Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
Journal of the South African Veterinary Association
versión On-line ISSN 2224-9435
versión impresa ISSN 1019-9128
J. S. Afr. Vet. Assoc. vol.91 no.1 Pretoria 2020
http://dx.doi.org/10.4102/jsava.v91i0.1720
ORIGINAL RESEARCH
Seal bites at sub-Antarctic Marion Island: Incidence, outcomes and treatment recommendations
Ryan R. ReisingerI, II; Miles PenfoldIII; Marthán N. BesterI; Gerhard SteenkampI, III
IDepartment of Zoology and Entomology, Mammal Research Institute, University of Pretoria, Pretoria, South Africa
IIDepartment of Zoology, Nelson Mandela University, Port Elizabeth, South Africa
IIIDepartment of Companion Animal Clinical Studies, Faculty of Veterinary Science, University of Pretoria, Pretoria, South Africa
ABSTRACT
Seal biologists at Marion Island (Southern Ocean) are in frequent contact with seals. During research activities, biologists may be bitten by seals, yet no standardised protocol for treating such bites is in place. Information on 22 seal bite cases at Marion Island was collected. Treatment of these bites varied, reflecting a need for standardised protocols for the treatment of bites. Recommendations for the in-field treatment of bites are presented. Five of the 22 cases had some symptoms which resembled 'seal finger' - a zoonotic infection, usually of the hands, that is contracted after a person comes into contact with tissues of seals or is bitten by one. However, in four of these cases, symptoms subsided within 4 days without antibiotic treatment; in the fifth case antibiotics were administered and symptoms subsided in 4 days. There is little evidence of the occurrence of seal finger at Marion Island, but this deserves further investigation.
Keywords: marine mammal; bite; treatment; infection; zoonoses.
Introduction
The Prince Edward Islands (46°54′S, 37°45′E) - comprising Marion Island and the smaller Prince Edward Island - are situated in the southern Indian Ocean. The islands support multiple breeding populations of three seal species: southern elephant seals Mirounga leonina (Phocidae), sub-Antarctic fur seals Arctocephalus tropicalis (Otariidae) and Antarctic fur seals Arctocephalus gazella (Otariidae) (Bester et al. 2011). Leopard seals Hydrurga leptonyx (Phocidae) are frequent transients during the austral spring and summer (Bester et al. 2006). Marine mammal research has been conducted on the islands since 1951 and a formal research programme commenced in 1973. Thenceforth, one to five marine mammalogists and their assistants were deployed annually on Marion Island (see Bester et al. 2011 for a history of the programme). During their research and monitoring activities, the seal biologists come in frequent contact with seals. For example, from 1993 to 2014, approximately 15 000 sub-Antarctic fur seal pups have been weighed (Oosthuizen et al. 2016) and seal biologists regularly draw blood from fur seals. During these activities, biologists may be bitten by seals, yet no standardised protocol for treating such bites is in place. Furthermore, seal biologists handle seal carcasses to perform necropsies or for osteological collections, and collect and process seal faeces. Protective measures, such as wearing gloves, are seldom undertaken (R.R. Reisinger and M.N. Bester, pers. obs.). It is therefore interesting that despite this there have been no reports of the zoonotic infection 'seal finger' from the island. This infection of the hands is contracted after a person comes into contact with blood, blubber or other tissues of pinnipeds or is bitten by one (Tryland 2018). The disease is common amongst professional seal hunters and those handling seal pelts and carcasses and, increasingly, amongst other professionals handling seals (biologists, aquarium personnel, wildlife workers, etc.) (Hartley & Pitcher 2002; Hunt et al. 2008). Most reports are from the northern hemisphere (e.g. Candolin 1953; Rodahl 1952; Waage 1950); in the southern hemisphere, only a small number of hand infections with clinical presentation similar to seal finger have been reported (Cawthorn 1994; Liavaag 1940; Panagis, Apps & Knight 1982).
The aim of this research was, firstly, to document the seal bites that researchers sustained at Marion Island over a 17-year period (1995-2012). Secondly, the treatment these researchers received was recorded and related to outcome. Thirdly, we offer suggestions for the treatment of seal bite wounds. Lastly, we discussed the apparently low risk of contracting 'seal finger' at this location.
Materials and methods
We contacted Marion Island seal biologists and asked them to provide details of any seal bites they had sustained, including treatment of the bite (as well as antibiotics administered, if any) and symptoms associated with the bite in the bitten limb. The South African Department of Environmental Affairs (DEA) released their available medical records for the island (n = 3 bite wounds) and medical staff (n = 3) that were stationed on the island and provided their personal records or recollections of bites.
Ethical considerations
Seal research on Marion Island was permitted by the Prince Edward Islands Management Committee (C06-08) and approved by the University of Pretoria's Animal Use and Care Committee (AUCC 040827-024).
Results
Bite responses
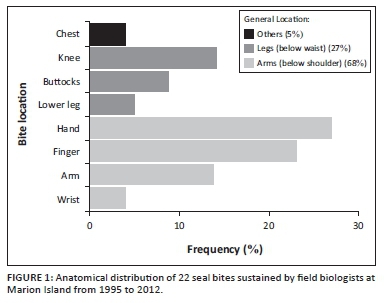
Eight field biologists (six men and two women, aged 23-28 years) reported 22 cases of seal bites from 1995 to 2012 (Table 1); three of these were included in the medical records. Biologists were bitten by all three of the seal species breeding on the island, but never by leopard seals. Sub-Antarctic fur seals were responsible for most of the bites (12 bites), followed by Antarctic fur seals (seven bites). Southern elephant seals were responsible for only three bites. Most bites (11) were sustained on the hands and fingers, but bites were also sustained on the forearms, knees, lower leg, buttocks, wrist and chest (Table 1; Figure 1). Treatment of bite wounds ranged from no treatment at all to thorough scrubbing with antiseptics, debridement, suturing and administering antibiotics (tetracycline and amoxicillin + clavulanic acid). Five cases (Table 1; cases 5-8 and 13) had some symptoms that could possibly resemble seal finger (Hartley & Pitcher 2002; Rodahl 1952; Tryland 2018), but in four of these cases, symptoms subsided within 4 days, without antibiotic treatment. In the fifth case (Table 1; case 13), antibiotics (including tetracycline) were administered and symptoms subsided in 4 days.
Bite treatment
Of the 22 cases of seal bites reported (Table 1), four cases were not treated, but some cleaning might have taken place during normal bathing of biologists. The remaining 18 cases were cleaned by flushing with saline, water or an antiseptic solution. Four of these cases were sutured to facilitate closure of wounds. Antibiotics were used prophylactically in seven cases. Six cases developed no signs of infection and the remaining case recovered within 4 days. Reported antibiotics used were amoxicillin+clavulanic acid or tetracyclines. The majority of wounds healed uneventfully. Only three cases (Table 1: cases 5, 7 and 13) showed symptoms of potential infection characterised by swelling, stiffness or pain. The remaining four cases (Table 1: cases 3, 4, 6 and 8) showed symptoms indicative of normal inflammatory response involved in wound healing and recovered without the use of antibiotics.
Discussion
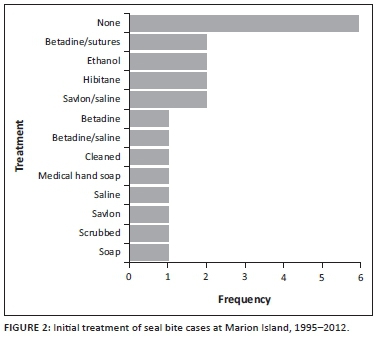
The use of at least 13 different wound treatment methods (Figure 2) amongst the 22 bite cases that we examined (Table 1) indicates a lack of knowledge of optimal in-field treatment of mammalian bite wounds.
All mammalian bite wounds are considered grossly contaminated (Ellis & Ellis 2014). Contamination is the presence of bacteria in the wound at concentrations that do not delay healing. Without timeous and appropriate treatment contamination may progress to infection, defined as the presence of replicating organisms in the wound with subsequent host injury (Edwards & Harding 2004), and may be characterised by fever, redness, swelling, pain, heat, loss of function and discharge from the wound (DeBoard et al. 2007; Edwards & Harding 2004; Patronek & Slavinski 2009; Velnar, Bailey & Smrkolj 2009) beyond the normal inflammatory phase. The wound healing process, which starts at the time of initial injury, can be arbitrarily divided into the following four main phases: (1) Coagulation and haemostasis. (2) Inflammation: the normal physiological response of the body to injury, clinically recognised in wounds by redness, swelling, pain, heat and loss of function. It establishes an immune barrier against invading micro-organisms, clears the wound of contaminants and foreign material and provides the injury site with the cells and chemical mediators needed for wound healing. It usually does not last for more than a few days (Broughton, Janis & Attinger 2006; Guo & DiPietro 2010; Reinke & Sorg 2012; Velnar et al. 2009). (3) Proliferation: it starts 3-10 days post-injury, covers the wound with granulation tissue, restores the vascular network, re-epithelialises the wound surface and decreases the surface area of the wound through contracture (Reinke & Sorg 2012). (4) Wound remodelling: connective tissue is realigned along tension lines and unneeded cells are removed (Reinke & Sorg 2012).
Following a seal bite, accepted bite wound management principles should be followed to optimise healing and prevent infection. As the most important step in optimising wound healing (Nicks et al. 2010), we recommend immediate (Patronek & Slavinski 2009) and thorough (Nicks et al. 2010) lavage of the wound with a physiological, sterile, non-cytotoxic solution such as saline or potable water (Fernandez & Griffiths 2008) until it is macroscopically clean to decrease contaminants and remove foreign material (Edwards & Harding 2004; Ellis & Ellis 2014; Kennedy, Stoll & Lauder 2015; Morgan & Palmer 2007; Owens & Wenke 2007; Patronek & Slavinski 2009; Smith, Walker & Brenchley 2003). Lavage can easily be performed in the field using a 20-mL syringe attached to a 21-G needle (Lam, Rastomjee & Dynan 2000) or 20-G catheter (Ellis & Ellis 2014). Surrounding skin should be cleaned (Ellis & Ellis 2014), dried and a sterile, non-adherent, semi-permeable, absorptive dressing must be applied to prevent further contamination of the wound environment, and to absorb wound exudate and promote wound healing (Abdelrahman & Newton 2011; DeBoard et al. 2007). Direct pressure can be applied over this dressing to stem any active bleeding (Edlich et al. 2010). Open wound management should be continued until the debridement phase is complete, followed by delayed primary or secondary wound closure (Edlich et al. 2010; Ellis & Ellis 2014; Jha, Khan & Siddiqui 2014; Morgan & Palmer 2007; Patronek and Slavinski 2009; Stevens et al. 2014). Prophylactic antibiotics are generally not indicated for 'low risk' bites (Morgan & Palmer 2007) but if deemed necessary, as in the case of deep puncture wounds of the hand, finger tendon sheaths or joints (Ellis & Ellis 2014; Jha et al. 2014; Kennedy et al. 2015), and in immune-compromised patients (Ellis & Ellis 2014), these should be directed against known pathogens of the biting animal's oral flora and the victim's skin (Patronek & Slavinski 2009). Antibiotics should be used as an adjunct to thorough wound washout as opposed to an alternative (Malahias et al. 2014). With signs of wound infection, microbial culture and sensitivity testing should be used for selection of appropriate antibiotics (Kennedy et al. 2015; Malahias et al. 2014; Nicks et al. 2010; Patronek & Slavinski 2009). Tetanus vaccination should be administered if the victim was immunised for more than five years prior to the bite (Ellis & Ellis 2014).
The higher incidence of bites on the fingers, hands and arms is expected because of the nature of the work being performed. However, it may also indicate the lack of use of appropriate protective clothing.
In spite of more than 40 years of seal research at Marion Island and thousands of contacts with three species of seal, no case of seal finger has been reported from the island. Our examination of 22 bite cases from the island provides little to no evidence of seal finger on the island. The stiffness experienced by the patient in case 13 (Table 1) might have been because of bruising and damage during the bite. Similarly, in spite of widespread sealing in the Antarctic and sub-Antarctic and extensive seal research activities (Basberg & Headland 2013; Laws 1993), few cases of possible seal finger were reported from the southern hemisphere (Cawthorn 1994; Liavaag 1940; Panagis et al. 1982). The two fur seal species occurring on Marion Island are from the same genus (Arctocephalus) as the fur seal species responsible for two of the aforementioned bite cases. Furthermore, Mycoplasma phocicerebrale, the putative causative agent of seal finger, has been isolated recently from Australian fur seals, Arctocephalus pusillus doriferus (Lynch et al. 2011). Handling southern elephant seal carcasses caused seal finger amongst sealers at South Georgia (Liavaag 1940) and a northern elephant seal, Mirounga angustirostris, bite has likely caused seal finger (Lewin, Knott & Lo 2004). Some cases of seal finger may have been diagnosed as erysipeloid (e.g. Hillenbrand 1953), but given the northern hemisphere provenance of most of the sealing vessels and crews in the Antarctic, it is very likely that Antarctic sealers would have been familiar with seal finger.
In 68.2% of bite cases, no antibiotics were used. In the remaining 31.8% of bite cases, at least two different antibiotics were used. Therefore, we conclude that the causative agent for seal finger was apparently not present during these bites or that lavaging most of them removed the organism.
Summary and recommendations
The large variety of wound treatments administered indicates a need for standardised training of personnel with currently accepted best medical practice (Figure 3) for the treatment of mammalian bites.
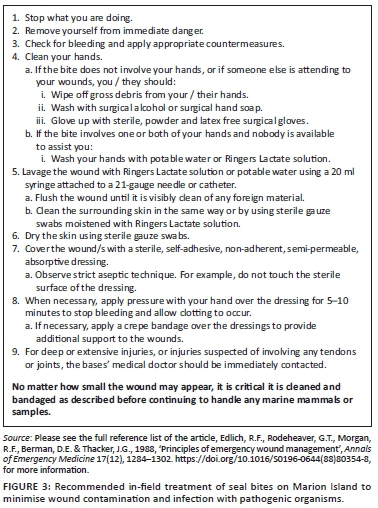
Firstly, we recommend that marine mammal biologists, veterinarians and medical staff at Marion Island and other Antarctic and sub-Antarctic research stations are to be better educated regarding seal finger and its treatment as well as in-field medical treatment of seal bites. Secondly, we recommend sealers must have immediate access to a 1-L bag of Ringer's lactate or potable water with 20-mL syringe and 21-G needle or catheter for in-field irrigation of seal bites together with a few sterile adhesive, non-adherent, semi-permeable, absorptive wound dressings as the most appropriate initial treatment for seal bites (Figure 3). Tetracycline should be used when seal finger is suspected, but because of the similarity of signs with Erysipelothrix (Hillenbrand 1953), a penicillin product should be administered concurrently (Stevens et al. 2014). The absence of reported seal finger from the island suggests that the putative agent may not be present. Better reporting of bites and their treatments would facilitate further investigations of seal finger.
Acknowledgements
The authors thank both the seal biologists and medical staff who responded to our enquiries and the Department of Environmental Affairs for releasing medical records.
Competing interests
The authors declare that no competing interests exist.
Authors' contributions
G.S. and M.N.B. conceived the study. R.R.R., G.S. and M.P. collected and analysed the data. R.R.R., M.P., M.N.B. and G.S. wrote the article.
Funding information
Funding for marine mammal research at the Prince Edward Islands was provided by the South African Department of Science and Technology, administered by the National Research Foundation, whilst the Department of Environmental Affairs provided logistical support. R.R.R. was supported by a National Research Foundation South African Network for Coastal and Oceanic Research (SANCOR) grant (94916) whilst preparing this article.
Data availability statement
Data available in Table 1.
Disclaimer
The views expressed in this article are those of the authors and not an official position of the institutions or funders.
References
Abdelrahman, T. & Newton, H., 2011, 'Wound dressings: Principles and practice', Surgery (Oxford) 29(10), 491-495. https://doi.org/10.1016/j.mpsur.2011.06.007 [ Links ]
Basberg, B.L. & Headland, R.K., 2013, 'The economic significance of the 19th century Antarctic sealing industry', Polar Record 49(4), 381-391. https://doi.org/10.1017/S0032247412000411 [ Links ]
Bester, M.N., de Bruyn, P.J.N., Oosthuizen, W.C., Tosh, C.A., McIntyre, T., Reisinger, R.R. et al., 2011, 'The marine mammal programme at the Prince Edward Islands: 38 years of research', African Journal of Marine Science 33(3), 511-521. https://doi.org/10.2989/1814232X.2011.637356 [ Links ]
Bester, M.N., Hofmeyr, G.J.G., Kirkman, S.P., Chauke, L.F., de Bruyn, P.J.N., Ferreira, S.M. et al., 2006, 'The leopard seal at Marion Island, vagrant or seasonal transient?', South African Journal of Wildlife Research 36(2), 195-198. [ Links ]
Broughton, G., Janis, J. & Attinger, C., 2006, 'The basic science of wound healing', Plastic and Reconstructive Surgery 117(Suppl 7), 12S-34S. https://doi.org/10.1097/01.prs.0000225430.42531.c2 [ Links ]
Candolin, Y., 1953, 'Seal finger and its occurrence in the gulfs of the Baltic Sea', Acta Chirurgica Scandinavica 177(Suppl), 1-50. [ Links ]
Cawthorn, M.W., 1994, 'Seal finger and mycobacterial infections of man from marine mammals: Occurrence, infection and treatment', Conservation Advisory Science Notes, No. 102, Department of Conservation, Wellington. [ Links ]
DeBoard, R.H., Rondeau, D.F., Kang, C.S., Sabbaj, A. & McManus, J.G., 2007, 'Principles of basic wound evaluation and management in the emergency department', Emergency Medicine Clinics of North America 25(1), 23-39. https://doi.org/10.1016/j.emc.2006.12.001 [ Links ]
Edlich, R.F., Rodeheaver, G.T., Morgan, R.F., Berman, D.E. & Thacker, J.G., 1988, 'Principles of emergency wound management', Annals of Emergency Medicine 17(12), 1284-1302. https://doi.org/10.1016/S0196-0644(88)80354-8 [ Links ]
Edlich, R.F., Rodeheaver, G.T., Thacker, J.G., Lin, K.Y., Drake, D.B., Mason, S.S. et al., 2010, 'Revolutionary advances in the management of traumatic wounds in the emergency department during the last 40 years: Part 1', Journal of Emergency Medicine 38(1), 40-50. https://doi.org/10.1016/j.jemermed.2008.09.029 [ Links ]
Edwards, R. & Harding, K.G., 2004, 'Bacteria and wound healing', Current Opinion in Infectious Diseases 17(2), 91-96. https://doi.org/10.1097/00001432-200404000-00004 [ Links ]
Ellis, R. & Ellis, C., 2014, 'Dog and cat bites', American Family Physician 90(4), 239-243. [ Links ]
Fernandez, R. & Griffiths, R., 2008, 'Water for wound cleansing', Cochrane Database of Systematic Reviews 23(1), CD003861. https://doi.org/10.1002/14651858.CD003861.pub2 [ Links ]
Guo, S. & DiPietro, L.A., 2010, 'Factors affecting wound healing', Journal of Dental Research 89(3), 219-229. https://doi.org/10.1177/0022034509359125 [ Links ]
Hartley, J.W. & Pitcher, D., 2002, 'Seal finger - Tetracycline is first line', Journal of Infection 45(2), 71-75. https://doi.org/10.1053/jinf.2002.1027 [ Links ]
Hillenbrand, F.K., 1953, 'Whale finger and seal finger; their relation to erysipeloid', Lancet 261(6762), 680-681. https://doi.org/10.1016/S0140-6736(53)91807-8 [ Links ]
Hunt, T.D., Ziccardi, M.H., Gulland, F.M.D., Yochem, P.K., Hird, D.W., Rowles, T. et al., 2008, 'Health risks for marine mammal workers', Diseases of Aquatic Organisms 81(1), 81-92. https://doi.org/10.3354/dao01942 [ Links ]
Jha, S., Khan, W.S. & Siddiqui, N.A., 2014, 'Mammalian bite injuries to the hand and their management', Open Orthopaedics Journal 8(Suppl 1:M9), 194-198. https://doi.org/10.2174/1874325001408010194 [ Links ]
Kennedy, S.A., Stoll, L.E. & Lauder, A.S., 2015, 'Human and other mammalian bite injuries of the hand: Evaluation and management', Journal of the American Academy of Orthopaedic Surgeons 23(1), 47-57. https://doi.org/10.5435/JAAOS-23-01-47 [ Links ]
Lam, D.G.K., Rastomjee, D. & Dynan, Y., 2000, 'Wound irrigation: A simple, reproducible device', Annals of the Royal College of Surgeons of England 82(5), 346-347. [ Links ]
Laws, R.M., 1993, Antarctic seals: Research methods and techniques, Cambridge University Press, Cambridge. [ Links ]
Lewin, M.R., Knott, P. & Lo, M., 2004, 'Seal finger', Lancet 364(9432), 448. https://doi.org/10.1016/S0140-6736(04)16768-8 [ Links ]
Liavaag, K., 1940, 'To tilfelleav "Spekk finger"', Tidsskrift fur Den Norske Legeforening 60, 173-178. [ Links ]
Lynch, M., Taylor, T.K., Duignan, P.J., Swingler, J., Marenda, M., Arnould, J.P.Y. et al., 2011, 'Mycoplasmas in Australian fur seals (Arctocephalus pusillus doriferus): Identification and association with abortion', Journal of Veterinary Diagnostic Investigation 23(6), 1123-1130. https://doi.org/10.1177/1040638711425699 [ Links ]
Malahias, M., Jordan, D., Hughes, O., Khan, W.S. & Hindocha, S., 2014, 'Bite injuries to the hand: Microbiology, virology and management', Open Orthopaedics Journal 8(Suppl 1: M4), 157-161. https://doi.org/10.2174/1874325001408010157 [ Links ]
Morgan, M. & Palmer, J., 2007, 'Clinical review: Dog bites', British Medical Journal 334(7590), 413-417. https://doi.org/10.1136/bmj.39105.659919.BE [ Links ]
Nicks, B.A., Ayello, E.A., Woo, K., Nitzki-George, D. & Sibbald, R.G., 2010, 'Acute wound management: Revisiting the approach to assessment, irrigation, and closure considerations', International Journal of Emergency Medicine 3(4), 399-407. https://doi.org/10.1007/s12245-010-0217-5 [ Links ]
Oosthuizen, W.C., de Bruyn, P.J.N., Wege, M. & Bester, M.N., 2016, 'Geographic variation in subantarctic fur seal pup growth: Linkages with environmental variability and population density', Journal of Mammalogy 97(2), 347-360. https://doi.org/10.1093/jmammal/gyv181 [ Links ]
Owens, B.D. & Wenke, J.C., 2007, 'Early wound irrigation improves the ability to remove bacteria', Journal of Bone & Joint Surgery 89(8), 1723-1726. https://doi.org/10.2106/JBJS.F.01210 [ Links ]
Panagis, K., Apps, P. & Knight, M.H., 1982, 'Seal finger: Occurrence in Antarctica', South African Journal of Antarctic Research 12, 49. [ Links ]
Patronek, G.J. & Slavinski, S.A., 2009, 'Animal bites', Journal of the American Veterinary Medical Association 234(3), 336-345. https://doi.org/10.2460/javma.234.3.336 [ Links ]
Reinke, J.M. & Sorg, H., 2012, 'Wound repair and regeneration', European Surgical Research 49(1), 35-43. https://doi.org/10.1159/000339613 [ Links ]
Rodahl, K., 1952, '"Spekk-finger" or sealer's finger', Arctic 5(4), 235-240. https://doi.org/10.14430/arctic3915 [ Links ]
Smith, M.R., Walker, A. & Brenchley, J., 2003, 'Barking up the wrong tree? A survey of dog bite wound management', Emergency Medicine Journal 20(3), 253-255. https://doi.org/10.1136/emj.20.3.253 [ Links ]
Stevens, D.L., Bisno, A.L., Chambers, H.F., Patchen Dellinger, E., Goldstein, E.J.C., Gorbach, S.L. et al., 2014, 'Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America', Clinical Infectious Diseases 59(2), e10-e52. https://doi.org/10.1093/cid/ciu296 [ Links ]
Tryland, M., 2018, 'Zoonoses and public health', in F.M.D. Gulland, L.A. Dierauf & K.L. Whitman (eds.), CRC handbook of marine mammal medicine, 3rd edn., pp. 47-61, CRC Press, Boca Raton, FL. [ Links ]
Velnar, T., Bailey, T. & Smrkolj, V., 2009, 'The wound healing process: An overview of the cellular and molecular mechanisms', Journal of International Medical Research 37(5), 1528-1542. https://doi.org/10.1177/147323000903700531 [ Links ]
Waage, P., 1950, 'Om spekkfinger behandling med aureomycin', Tidsskr Nor Lœgeforen 70(21), 679-681. [ Links ]
 Correspondence:
Correspondence:
Gerhard Steenkamp
gerhard.steenkamp@up.ac.za
Received: 03 Aug. 2018
Accepted: 17 Jan. 2020
Published: 24 Mar. 2020














