Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
Journal of the South African Veterinary Association
versión On-line ISSN 2224-9435
versión impresa ISSN 1019-9128
J. S. Afr. Vet. Assoc. vol.94 no.1 Pretoria 2023
http://dx.doi.org/10.36303/JSAVA.558
CASE REPORT
Urethral cutaneous fistula correction using an autologous tunica vaginalis pedicle flap in a four-year-old intact male German shepherd dog
KM van de Wetering; RC Elliott
Department of Companion Animal Clinical Studies, Faculty of Veterinary Science, University of Pretoria, South Africa
ABSTRACT
Urethral cutaneous fistulas are rarely reported in doqs. Several techniques have been described to treat urethrocutaneous fistulas with different degrees of success. This case report is on a four-year-old male intact German shepherd diagnosed with urethrocutaneous fistulas after two weeks of dysuria. The urethra was repaired using an autologous tunica vaginalis pedicle flap after open castration and scrotal ablation. The dog was catheterised for two weeks after which a positive contrast urethrogram revealed a healed urethra with no stricture or leakage into surrounding tissue. The dog was discharged the following day after normal urination. Follow-up examination with the referring veterinarian at five months confirmed that the dog was clinically healthy and urinating normally. Literature about urethrocutaneous fistulas is lacking in the small animal field. To our knowledge there are no reports in the literature describing the use of an autologous tunica vaginalis pedicle flap for the repair of a urethral defect in dogs. This case report describes a novel technique to treat urethrocutaneous fistulas in an intact male dog.
Keywords: urethrocutaneous fistula, tunica vaginalis, urethral trauma, urethral tear, urethral defect
Introduction
Urethrocutaneous fistulas are rarely reported in dogs. They can be either congenital or acquired, with acquired being the most common and are often caused by trauma. The treatment of congenital fistulas entails ligation and excision and it is often possible to close the urethra without marked narrowing (Ralphs & Kramek 2003). Significant defects in the urethral mucosa often require autologous grafts or other techniques to reconstruct the urethra and divert urine to the normal anatomical urethral opening (Atalan et al. 2005).
Several techniques have been described for the treatment of urethral defects due to trauma. The most common being temporary urine diversion and secondary healing by epithelisation, primary healing after surgery and urine diversion and lastly permanent urine diversion as a salvage procedure (Cooley et al. 1999). There is currently no agreement on the length of time needed for healing of the urethra with urinary diversion, ranging from five days to 14 days (Meige et al. 2008). Evidence suggests that the two most important factors for urethral healing are tension free anastomosis and temporary urine diversion. This will limit the rate of anastomotic breakdown and limit stricture formation (Cooley et al. 1999). Although stricture formation is expected during urethral healing, a reduction of urethral diameter of 40% has been shown to have little clinical effect (Layton et al. 1987).
Given the rarity of traumatic urethrocutaneous fistula repair in dogs in the literature, there is limited information on the surgical approach to these cases. In human medicine buccal mucosal grafts have been used with good outcomes in 85.9% of cases (Lumen et al. 2012). Buccal mucosal grafts have been reported in 15 cats with 13 of the cats having excellent results with no complications at the donor site and normal urination (Yippaditr et al. 2022). Various types of autografts have been described in the veterinary literature, however most of these are described in small case series or experimental studies. An experimental study was performed on 14 dogs using fascia lata autografts. All 14 dogs had favourable outcomes with normal urinary function. In this experimental study, histopathology revealed urothelium in the entire lumen of the urethra at the graft site (Atalan et al. 2005).
The use of the tunica vaginalis as a substitute for the bladder wall in 10 male dogs resulted in good outcomes. This was an experimental study performed on healthy bladders (Wongsetthachai et al. 2011). The bladder wall of one dog on the edge of the tunica substitution site could not be distinguished macroscopically from normal bladder at the time of necropsy 10 weeks after the surgery. Histopathology also confirmed healing was complete 10 weeks after the procedure with all three layers of normal bladder present (Wongsetthachai et al. 2011). In a similar study performed in humans, free autografts of the tunica vaginalis for substitution urethroplasty showed good outcomes in 80% of the 52 dogs in the study population (Ashmawy & Magama 2018).
A single case report of an 11-month-old female dog diagnosed with urolithiasis and necrosis of the distal bladder neck and urethra has been described. The resulting defect was repaired with an axial pattern flap using the rectus abdominal muscle to reconstruct the bladder neck and urethra. In this case report, follow-up cystoscopy performed 2.5 years later revealed normal urethral mucosa without evidence of a stricture at the bladder neck (Savicky & Jackson 2009).
To our knowledge there are no reports in the literature describing the use of an autologous tunica vaginalis pedicle flap for the repair of a urethral defect in dogs.
Presentation
A four-year-old German shepherd dog was referred to the Onderstepoort Veterinary Academic Hospital with a history of dysuria for two weeks. A previous incident involving a dog bite to the perineum was reported, preceding the onset of dysuria. At that stage the owner perceived the injury as non-severe and decided not to pursue treatment. However, the dog subsequently presented to the referring veterinarian with a primary complaint of weight loss, pain over the perineal area and dysuria. On examination the referring veterinarian noticed multiple small fistulous lesions of the perineum ventral to the anus and palpated a firm tubular mass over the root of the penis. The owner did not observe the incident leading to the trauma and was not able to provide a reliable time period since the injury.
Upon presentation, the dog was alert and responsive but painful when his perineum was touched. A firm, painful mass was palpated on his perineum.
A further clinical examination was within normal limits except for the mass on the perineum. Complete blood count was performed (Table I). Packed cell volume was 35% and there was a marked inflammatory leukogram. Urinalysis revealed 4 plus erythrocytes. There were multiple fistulous tracts associated with the soft tissue mass in the perineum and a serosanguinous discharge from these tracts.
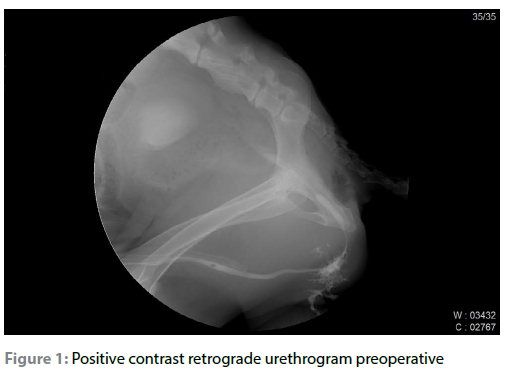
A positive contrast retrograde urethrogram was performed using fluoroscopy (Apelem Bacarra 90/20, Apelem DMS group, France) and positive contrast (Urografin 30% 1 ml/kg, Bayer, Berlimed SA, Madrid, Spain). A diagnosis of traumatic urethral cutaneous fistula suspected to be as a result of previous bite wounds to the perineum was made. The urethrogram also showed a urethral stricture at the bulb of the penis (Figure 1), as well as multiple areas of urine leakage into the tissue surrounding the urethra as well as leakage through the skin.
Given the length of the penile urethra that was affected, and the amount of fibrous tissue associated with the urethra and bulb of the penis, a novel technique using a vascularised pedicle graft from the tunica vaginalis after open castration was proposed. The surgery was discussed with the owner who consented to the procedure.
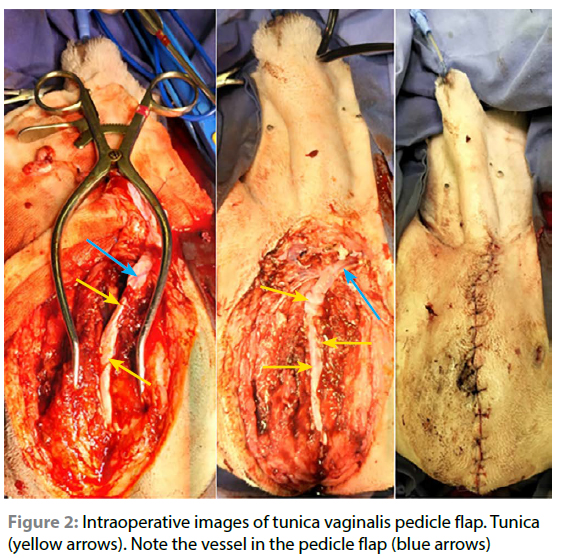
The dog was premedicated with medetomidine (0.01 mg/kg IM, Domitor 1 mg/ml, Zoetis, South Africa) and morphine sulphate (0.3 mg/kg IM, Morphine Sulphate PF, Fresenius Kabi, South Africa) and induced with propofol to effect (2 mg/kg IV, Propoven 1%, Fresenius Kabi, South Africa). The dog was intubated and placed on isoflorane (Isofor, Safeline pharmaceuticals, South Africa) in oxygen. An epidural injection was administered with morphine sulphate (0.1 mg/kg, Morphine Sulphate PF, Fresenius Kabi, South Africa) and ropivacaine (1 ml/4.5 kg ropivacaine, Naropin 10 mg/ml, Aspen pharmacare LTD). The abdomen, prepuce, scrotum and perineum were aseptically prepared, and the dog was placed in dorsal recumbency for surgery. A scrotal ablation and open castration were performed using a standard technique. Care was taken to manipulate the tunica as gently as possible to ensure no iatrogenic trauma to the vascular supply of the tunica. The incision from the caudal aspect of the scrotal ablation was then extended caudo-dorsally to the perineum over the root of the penis. The dog was catheterised through the prepuce and ostium of the penis with an 8FG sterile feeding tube. Placing the catheter facilitated identification of the urethra and the urethral mucosal defect. There was complete loss of the urethral mucosa that made up the roof of the urethra just distal to the penile root. There was a thin strip of mucosa on the cranial aspect of the urethra, making up the urethral floor. There were marked fibrous adhesions to the ishiocavernosus and bulbospongiosus muscles to the point that it was not possible to differentiate them from one another. The urinary catheter facilitated identification of the remaining urethral mucosa and the removal of the fibrous tissue. A vascularised strip of the tunica, 5 mm in width, and covering the entire defect was identified (Figure 2). The strip of tunic was sutured onto the dorsal aspect of the mucosa with simple interrupted 6-0 PDS (MonoPlus 6/0, B Braun surgical, Rubi, Spain) sutures replacing the mucosal defect, taking care to protect the blood supply (Figure 2.) onto the urethral defect.
Prior to closure, tissue samples from the perineum were taken for histopathology and culture. Closure was routine with a subcutaneous continuous suture pattern using 4/0 polyglyconate (Monosyn 4/0, B Braun surgical, Rubi, Spain) and a simple interrupted suture pattern using nylon 4-0 (Nylon 4/0, Gabler medical, Essex, United Kingdom) to close the skin.
Management and outcome
The dog was kept in the high care ward with an indwelling urinary catheter for two weeks post-surgery. Postoperatively the dog received morphine sulphate for three days (0.3 mg/kg IV, q4, Morphine Sulphate PF, Fresenius Kabi, South Africa), meloxicam for five days (0.1 mg/kg per os, q24, Metacam, Boehringer Ingelheim animal health, South Africa [Pty] Ltd) and was on maintenance fluids for three days (Ringers lactate, Fresenius Kabi Manufacturing SA [Pty] Ltd, South-Africa). The dog tolerated the catheter and no complications associated with the catheter were seen. The catheter was not removed during the entire two weeks as we were concerned that we may not be able to replace it. This was done to divert urine away from the flap to reduce risk of stricture formation.
The histopathology result from the perineal revealed a severe locally extensive chronic active pyogranulomatous myositis with a draining tract. The bacterial culture was negative after five days of incubation.
At two weeks post-surgery, the dog was sedated using medetomidine (0.01 mg/kg IM, Domitor 1mg/ml, Zoetis, South Africa) and the catheter was removed. A retrograde positive contrast urethrogram was performed using positive contrast (Urografin 30% 1 ml/kg, Bayer, Berlimed SA, Madrid, Spain) (Figure 3). The urethrogram showed no leakage of contrast and minimal stricture in the pelvic urethra. The urinary catheter was removed, and the dog monitored for a further 24 hours in the high care unit. A strong stream of urine was passed during voluntary urination by the dog the next morning. There was no dysuria and the dog was discharged the following day. The tip of the urinary catheter was sent for bacterial culture. The bacterial culture was negative after five days of incubation. The owner lived in a neighbouring province and was unable to return for a follow-up contrast study a month after the removal of the catheter. Telephonic follow-up with the referring veterinarian five months after the surgery confirmed that the dog was doing very well and urinating normally.

Discussion
Autologous tunica vaginalis free grafts have been used in humans to treat urethral strictures and rupture for more than 10 years (Ashmawy & Magama 2018). The outcomes are generally good to excellent with patients making a full recovery and being able to urinate normally (Ashmawy & Magama 2018). To our knowledge this is the first to report describing the use of a vascularised pedicle flap of tunica vaginalis in the repair of a urethral defect in a dog. This procedure is made easier in the intact male veterinary patient by the ability to perform a castration and harvest a flap long enough to cover large urethral defects. The advantage of this over a free flap is the attachment of the tunica to the dog maintaining the vascular supply. The advantage of maintaining the blood supply over a free graft of tunica cannot however be determined by a single case report. This is an area of study that can potentially be investigated in the future. The use of tunica for repair of defects of the urinary system has been shown to be effective in an experimental setting in the urinary bladder of dogs (Wongsetthachai et al. 2011). The length of tunica one can harvest from an open castration in a dog will usually reach the majority of the lower urinary tract. This makes it a versatile technique for repair of defects in the urinary tract.
Urinary diversion is critical to urethral healing (Meige et al. 2008). This will limit the formation of a clinical stricture and allow the urethral re-epithelisation. In these patients the use of an indwelling urinary catheter provides the best means of urinary diversion. Unfortunately, this will predispose the dog to an iatrogenic or catheter-induced infection. Thankfully, if healing is uncomplicated and the normal urine stream and frequency returns, these post-catheter infections often do not require antimicrobial therapy.
The limitations of this study are that it remains a single case that has been described retrospectively. There was no long-term follow up at the academic hospital and the final assessment was based on owner and referring veterinarian's reports. There is also no way to determine how the defect would have healed had we just performed urinary diversion with an indwelling catheter for two weeks.
However, the dog, by all reports, appears to have a good quality of life with no issues associated with urination. The authors suggest that the use of a vascularised pedicle flap of the tunica vaginalis provides a viable alternative option to repair urethral defects.
Conflict of interest statement
Dr Klaas-Jan Maurits van de Wetering declares that he has no conflict of interest. Dr Ross Christopher Elliott declares that he has no conflict of interest.
The authors declare no conflict of interest.
Funding sources
No funding.
Ethics
Ethics approval was obtained from the University of Pretoria, Faculty of Veterinary Science Research Ethics Committee (Ref: REC170-22).
ORCID
KM van de Wetering https://orcid.org/0000-0002-3902-2739
RC Elliott https://orcid.org/0000-0002-6774-7892
References
Ashmawy, H., Magama, P.T., 2018, Tunica vaginalis free graft urethroplasty: 10 years experience, African Journal of Urology 24, 37-40. https://doi.org/10.1016/j.afju.2017.09.008. [ Links ]
Atalan, G.N., CiHan, M., Sozmen, M., Ozaydin, I., 2005, Repair of urethral defects using fascia lata autografts in dogs, Veterinary Surgery 34, 514-518. https://doi.org/10.1111/j.1532-950X.2005.00077.x. [ Links ]
Cooley, A.J., Waldron, D.R., Smith, M.M., et al., 1999, The effects of indwelling transurethral catheterization and tube cystostomy on urethral anastomoses in dogs, J Am Anim Hosp Assoc 35, 341-7. https://doi.org/10.5326/15473317-35-4-341. [ Links ]
Layton, C.E., Ferguson, H.R., Cook, J.E., et al., 1987, Intrapelvic urethral anastomosis. A comparison of three techniques, Vet Surg 16, 175-82. https://doi.org/10.1111/j.1532-950X.1987.tb00933.x. [ Links ]
Lumen, N., Oosterlinck, W., Hoebeke, P., 2012, Urethral reconstruction using buccal mucosa or penile skin grafts: systematic review and meta-analysis, Urologia International 89, 387-394. https://doi.org/10.1159/000341138. [ Links ]
Meige, F., Sarrau, S., Autefage, A., 2008, Management of traumatic urethral rupture in 11 cats using primary alignment with a urethral catheter, Vet Comp Orthop Traumatol 21, 76-84. https://doi.org/10.1160/VCOT-07-01-0010. [ Links ]
Ralphs, S.C., Kramek, B.A., 2003, Novel perineal approach for repair of a urethrorectal fistula in a bulldog, Can Vet J 44, 822-3. [ Links ]
Savicky, R.S., Jackson, A.H., 2009, Use of a rectus abdominis muscle flap to repair urinary bladder and urethral defects in a dog, Journal of the American Veterinary Medical Association 234, 1038-1040. https://doi.org/10.2460/javma.234.8.1038. [ Links ]
Wongsetthachai, P., Pramatwinai, C., Banlunara, W., et al., 2011, Urinary bladder wall substitution using autologous tunica vaginalis in male dogs, Research in Veterinary Science 90, 156-159. https://doi.org/10.1016/j.rvsc.2010.05.015. [ Links ]
Yippaditr, W., Watanangura, A., Pencharee, D., et al., 2022, Buccal mucosal graft urethroplasty in male cats with traumatic complete urethral rupture, Journal of the American Veterinary Medical Association 260, 56-63. https://doi.org/10.2460/javma.20.09.0540. [ Links ]
 Correspondence:
Correspondence:
KM van de Wetering
Email: klaas-jan.vandewetering@up.ac.za














