Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
Journal of the South African Veterinary Association
versão On-line ISSN 2224-9435
versão impressa ISSN 1019-9128
J. S. Afr. Vet. Assoc. vol.95 no.1 Pretoria 2024
http://dx.doi.org/10.36303/JSAVA.565
CASE REPORT
Impaired endochondral ossification in a skeletally immature dog: implications for femoral cleft formation and suspected incomplete femoral ossification
P GuyI; C Le RouxII
IPanorama Veterinary Clinic, South Africa
IIVet Imaging Specialists, South Africa
ABSTRACT
Historically, knowledge regarding congenital skeletal malformations in canines is poor. The Nomina Embryologica Veterinaria does not currently list any dysmorphia related to distal femoral fusion, and there is a significant absence of comprehensive descriptions of congenital defects in the veterinary literature. This paper reports on the radiographic and computed tomography (CT) characteristics of a skeletal abnormality in a seven-month-old crossbreed dog that presented for chronic right pelvic limb lameness as a result of secondary developmental patella luxation. Successful resolution of the lameness was achieved through concurrent surgical correction of the patella luxation and distal femoral cleft.
Keywords: patella luxation, femoral malformation, stifle, congenital, diagnostics, dog, imaging, skeletal
Introduction
Mammalian skeletal development encompasses a highly intricate and dynamic process characterised by the orchestrated interplay of various biological mechanisms. This process is governed by a sequence of events that includes vascular ingrowth, mineralisation, and ossification, collectively driving the growth and maturation of long bones and the development of apophyses (Moioli 2014). Ossification commences within a focal site, expanding until preexisting tissue is entirely replaced by bone. This origin is termed the primary ossification centre, signifying the initial locus of bone formation. The majority of primary ossification centres arise during the embryonic (days 19-35) and early foetal stages (days 35-birth), with a subset also emerging during the postnatal period. Notably, in certain bones, such as long bones, the primary ossification centre does not uniformly include the entirety of the precursor tissue zone. This insufficiency prompts the formation of secondary centres of ossification in regions where primary centres have not propagated. These secondary centres of ossification predominantly manifest postnatally. Following the appearance of secondary centres of ossification within the epiphyseal region of long bones, a process ensues whereby the centre undergoes multidirectional growth, culminating in the establishment of the epiphyseal growth plate (Zoetis et al. 2003). In the dog, some bones develop from a single centre of ossification, whilst others develop from two or more. Their appearance and fusion are well documented in scientific literature and occur at different times (Evans & de Lahunta 2013; Modina et al. 2019; Zoetis et al. 2003). The femur's ossification involves five centres: four proximal (diaphysis/shaft, proximal epiphysis/head, major trochanter, minor trochanter) and a combined unit for lateral and medial condyles in the distal epiphysis. However, variation in the literature exists to the total number as some authors suggest an extra centre at the femoral trochlea (Moiloi 2014; Zoetis et al. 2003).
Diverse degrees of malformation are observed in veterinary medicine, spanning from the complete absence of a joint to the lack of bony fusion in skeletal elements (Peterson & Kutzler 2011). These deviations from the normal anatomical configuration can arise due to hereditary influences stemming from genetic mutations, as well as external environmental factors such as physical injuries, pharmacological agents, and maternal illnesses. These factors collectively disrupt the intricate course of normal developmental processes (Bergère et al. 2015; Di Pietro et al. 2021)
The current body of literature lacks comprehensive description of defects pertaining to metaphyseal development of the distal femur. In this particular case involving incomplete ossification of the femoral condyle, we observe a condition similar to the extensively documented incomplete ossification of the humeral condyle (IOHC), or the potential occurrence of a traumatic fracture leading to nonunion.
The objective of this report is to present the diagnostic findings, including radiological and computer tomography (CT) assessments, surgical observations, and the results of treatment in the case of a developmental patella luxation attributed to incomplete ossification of the femoral condyles in a seven-month-old dog.
Patient presentation
A seven-month-old, 12.2 kg, neutered male crossbreed dog, acquired as a puppy from a welfare organisation at six weeks of age, was presented as a referral for investigation of chronic right pelvic limb lameness of 15 weeks duration. Initial radiographs were performed at four months of age, with referral at seven months. The dog had a history of developing an abnormal sit. At run or walk, no lameness was noted. No previous history of trauma was noted.
At presentation, the dog had a 2/5 weight-bearing lameness of the right pelvic limb with mild atrophy of the pelvic limb musculature (Nielsen et al. 2020). A notable click was present on hyperflexion of the right stifle with moderate pain on extension. A bony prominence was palpable proximolateral to the patella, with the patella luxated medially (grade 4). No joint instability was observed. Physical examination findings were otherwise unremarkable. Complete blood count, biochemistry including ionised calcium, T4, TSH, and urinalysis were unremarkable. Primary differential considerations, given the patient's age, include a congenital malformation with concurrent developmental patella luxation. Although a T fracture secondary to trauma, potentially resulting in nonunion, cannot be entirely dismissed, the absence of degenerative changes, callus formation, sclerosis, and physeal closure suggests a non-traumatic aetiology. Instead, an uncommon congenital issue affecting the lower femur is considered, differing from usual canine conditions.
Management and outcome
Repeat orthogonal mediolateral and craniocaudal radiographs of the left and right stifle were obtained under sedation to be compared to those obtained initially at four months of age. (55 kV and 3.2 mAs, GE Haulun Medical Systems, Beijing, China) (Figure 1).
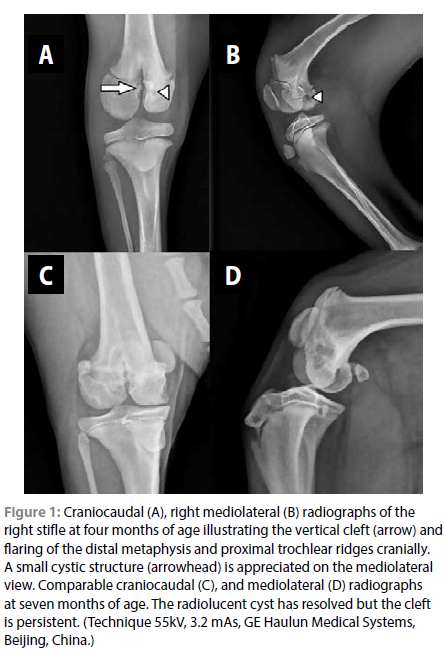
These revealed a persistent radiolucent vertical cleft between the femoral condyles of the right limb, resulting in complete separation of the condyles from each other with the absence of bone and extension of the fissure through the distal physis into the distal femoral metaphysis. There was mild sclerosis of the margins of the cleft within the metaphysis, which had shown some progression. The subchondral bone of the lateral femoral condyle was rounder than it should be when compared to the normal opposite limb. The subchondral bone was also mildly irregular, with a small cystic structure of the medial condyle seen on the initial radiographs but with resolution in the follow-up study. The distal femoral metaphysis was flared cranially, resulting in a triangular cranial projection of the metaphysis proximal to the physis, which was normal, with a flattening of the trochlear ridges. No stifle effusion was noted. The right femur was approximately 8 mm shorter than the left (on approximation, with differences in limb positioning). The proximal tibial physis and apophysis were comparable to the opposite normal limb.
Non-contrast transverse CT images were acquired in a bone window (WW 2000 WL 350) using a 64-slice helical scanner (Revolution Evo, GE Medical Systems), kV 120, 100 mAs, 1.3 mm slice thickness, and confirmed the right femur to be shorter than the left by approximately 2 cm. An irregular hypoattenuating cleft was confirmed between the right medial and lateral condyles, and extended from a cranial direction through the trochlear groove and cranial physis, caudomedially between the condyles. A shallow to nearly convex trochlear groove, with severe medial patella luxation, was present. The lateral condyle appeared to be positioned slightly caudally relative to the medial one. The cystic structure within the condyle was not identified on CT (Figure 2).
Following diagnostic imaging, the patient underwent surgical correction of the medial patella luxation and intercondylar cleft. Initial treatment consisted of placement of 3.5 mm cancellous transcondylar lag screw (Roth Medical, South Africa) from medial to lateral to prevent the risk of potential future fractures and to stimulate ossification between the condyles, block trochleoplasty, medial desmotomy, and lateral imbrication. Intraoperatively, an intact thin film of tissue was present extending from the distal portion of the cleft to the lateral joint, the origins of which were uncertain, as the cruciate ligaments and meniscus appeared normal (Figure 3).
Follow-up examination at six weeks revealed weight bearing lameness with relaxation of the patella medially. Follow-up radiographs (not provided) confirmed medial patella luxation but showed good intercondylar ossification. Revision sulcoplasty with removal of the original implants was performed. The medial trochlear ridge was heightened with the implantation of a Ridgestop (Ridgestop™, Orthomed UK) to aid in prevention of medial patella luxation. Postoperative radiographs (Figure 4) showed correct patella alignment with adequate intercondylar ossification. At five months following revision, the patient showed full weight bearing without noticeable lameness and had returned to normal activity.
Discussion
The Nomina Embryologica Veterinaria (World Association of Veterinary Anatomists 2017) currently represents the standard for which congenital anomalies are identified and classified. To date this is the only system in animals that recognises and allows the classification of many congenital limb malformations, however, this system is not canine-specific. The system to date only lists malformations without a definitive description. Currently no dysmorphia regarding the fusion of the distal femur is listed.
This study reports on the clinical, radiological, and CT patterns of a congenital malformation of the distal femur in the canine species. Clinical observation aids in the diagnosis of bone malformations so that the extent of the defects can be further evaluated with additional diagnostics. Recent evidence suggests that appropriate mechanical stimulation during embryonic movement is responsible for the normal bone ossification and morphogenesis, including tissue patterning of joint formation. There is, however, a lack of knowledge on how the mechanical signals are integrated with the biochemical signalling (Nowlan et al. 2010; Rolfe et al. 2013).
To the best of the authors' knowledge, no other congenital malformations of the distal canine femur are reported in the literature. In the human literature bifurcation of the distal femur (femoral duplication) is a rare congenital anomaly and is often reported to be associated with tibial hemimelia and/ or ectrodactyly (Gollop-Wolfgang complex) (Küsswetter et al. 1976). On rare occasions, bifurcation of the femur with a normal tibia and fibula have been reported (Ostrum et al. 1987). The condition has previously been described to result from splitting of the cartilaginous femoral anlage (primordium) early in development or as a result of ectopic tibial anlage. One human report describes a femoral bifurcation with a normal tibia and fibula suggesting that the bifurcation cannot be as a result of ectopic tibial anlage (Ostrum et al. 1987).
In this case, the radiographic appearance of the distal femur is similar to that seen in human patients with femoral bifurcation. The process of ossification in this patient had not occurred in the distal femur which was both confirmed radiographically and on CT with clear demonstration of an intercondylar cleft, similar to that seen in animals with humeral intercondylar fissures (HIF)/ incomplete ossification of the humeral condyle (IOHC). In dogs with HIF/IOHC the two major centres of the humeral condyle fail to fuse with medial and lateral sides separated by fibrous tissue (Carrera et al. 2008; Moores 2021). The main difference in this case being that the distal humerus does develop from two separate centres of ossification whilst the femur does not.
Proposed causes for cleft formation in the distal femur include reduced vascular density of the femoral condyle, lack of appropriate mechanical stimulation secondary to the developmental patella luxation, conformational abnormalities and hereditary or genetic factors that may have resulted in failure of the mineralisation of the femoral cartilaginous anlage shortly after birth. Mucopolysaccharidosis (MPS) VII has been reported in dogs with resultant delayed hypertrophic differentiation of epiphyseal chondrocytes leading to failure of secondary ossification but typically affects multiple joints (Peck et al. 2015). In general, little is known about the aetiology, pathogenesis, presentation and treatment of congenital limb deformities in dogs; in this case, no information was available regarding any traumatic event, inbreeding, environmental or genetic factors with the aetiology in this case remaining unknown. Unfortunately, a major limiting factor in this study is the lack of histopathology to allow correlation with diagnostic imaging. This may have led to less speculation as to the underlying cause.
The current knowledge about congenital limb malformations in dogs is poor, despite growing numbers of reports. Compared to human literature which contains descriptions for many congenital defects, veterinary literature is lacking complete and detailed descriptions for these defects.
Conflict of interest
The authors declare no conflict of interest directly or indirectly related to the research.
Ethical approval
This paper does not involve human patients. The owner of the dog in this study is aware that a case report has been written and has provided verbal consent for its publication. Signed consent was given for the treatment of this dog as part of my routine clinical caseload and this report details the management of the clinical case. Management was in no way altered in any way due to the writing of this case report.
ORCID
P Guy https://orcid.org/0000-0001-6003-1261
C Le Roux https://orcid.org/0000-0001-8333-5372
References
Bergère, A., Amzallag-Bellenger, E., Lefebvre, G., et al., 2015, Imaging features of lower limb malformations above the foot Diagn Interv Imaging 96, 901-14. https://doi.org/10.1016/j.diii.2014.08.008. [ Links ]
Carrera, I., Hammond, G.J., Sullivan, M., 2008, Computed tomographic features of incomplete ossification of the canine humeral condyle, Vet Surg 37, 226-31. https://doi.org/10.1111/j.1532-950X.2008.00370.x. [ Links ]
Di Pietro, S., Rapisarda, G.S., Cicero, L., et al., 2021, Four unusual cases of congenital forelimb malformations in dogs, Animals 11, 813. https://doi.org/10.3390/ani11030813. [ Links ]
Evans, H.E., De Lahunta, A., 2013, Miller's Anatomy of the Dog - E-Book, Elsevier Health Sciences. [ Links ]
Küsswetter, W., Matzen, K.A., Baumann, D., 1976, Bifurcation of the distal femur, Acta Orthop Scand 47, 648-52. https://doi.org/10.3109/17453677608988753. [ Links ]
Modina, S.C., Andreis, M.E., Moioli, M., et al., 2019, Age assessment in puppies: Coming to terms with forensic requests, Forensic Sci Int 297, 8-15. https://doi.org/10.1016/j.forsciint.2019.01.003. [ Links ]
Moioli, M., 2014, Appearance of ossification centers of the limbs and skeletal development in newborn toy-dog breeds: radiographic, morphometric and histological analysis, Doctoral Program in Veterinary Clinical Sciences, Università degli Studi di Milano, Milano. [ Links ]
Moores, A.P., 2021, Humeral intracondylar fissure in dogs, Vet Clin North Am Small Anim Pract 51, 421-437. https://doi.org/10.1016/j.cvsm.2020.12.006. [ Links ]
Nielsen, B.M.M., Pedersen, T., Mouritzen, A., et al., 2020, Kinetic gait analysis in healthy dogs and dogs with osteoarthritis: An evaluation of precision and overlap performance of a pressure-sensitive walkway and the use of symmetry indices, PLoS One 15, e0243819. https://doi.org/10.1371/journal.pone.0243819. [ Links ]
Nowlan, N.C., Sharpe, J., Roddy, K. A., et al., 2010, Mechanobiology of embryonic skeletal development: Insights from animal models, Birth Defects Res C Embryo Today 90, 203-13. https://doi.org/10.1002/bdrc.20184. [ Links ]
Ostrum, R.F., Betz, R.R., Clancy, M., et al., 1987, Bifurcated femur with a normal tibia and fibula, J Pediatr Orthop 7, 224-6. https://doi.org/10.1097/01241398-198703000-00025. [ Links ]
Peterson, M.E., Kutzler, M.A., 2011, Small animal pediatrics: The first 12 months of life, Saunders/Elsevier, pp. 443. [ Links ]
Rolfe, R., Roddy, K., Murphy, P., 2013, Mechanical regulation of skeletal development, Current Osteoporosis Reports 11, 107-116. https://doi.org/10.1007/s11914-013-0137-4. [ Links ]
World Association of Veterinary Anatomists 2017, Nomina Embryologica Veterinaria (Second Edition), World Association of Veterinary Anatomists, viewed 26 June 2022, <https://www.wava-amav.org/wava-documents.html> [ Links ].
Zoetis, T., Tassinari, M.S., Bagi, C., et al., 2003, Species comparison of postnatal bone growth and development, Birth Defects Res B Dev Reprod Toxicol 68, 86-110. https://doi.org/10.1002/bdrb.10012. [ Links ]
 Correspondence:
Correspondence:
email: peterguyvet@gmail.com














