories, it is important that these are reviewed by local specialists to ensure that cut-offs are clinically relevant.
Intermittent positive pressure breathing is an effective technique to improve ventilation distribution in high-risk adults following open upper abdominal surgery
N Ross,* B Morrow, S Hanekom
Division of Physiotherapy, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa *nicoletteros@gmail.com
Background. Upper abdominal surgery (UAS) is associated with a high risk of postoperative pulmonary complications (POPC). The risk and severity of POPC can be reduced by the use of physio-therapeutic manoeuvres that increase lung volumes. Delivering intermittent positive pressure breathing (IPPB) via a mouthpiece is commonly practised for patients following UAS, with or without positive end expiratory pressure (PEEP) according to personal preference. Electrical impedance tomography (EIT) is a non-invasive tool for monitoring regional ventilation. The ability of EIT to accurately measure ventilation distribution has been validated in experimental and clinical studies using established techniques as the reference standards.
Objective. To describe differences in regional and global ventilation magnitude and distribution when administering IPPB with or without PEEP, compared with deep breathing exercises (DBExs) alone, in adult patients at high risk of POPC following UAS.
Methods. Ethical approval was obtained from relevant ethical committees. All adults who had open UAS at two hospitals in Cape Town, South Africa, between May 2013 and March 2014 were eligible for inclusion into this randomised, controlled, crossover trial. Seven patients were included in this study.
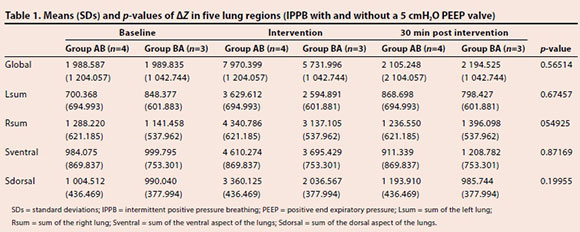
Results. When compared with baseline readings (1989) (95% confidence interval (CI) 328 - 3 650), a greater mean global lung impedance change (ΔΖ) was detected with IPPB (6 851) (95% CI 5 190 - 8 512; p=0.00015) compared with DBExs (4 047) (95% CI 2 047 - 6 047); p=0.055). There was no difference in ΔΖ when patients received IPPB with 5 cmH2O PEEP, compared with no PEEP (Table 1).
Conclusion. IPPB is an effective technique to improve lung volumes compared with DBExs. Further studies are required to investigate the effect of IPPB on clinical outcome.
Use of inhaled nitric oxide as rescue therapy in a patient with severe ARDS: A case report
A Goolam Mahomed,1* M I E Hassen,3 Z Asmal,3 F Tsela3
1 Department of Intensive Care, Medunsa Campus, University of Limpopo, Pretoria, South Africa;
2 Internal Medicine, Medi-Clinic Heart Hospital, Pretoria, South Africa;
3 Nephrology, Medi-Clinic Heart Hospital, Pretoria, South Africa *akhtergm@telkomsa.net
Inhaled nitric oxide (iNO) used as a pulmonary vasodilator works best in areas of the lung that are well ventilated, leading to improved oxygenation owing to improvements in ventilation/perfusion mismatch. However, randomised controlled studies have failed to show any survival benefit. We present a case report to highlight the use of iNO as rescue therapy in a patient with severe acute respiratory distress syndrome (ARDS). A patient with systemic lupus erythematosus and chronic renal failure, on regular dialysis, developed respiratory distress with dense bilateral consolidations, and remained hypoxic despite mechanical ventilation with 100% oxygen, hydrocortisone and prone positioning. iNO was then commenced via a side port on the ventilator circuit at a flow rate of 20 ppm. Within 1 h, the partial pressure of oxygen (PO2) had improved to 106 mmHg and remained high. The patient was then gradually weaned from a fractional inspiration of oxygen (FiO2) of 1.0 to 0.65 by the next morning, and further to 0.40 over the ensuing days. iNO was then gradually weaned off after 18 days of therapy. The patient was subsequently weaned off the ventilator and discharged from the intensive care unit. Although iNO is not recommended for routine use in severe ARDS, it should be considered as rescue therapy in patients who do not respond to conventional management.
A profile of current physiotherapy practices in intensive care in South Africa
F Karachi,1,2* S Hanekom,1 R Gosselink3
1 Department of Physiotherapy, Faculty of Health Sciences, Stellenbosch University, Cape Town, South Africa;
2 Department of Physiotherapy, University of the Western Cape, Cape Town, South Africa;
3 Student Affairs and Sports Policy, Katolieke Universiteit Leuven, Leuven, Belgium *fkarachi@uwc.ac.za
Background. Neither internationally nor locally has the profile, role and practices of intensive care physiotherapists been defined, but some evidence exists for the effectiveness of intensive care physiotherapy. No study has attempted to evaluate the profile, role and current practices of public sector intensive care unit (ICU) physiotherapists in South Africa (SA) particularly.
Objective. To conduct a survey of the current profile, role and practices of physiotherapists in public sector ICUs in SA.
Methods. An electronic survey on general data, qualifications, training, work experience, workload, patient load, referral system, patient management, utilisation of protocols, discharge procedure and follow-up was used to collect data. All physiotherapy heads and respective physiotherapists offering services to public sector ICUs in SA were included. Descriptive data are currently being analysed.
Results. Preliminary results show that the majority of physiotherapists working in intensive care have BSc degrees, minimal postgraduate ICU training, increased workload, are not exclusively allocated to a unit, use very few protocols, if any, and do not have a standardised referral, discharge and follow-up service.
Conclusion. Preliminary results concur with international findings that there is variation in practice of intensive care physiotherapists in SA. This may have an effect on patient outcome in intensive care. Final conclusions will be drawn once all data have been collected and analysed.