Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
Journal of the South African Veterinary Association
versão On-line ISSN 2224-9435
versão impressa ISSN 1019-9128
J. S. Afr. Vet. Assoc. vol.84 no.1 Pretoria Jan. 2013
CASE REPORT
Adipsia and hypernatraemia in a 6-month-old Staffordshire bull terrier
Vanessa McClure; Eran Dvir
Department of Companion Animal Clinical Studies, University of Pretoria, South Africa
ABSTRACT
A 6-month-old female Staffordshire bull terrier cross presented to the Onderstepoort Veterinary Academic Hospital with lethargy, weakness, decreased appetite, abnormal vocalisation, twitching of the facial muscles and ears, circling, alopecia, pruritus, seborrhoea sicca and erythema. Serum biochemistry revealed severe hypernatraemia (200.4 mmol/L; Reference Interval 140 mmol/L - 155 mmol/L). Treatment required careful administration of intravenous fluids. The electrolytes were monitored to ensure slow and controlled sodium normalisation (the target reduction of Na concentration was by 0.5 mmol/L/h - 1 mmol/L/h or 12 mmol/L/24 h - 24 mmol/L/24 h). Despite the careful fluid calculations and close monitoring, the serum sodium levels dropped more than the recommended 0.5 mmol/L/h -1 mmol/L/h in the first 4 h and the fluids had to be adjusted. The patient's habitus improved and the central nervous system signs started to resolve after 1 day of fluid treatment. The puppy started eating food mixed with water, but made no attempt to drink water. The pruritus and erythema resolved once the sodium levels normalised and the seborrhoea sicca began to resolve. At a follow up visit 20 days post discharge the skin was normal. A diagnosis of hypernatraemia as a result of pure water loss due to hypodipsia or adipsia was made, as the puppy made no attempt to drink water when her serum sodium levels increased (a strong thirst stimulus). Hypernatraemia recurred if she was not forced to take in adequate amounts of water mixed with her food. Dermatological changes such as seborrhoea, hyperkeratosis and alopecia have been reported in a few other cases of hypernatraemia in dogs and sodium levels should be investigated in dermatological patients when no other cause can be established. This study, supported by another retrospective study done in 2008, suggests that the Staffordshire bull terrier may be a breed that is predisposed to hypernatraemia.
Introduction
Sodium is the primary extracellular cation and the most important osmotically active solute in the body of all species. Serum sodium is maintained within a narrow range (140 mmol/L -155 mmol/L) in healthy individuals, even with large variations in daily sodium and water intake (Bagshaw, Townsend & McDermid 2009). The body is very sensitive to changes in osmolality and an increase of 2% in osmolality will stimulate the secretion of antidiuretic hormone (ADH) from the hypothalamus, reducing the loss of free water via the kidneys and stimulating the thirst centre, leading to increased drinking behaviour. In biological fluids, there is a negligible difference between osmolality and osmolarity (Di Bartola 2006), so osmolality will be used in this article.
Hypernatraemia is a potentially life-threatening electrolyte disorder (Di Bartola 2006; Kasai & King 2009). Marked hypernatraemia (sodium > 170 mmol/L) leads to severe clinical signs and can result in death (Goldkamp & Schaer 2007). Hypernatraemia represents a deficit of water in relation to the body's sodium stores. This can occur due to net water loss or sodium gain (ingestion of sodium containing products, metabolic or iatrogenic causes) (Adrogue & Madias 2000). Net water loss can be due to pure water loss (diabetes insipidus, insensible water loss or inadequate water intake) or hypotonic fluid loss (renal or extrarenal causes, see Table 1) (Adrogue & Madias 2000; Chapman, Petrus & Neiger 2009). Hypernatraemia, due to inadequate water intake, can be due to insufficient access to free water, an impaired or altered sensation of thirst or altered mental status. Hypernatraemia is a common finding in critically ill human patients in intensive care units. On admission, 2% - 6% of patients are already hypernatraemic, whilst 6% - 26% become hypernatraemic during the course of treatment in Intensive Care Units (Lindner & Funk 2012). These patients are often unconscious, sedated and intubated, and the physician manages their water intake, making them prone to hypernatraemia (Lindner & Funk 2012). Altered sensation of thirst can occur in aged humans as well as patients with acquired hypothalamic structural lesions (Bagshaw, Townsend & McDermid 2009).
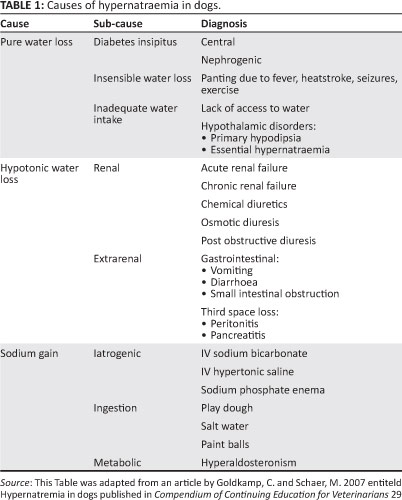
Pure water deficit due to altered sensation of thirst is an uncommon cause of hypernatraemia in animals (Chapman, Petrus & Neiger 2009). If the thirst response is absent due to a defect in the hypothalamus caused by trauma, neoplasia, inflammatory brain disease, hydrocephalus, congenital defects or idiopathic reasons (Goldkamp & Schaer 2007), it leads to the syndrome of primary hypodipsia or adipsia, and severe hypernatraemia results (Chapman, Petrus & Neiger 2009; Goldkamp & Schaer 2007). This syndrome has been documented as a congenital disorder of young miniature Schnauzers (Crawford, Kittelson & Fink 1984; Shimokawa Miyama et al. 2009; Van Heerden, Geel & Moor 1992). It has also been reported in several dogs (Chapman, Petrua & Neiger 2009; Crawford, Kittelson & Fink 1984; Hawks et al. 1991; Kang et al. 2007; Van Heerden, Geel & Moor 1992) and a cat that had an intracranial B-cell lymphoma (Morrison & Fales-Williams 2006).
Most of the clinical signs resulting from hypernatraemia involve the central nervous system (CNS). These include anorexia, lethargy, weakness, disorientation, ataxia, myoclonus, abnormal vocalisation, seizures, coma and death (De Morais & Di Bartola 2008; Di Bartola 2006; Kasai & King 2009; Schaer 2008). Metabolic acidosis can also occur due to an increased anion gap and decreased tissue perfusion with concurrent lactic acidosis (Goldkamp & Schaer 2007).
The more rapidly the hypernatraemia develops, the more severe the neurological signs will be (Adrogue & Madias 2000; De Morais & Di Bartola 2008; Marks & Taboada 1998). When severe hypernatraemia occurs acutely, cellular dehydration results in brain shrinkage, which leads to tearing of the cerebral blood vessels, resulting in brain haemorrhage or thrombosis (Adrogue & Madias 2000; Schaer 2008). These changes start to occur at a serum sodium concentration of > 170 mmol/L (Marks & Taboada 1998; Schaer 2008; Willard 2008). If the hypernatraemia occurs gradually, the brain shrinkage is countered by an adaptive response where the brain cells accumulate amino acids called 'idiogenic osmoles' (Adrogue & Madias 2000; James & Lunn 2007; Schaer 2008; Willard 2008). These idiogenic osmoles increase the intracellular osmolality and pull water back into the brain cells and restore their volume. The presence of these idiogenic osmoles is also the reason why rapid lowering of the serum sodium levels causes brain cells to accumulate water and swell, leading to cerebral oedema (Schaer 2008). This makes treatment of hypernatraemia complicated. Treatment involves administration of free water, correcting the metabolic acidosis if severe (pH < 7.15) and, where possible, eliminating the underlying cause without causing further damage to the brain (Feldman & Nelson 1996; Goldkamp & Schaer 2007; Willard 2008). Free water can be supplied parenterally or enterally to alleviate the hypernatraemia.
This report describes the diagnosis of hypernatraemia due to hypodipsia or adipsia in a puppy and discusses some expected changes and also skin changes most probably associated with the hypernatraemia.
Case history
A 6-month-old female Staffordshire bull terrier cross, weighing 8.6 kg, presented at Onderstepoort Veterinary Academic Hospital (OVAH) with clinical signs including lethargy, weakness, decreased appetite, abnormal vocalisation, twitching of the facial muscles and ears, circling, alopecia and erythema of the ventral abdomen, neck and medial thighs. The signs had been getting progressively worse over the past few months. The puppy did not appear to drink much. She had received her first two vaccinations and was fed a good quality dry puppy food. She had fallen from a height when the owner first got her. There was no history of exposure to any type of toxin or foreign substances. Pruritus was noted as well as severe seborrhoea sicca. The referring veterinarian found no parasites or fungi and treated the pruritis with prednisolone (0.5 mg/kg twice a day).
Clinical signs
On clinical examination the patient was weak, lethargic and hyperaesthetic when touched. The rectal temperature, pulse and respiration rate were all within normal limits. She appeared to be approximately 10% dehydrated. A neurological examination revealed a dull and depressed mental state and slight ataxia of all four limbs.
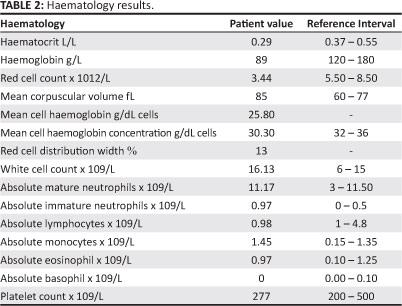
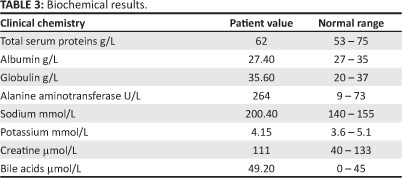
Haematology showed a moderate macrocytic, hypochromic, inappropriately regenerative anaemia and a mild inflammatory leukogram (Table 2). Biochemistry revealed severe hypernatraemia (200.4 mmol/L; reference interval [RI] 140 mmol/L - 150 mmol/L), mildly elevated alanine aminotransferase (ALT) (264 U/L; RI 9-73 U/L), and postprandial bile acids (49.2 µmol/L; RI 0 µmol/ - 45 µmol/L) (Table 3). The calculated plasma osmolality was severely elevated (410.5 mmol/L; RI 292 mmol/L - 308 mmol/L). The urine specific gravity (SG) was 1.050, which excluded renal failure and diabetes insipidus as the underlying causes. The rest of the urine analysis (dipstick and sediment evaluation) was within normal limits.
Thoracic radiographs were normal and abdominal ultrasound examination was unremarkable. A computer tomography (CT) scan of the head was performed with no significant findings. A diagnosis of primary hypodipsia with secondary hypernatraemia was made based on the severely elevated plasma sodium levels with no history of excessive sodium intake, the ability to concentrate urine and the fact that the dog was not interested in drinking water despite the chronically elevated sodium levels.
Treatment
On admission, the patient was placed on intravenous Ringers locate to supplement maintenance and ongoing losses. To replace the water deficit whilst avoiding a rapid reduction in serum sodium levels (no more than 0.5 mmol/L/h - 1 mmol/ L/h or 12 mmol/L/24 h - 24 mmol/L/24 h) (Adrogue & Madias 2000; Goldkamp & Schaer 2007; Marks & Taboada 1998), 0.45% sodium chloride (77 mEq/L sodium concentration) with 2.5% dextrose was administered intravenously through a second catheter. The rate was calculated at 25 mL/h using the following equations (Goldkamp & Schaer 2007):
Δ [Na]p = ([Na]inf - [Na]p) ÷ (TBW + 1) [Eqn 1]
Δ [Na]p = Change in patient's plasma sodium concentration caused by administration of 1L of the fluid selected.
[Na]inf = Sodium concentration of the selected fluid.
[Na]p = Patient's measured plasma sodium concentration.
TBW = total body water = 60% of body weight (BW) = 0.6 x BW = 5.16.
Therefore, for this patient:
Δ [Na]p = (77 - 200.4) ÷ ( 5.16 + 1) = -20 mmol/L
Serum Na must be reduced by 12 mmol/L in 24 h = 12 ÷ 20 = 0.6 L of the selected fluid over 24 h = 600 mL/24 h, 25 mL/h 0.45% NaCl and dextrose.
Maintenance fluid requirements = (BW x 30) + 70 [Eqn 2]
Maintenance fluid requirements for this dog = (8.6 x 30) + 70 over 24 h = 14mL/h Ringers lactate.
Ongoing losses estimated as 20 mL/kg/24 h = 500 mL/24 h = 21 mL/h Ringers lactate.
Total = 35 mL/h Ringers lactate
The electrolytes were monitored every 4 h - 8 h for the first two days and then daily, to determine whether any adjustment in the fluid rates or type needed to be made (Table 4).
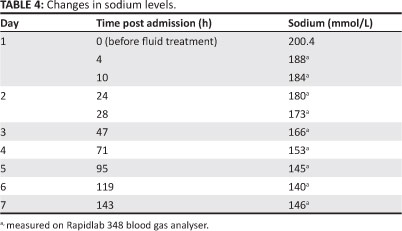
Despite the careful fluid calculations and close monitoring, the serum sodium levels dropped more than the recommended 0.5 mmol/L/h - 1 mmol/L/h in the first 4 h and so the fluids had to be adjusted. This rapid drop did not seem to cause any further deterioration in the puppy's neurological status.
After one day on IV fluids, the patient's habitus improved and the central nervous system signs resolved; she started eating food mixed with water. Once her sodium levels stabilised, the fluid rate was decreased and she was weaned off the fluids. For the superficial pyoderma she was started on cephalexin 30 mg/kg (Ranbaxy [SA] Pty Ltd, Centurion, Pretoria) twice a day.
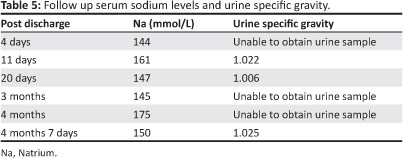
She was discharged once she was maintaining her sodium levels using food mixed with water. Her daily water requirements were calculated and that amount was added to her food over three feeds per day. The pruritus and erythema resolved with the normalisation of the serum sodium levels and the seborrhoea began to resolve. Follow-up visits were scheduled and her sodium levels and urine SG were monitored (Table 5). However, the puppy made no attempt to drink water and her sodium levels rose if she did not receive her full fluid requirements with her food, confirming the diagnosis of hypernatraemia due to hypodipsia or adipsia.
The skin lesions (pruritus, seborrhoea and erythema) also reoccurred when the serum sodium levels increased. The owner used the skin lesions as early warning signs that the sodium levels were increasing and returned the puppy for re-evaluation when this occurred.
Discussion
The diagnosis in this case was hypernatraemia from pure water loss due to primary hypodipsia or adipsia, as the following were ruled out: salt intoxication, hypertonic fluid administration, sodium gain, hypotonic fluid losses and pure water losses due to lack of access to water and hyperthermia or pyrexia. Primary hypodipsia or adipsia with resultant hypernatraemia has been documented as a congenital disorder of young miniature Schnauzers (Crawford, Kittelson & Fink 1984; Shimokawa Miyama et al. 2009; Van Heerden, Geel & Moor 1992) and there have been a few reports of it occurring in other breeds (Bagley et al. 1993; Chapman, Petrus & Neiger 2009; Hawks et al. 1991) and other species (Adrogue & Madias 2000; Morrison & Fales-Williams 2006).In a retrospective study of hypernatraemic dogs, four of the eight (50.00%) were Staffordshire bull terriers, compared to 2.10% of all dogs presenting to the Queen Mother Hospital, Royal Veterinary College. The median age at presentation was eight months (Chapman, Petrus & Neiger 2009). In this case, the patient was a Staffordshire bull terrier cross who was six months old, suggesting that the hypodipsia or adipsia might have been congenital, further supporting the indications that this breed might be predisposed.
In the above-mentioned retrospective study, the most consistent clinical finding was the presence of dermatological changes; all dogs had hyperkeratosis, seborrhoea and alopecia (Chapman, Petrus & Neiger 2009). In another case of hypernatraemia due to adipsia in a dog, severe seborrhoea was described as one of the clinical signs (Hawks et al. 1991). This case is another example of hypernatraemia leading to dermatological changes. The aetiology of these changes is unknown, but might be related to chronic dehydration of the stratum corneum (Chapman, Petrus & Neiger 2009). The stratum corneum serves as a primary barrier between the body and the environment (Mauldin 2013). Once this layer is damaged, allergens and pathogens are able to penetrate the epidermis and this can lead to pruritus, alopecia and secondary skin disorders.
Treatment for hypernatremia consists of administration of free water. Free water can be supplied parenterally or enterally (James & Lunn 2007; Willard 2008). If the patient will tolerate oral fluids, a naso-oesophageal tube can be inserted and water can be supplied that way; if this is not feasible then fluids should be given intravenously. Only hypotonic fluids are appropriate, including 0.45% sodium chloride (NaCl) or 5.00% dextrose. Conventional equations do not account for the sodium content in various fluid types and the impact they have on the patient's plasma sodium concentration (Goldkamp & Schaer 2007). The rate of infusion can be calculated from the following formula, which estimates the change in the serum sodium concentration caused by the retention of 1L of any infusate: Δ [NA]p = ([Na]inf- [Na]p) ÷ (TBW + 1).
The estimated ongoing losses and maintenance needs should be added to the fluid regimen using isotonic fluids (Goldkamp & Schaer 2007). The required volume and therefore the rate of infusion is then determined by dividing the change in the serum sodium concentration chosen for the given treatment period by the value obtained from the formula (Adrogue & Madias 2000; Goldkamp & Schaer 2007). Recommendations for changes in serum sodium concentrations vary slightly between references, but are approximately no more than 0.5 mmol/L/h - 1 mmol/L/h (or 12 mmol/L/24 h -24 mmol/L/24 h) (Adrogue & Madias 2000; Goldkamp & Schaer 2007). Serum electrolytes must ideally be monitored every two to 4 h, and the fluids adjusted accordingly to prevent the sodium levels from dropping too quickly (Goldkamp & Schaer 2007). In the above case, the serum levels dropped more than the recommended value in the first 4 h, but the total drop over 24 h was within the recommended range. The patient did not deteriorate due to the sudden drop in sodium as would have been expected. This could be due to the fact that the fluids were corrected soon after the drop was detected and the total drop over the 24 h period was still within the required range. When the clinical signs had been resolved, the patient could be managed as an outpatient by adding the daily fluid requirements to its food (Goldkamp & Schaer 2007). Drinking can be encouraged by placing flavouring in the water (beef or chicken stock mixed and made into ice cubes and added to the water). The prognosis is fair to good if no structural CNS abnormalities are present.
Normal physiological responses to increased plasma osmolality include the release of ADH and the stimulation of the thirst centre in the hypothalamus. Animals with adipsic or hypodipsic disorders make no effort to drink water despite their severely elevated plasma osmolality and sodium levels (Kang et al. 2007). Hypodipsic hypernatraemia has been documented in dogs as a congenital disorder caused by brain malformation (Schaer 2008). Acquired causes due to defects in the hypothalamus caused by trauma, neoplasia and infections can also occur (Chapman, Petrua & Neiger 2009). In this case the puppy had a history of trauma, but she was reportedly not drinking before the accident, so the hypodipsia is unlikely to be trauma induced. The CT scan of the brain showed no abnormalities, but is not the ideal modality to use to evaluate brain defects. Magnetic resonance imaging (MRI) would have been the modality of choice, but the owner declined it due to financial constraints. Abnormalities that have been described on MRI are: hydrocephalus (Chapman, Petrus & Neiger 2009), absence or dysgenesis of the corpus collosum (Chapman, Petrus & Neiger 2009; Shimokawa Miyama et al. 2009) and dysgenesis of forebrain structures (Shimokawa Miyama et al. 2009). Other causes of hypernatraemia were ruled out from the history and diagnostic tests, so this patient was thought to have hypodipsia due to a congenital disorder of the hypothalamus.
Conclusion
Hypernatraemia is a life-threatening electrolyte disorder that needs to be corrected carefully. The clinical signs caused by hypernatraemia are most commonly related to the CNS. The dermatological changes presented here are consistent with other case studies in dogs. Dermatological changes, especially seborrhoea, should be evaluated in hypernatraemic patients as a complication and not as an unrelated finding. Sodium levels should be investigated in dogs with dermatological problems when no other cause can be established. Staffordshire bull terrier may be a breed that is predisposed to hypernatraemia.
Acknowledgements
Competing interests
The authors declare that they have no financial or personal relationship(s) which may have inappropriately influenced them in writing this article.
Authors' contributions
V.M. (University of Pretoria) and E.D. (University of Pretoria) were the responsible clinicians that diagnosed and managed the case and wrote the article. Publication of this article was sponsored by the National Veterinary Clinicians Group of the South African Veterinary Association.
References
Adrogue, H.J. & Madias, N.E., 2000, 'Hypernatremia', The New England Journal of Medicine 342, 1493-1499. http://dx.doi.org/10.1056/NEJM200005183422006, PMid:10816188 [ Links ]
Bagley, R.S., De Lahunta, A., Randolph, J.F. & Centre, S.A., 1993, 'Hypernatraemia, adipsia and diabetes insipidus in a dog with hypothalamic dysplasia', Journal of the American Animal Hospital Association 29, 267-271. [ Links ]
Bagshaw, S.M., Townsend, D.R. & McDermid, R.C., 2009, 'Disorders of sodium and water balance in hospitalized patients', Canadian Journal of Anesthesiology 56, 151-167. http://dx.doi.org/10.1007/s12630-008-9017-2, PMid:19247764 [ Links ]
Chapman, P.S., Petrus, D. & Neiger, R., 2009, 'Hypodipsic hypernatremia in eight dogs', Tierärztliche Praxis 37, 15-20. [ Links ]
Crawford, M.A., Kittelson, M.D. & Fink, G.D., 1984, 'Hypernatraemia and adipsia in a dog', Journal of the American Veterinary Medical Association 184, 818-821. PMid:6725116 [ Links ]
De Morais, H.A. & Di Bartola, S.P., 2008, 'Hypernatremia: a quick reference', Veterinary Clinics of North America 38, 485-489. http://dx.doi.org/10.1016/j.cvsm.2008.01.025, PMid:18402874 [ Links ]
Di Bartola, S.P., 2006, 'Disorders of sodium and water: hypernatremia and hyponatremia', in: S.P. Di Bartola (ed.), Fluid therapy in small animal practice, 3rd edn., pp. 47-79, Saunders,St Louis. [ Links ]
Feldman, E.D. & Nelson, R.W., 1996, 'Water metabolism and diabetes insipidus', in: E.D. Feldman & R.W. Nelson (eds), Canine and feline endocrinology and reproduction, 3rd edn., pp. 2-44, Saunders, Philadelphia. [ Links ]
Goldkamp, C. & Schaer, M., 2007, 'Hypernatremia in dogs' Compendium of Continuing Education for Veterinarians 29, 148-161. [ Links ]
Hawks, D., Giger, U., Miselis, R. & Bovee, K.C., 1991, 'Essential hypernatraemia in a young dog', Journal of Small Animal Practice 33, 420-424. http://dx.doi.org/10.1111/j.1748-5827.1991.tb00970.x [ Links ]
James, K.M., & Lunn, K.F., 2007, 'Normal and abnormal water balance: hyponatremia and hypernatraemia', Compendium of Continuing Education for Veterinarians' 29, 589-609. [ Links ]
Kang, J., Chang, D., Lee, Y.W., Na, K. & Yang, M., 2007, 'Adipsic hypernatraemia in a dog with antithyroid antibodies in cerebrospinal fluid and serum', Journal of Veterinary Medical Science 69, 751-754. http://dx.doi.org/10.1292/jvms.69.751, PMid:17675808 [ Links ]
Kasai, C.M. & King, R., 2009, 'Hypernatraemia', Compendium of Continuing Education for Veterinarians 31, E1-E6, viewed 4 March 2013 from https://www.vetlearn.com/compendium/hypernatremia. [ Links ]
Lindner, G. & Funk, G., in press, 'Hypernatremia in critically ill patients', Journal of Critical Care, http://dx.doi.org/10.1016/j.jcrc.2012.05.001 [ Links ]
Marks, S.L. & Taboada, J., 1998, 'Hypernatraemia and hypertonic syndrome', Veterinary Clinics of North America 28, 533-543. [ Links ]
Mauldin, E.A., 2013, 'Canine ichthyosis and related disorders of cornification', Veterinary Clinics of North America 43, 89-97. http://dx.doi.org/10.1016/j.cvsm.2012.09.005, PMid:23182326 [ Links ]
Morrison, J. & Fales-Williams, A., 2006, 'Hypernatraemia associated with intracranial B-cell lymphoma in a cat', Veterinary Clinical Pathology 35, 362-365. http://dx.doi.org/10.1111/j.1939-165X.2006.tb00150.x, PMid:16967428 [ Links ]
Schaer, M., 2008, 'Theraputic approach to electrolyte emergencies', Veterinary Clinics of North America 38, 513-533. http://dx.doi.org/10.1016/j.cvsm.2008.01.012, PMid:18402878 [ Links ]
Shimokawa Miyama, T., Iwamoto, E., Umeki, S., Nakaichi, M., Okuda, M. & Mizuno, T., 2009, 'Magnetic resonance imaging and clinical findings in a miniature schnauzer with hypodipsic hypernatraemia', Journal of Veterinary Medical Science 71, 13871391. http://dx.doi.org/10.1292/jvms.001387, PMid:19887748 [ Links ]
Van Heerden, J., Geel, J. & Moore, D.J., 1992, 'Hypodipsic hypernatraemia in a miniature schnauzer', Journal of the South African Veterinary Association 63, 39-42. PMid:1569541 [ Links ]
Willard, M., 2008, 'Therapeutic approach to chronic electrolyte disorders', Veterinary Clinics of North America 38, 535-541. http://dx.doi.org/10.1016/j.cvsm.2008.01.013, PMid:18402879 [ Links ]
 Correspondence:
Correspondence:
Vanessa McClure
Private Bag X04
Onderstepoort 0110, South Africa
Email: vanessa.mcclure@up.ac.za
Received: 05 Nov. 2012
Accepted: 09 Apr. 2013
Published: 25 Oct. 2013














