Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
Journal of the South African Veterinary Association
versión On-line ISSN 2224-9435
versión impresa ISSN 1019-9128
J. S. Afr. Vet. Assoc. vol.82 no.1 Pretoria ene. 2011
ARTICLE ARTIKEL
Serial plasma glucose changes in dogs suffering from severe dog bite wounds
J P SchoemanI,*; A M KitshoffI; C J du PlessisI; P N ThompsonII
IDepartment of Companion Animal Clinical Studies, Faculty of Veterinary Science, University of Pretoria, Private Bag X04, Onderstepoort, 0110 South Africa
IIDepartment of Production Animal Studies, Faculty of Veterinary Science, University of Pretoria, Private Bag X04, Onderstepoort, 0110 South Africa
ABSTRACT
The objective of this study was to describe the changes in plasma glucose concentration in 20 severely injured dogs suffering from dog bite wounds over a period of 72 hours from the initiation of trauma. Historical, signalment, clinical and haematological factors were investigated for their possible effect on plasma glucose concentration. Haematology was repeated every 24 hours and plasma glucose concentrations were measured at 8-hourly intervals post-trauma. On admission, 1 dog was hypoglycaemic, 8 were normoglycaemic and 11 were hyperglycaemic. No dogs showed hypoglycaemia at any other stage during the study period. The median blood glucose concentrations at each of the 10 collection points, excluding the 56-hour and 64-hour collection points, were in the hyperglycaemic range (5.8- 6.2 mmol/ℓ). Puppies and thin dogs had significantly higher median plasma glucose concentrations than adult and fat dogs respectively (P < 0.05 for both). Fifteen dogs survived the 72-hour study period. Overall 13 dogs (81.3 %) made a full recovery after treatment. Three of 4 dogs that presented in a collapsed state died, whereas all dogs admitted as merely depressed or alert survived (P = 0.004). The high incidence of hyperglycaemia can possibly be explained by the 'diabetes of injury" phenomenon. However, hyperglycaemia in this group of dogs was marginal and potential benefits of insulin therapy are unlikely to outweigh the risk of adverse effects such as hypoglycaemia.
Keywords: dog bite wounds, glucose, SIRS, trauma.
INTRODUCTION
Published reports on the incidence of bite wounds in dogs and cats vary from 10.2 % to 14.7 % of trauma cases24, with a high incidence of severe bite wounds in intact male dogs weighing less than 10 kg39.The average dog's canine tooth can generate a crushing pressure of 150 to 450 pounds per square inch8,36. The shearing and tensile forces involved in the crushing and shaking of especially smaller dogs can cause a large amount of damage to the underlying fascia, muscle, vasculature, nervous tissue, bone and parenchymatous organs10,20,35,36, which predisposes these wounds to swelling, ischaemia and necrosis. This type of tissue damage is a result of the penetration of the dog's teeth from an area with elastic tissue to an area with less elastic tissue36. This phenomenon has been referred to as the 'iceberg effect', because the external wounds conceal the severity of the underlying damage10.
Local and systemic factors can influence the wound healing process. Some of the local factors needed for optimal wound healing include oxygen and nutrients9. During the early stages of healing, proteolysis of endogenous proteins mobilises amino acids, which are in turn used for glucose production10. Glucose is the primary source of energy for leucocytes and the predominating carbohydrate substrate for fibroblasts in their synthesis of proteoglycan polymers during wound healing10. However, excessively high plasma glucose concentrations can potentially inhibit neutrophil function by impairing phagocytosis and diminishing the production of oxygen radicals1,14.
Dogs with dog bite wounds are generally in a state of shock when admitted and are therefore under excessive sympathoadrenal control11,12,38. After injury there is a rapid increase in plasma cortisol levels, which peak within 4-6 hours and decrease to resting levels within 24 hours38. Changes in blood volume and afferent sensory nerve stimulation of the hypothalamus due to injury result in the release of catecholamines into the bloodstream23,38. These hormones increase cardiac output and raise blood pressure. Furthermore, epinephrine increases basal metabolic rate by as much as 100 % and stimulates metabolic activities such as glycogenolysis in the liver as well as glucose, cortisol and free fatty acid release into the blood38. Patients with severe injury therefore undergo an accelerated form of starvation7,11,37. During the hypermetabolic state, a number of alterations in carbohydrate metabolism are induced, these include1,23,34,42:
• Enhanced peripheral uptake and utilisation of glucose by the wound and other organs such as the liver and spleen, which are involved in the immune response;
• Increased glucose production stimulated by the release of epinephrine, cortisol, glucagon and growth hormone;
• Hyperlactataemia due to hypoperfusion;
• Decreased glucose production due to the release of gram-negative bacterial endotoxin, interleukin-6, insulin-like factors and decreased hepatic export or increased utilisation;
• Depressed glycogenesis due to the persistent high rate of glycogen breakdown under the influence of epinephrine and glucagon, decreased glycogen synthetase activity or the presence of tumour necrosis factor (TNF);
• A rise in extra-cellular glucose concentrations due to defective suppression of gluconeogenesis, glucose intolerance and resistance to the peripheral action of insulin, also termed 'diabetes of injury'.
Tissue trauma with or without infection can initiate the systemic inflammatory response syndrome (SIRS), in which multiple inflammatory, immunological, coagulation and fibrinolytic cascades are activated and interact18,20. SIRS is characterised by hypermetabolism, a hyperdynamic cardiovascular state and clinical manifestations of fever or hypothermia, tachycardia, tachypnoea and leucocytosis or leucopaenia4,18,44. Sepsis has been defined as SIRS with infection and severe sepsis as SIRS with infection and haemodynamic compromise18,20. Septic shock is defined as severe sepsis that requires both volume replenishment and inotropic support to restore tissue perfusion18. All these syndromes are commonly seen in dogs with bite wounds20.
Alterations in blood glucose concentrations represent one of the most consistent findings in models of experimentally induced sepsis6. Sepsis and SIRS can lead to hypoglycaemia due to impaired gluconeogenesis, especially from amino acids45and increased peripheral uptake and utilisation of glucose18,32. Lethal models of sepsis in animals demonstrate an initial hyperglycaemia followed by a phase of hypoglycaemia during which glucose production is suppressed6,32.
Hypothermia33, anorexia15, age2,29, pregnancy21,27 and breed2,27 have also been shown to influence blood glucose concentrations. A previous veterinary study has shown that blood glucose concentrations were significantly higher in dogs and cats with head trauma than in the control animals, but were not associated with outcome41. In contrast, canine babesiosis cases with low blood glucose concentrations were more likely to die22. However, dog bite wounds are peracute injuries usually inflicted on otherwise healthy animals and cannot be directly compared with a more chronic illness like babesiosis in which dogs can be presented days after the start of the disease process22. Hyperglycaemia has also been reported in dogs with heart failure5, a condition in which dogs are often presented days to months after the onset of the disease, rendering a comparison with acute trauma cases problematic.
The aim of this study was to describe the prevalence and prospective incidence of hypo-, normo-or hyperglycaemia in admitted canine bite wound cases over a 72-hour period. Historical, signalment and clinical factors were investigated to determine their possible effect on blood glucose concentrations.
MATERIALS AND METHODS
Twenty dogs presented to the Onderstepoort Veterinary Academic Hospital (OVAH) that had been bitten within the preceding 24 hours, with at least 1 open wound, and whose clinical condition, in the opinion of the attending outpatients clinician, warranted the use of intravenous fluid therapy, were recruited into the study. The criteria set out above were used in order to collect the most severely affected animals. All the patients recruited for the study were admitted to the Intensive Care Unit (ICU) of the OVAH. Possible Babesia canis infection was excluded by means of a peripheral blood smear, because this disease can result in perturbations in blood glucose concentrations22.In order to minimise any confounding influences on plasma glucose concentrations, all patients that received intravenous fluids containing dextrose or drugs that act by antagonising alpha2-receptors were excluded from the study. These cases presented over an 8-month period.
The dogs' owners signed a consent form and were asked to complete a questionnaire regarding the approximate time of the bite incident, time since the last meal, the dog's pregnancy status, known medical conditions and the administration of any medication prior to presentation.
On admission a full clinical examination was performed and habitus (alert, depressed or collapsed), age, sex, breed and body weight (Table 1), body condition (Purina Nine Point Body Condition Score), temperature, pulse and respiration were recorded. Blood was collected after a fasting period of at least 2 hours via the cephalic or jugular vein into a paediatric EDTA tube and a tube containing Sodium Fluoride Oxalate (NaF/Ox) 28. Additional, serial NaF/Ox samples for plasma glucose determination were taken at 8-hourly intervals post-trauma and haematology at 24-hour intervals, measured from the time the bite was inflicted, as indicated by the owners. These blood collection time points were selected with the purpose of comparing the dogs at similar times in the trauma pathway. A full haematological examination was also done on admission. The NaF/Ox samples were centrifuged within minutes of collection at a speed of 1730 g for 8 minutes. The plasma was separated and aliquoted into cryopreservation tubes, labelled and immediately frozen at -20 ºC. Glucose analysis was performed in a single batch using the hexokinase method, ensuring that the primary investigator was blinded as to the blood glucose concentrations of the patients for the duration of the study. Hypoglycaemia was defined as plasma glucose concentration below 3.3 mmol/ℓ 13,43and hyperglycaemia as plasma glucose concentration above 5.5 mmol/ℓ 43.
Temperature, pulse and respiration were recorded at each collection point. The study period extended from infliction of trauma to 72 hours, or until euthanasia or death. The study did not interfere with the normal clinical management of the cases.
Habitus at admission, time since last meal, time from infliction of trauma, age (<6 months = puppy; >6 months = adult), sex, body weight, body condition and outcome (died vs survived) were included as predictor variables for plasma glucose concentrations. Patients were classified into discrete, clinically meaningful categories of each predictor variable. The median plasma glucose concentration for each category of a variable was compared using Kruskal-Wallis 1-way ANOVA on ranks for multiple categories and the Wilcoxon rank sum test for 2 categories.
The presence of SIRS was determined from the admission data and other clinical and haematological data collected at 24-hour intervals after the initial trauma. To be considered SIRS positive, patients had to satisfy the following19,44:
• White cell count <6000/mm3or >16 000/mm3and/or >3 % band cells, plus at least 1 of the following:
- Rectal temperature of 38.1 or >39.2 ºC;
- Heart rate of >120 beats per minute;
- Respiratory rate of >20 breaths per minute.
The plasma glucose concentration of SIRS-positive and SIRS-negative groups were compared at each blood collection time point using the Wilcoxon rank sum test. The association between habitus on admission and outcome was assessed using Fisher's exact test. Statistical analysis was done using NCSS 2004 (NCSS, Kaysville, UT, USA.).
RESULTS
Signalment
The 3 dog breeds that were over-represented in this study included: Jack Russell terriers (5), Dachshunds (3) and Boerboels (3). The mean age of the patients in this study was 41.7 months. These patients had a mean weight of 10.1 kg and most dogs were females (11). Of the female dogs, 5 were intact (Table 1).
Outcome
Two dogs were euthanased within 8 hours of being bitten and only admission samples were obtained. One dog was euthanased after 48 hours. All instances of euthanasia were attributable to financial reasons and not prognosis. Another dog was discharged after 16 hours, also because of financial constraints; this dog's outcome was unknown. This left 16 dogs in the study in which mortality could be assessed. One dog died during the study period and 2 died thereafter. Thus, 15 of 16 dogs survived the 72-hour study period and 13 of 16 dogs made an eventual recovery. All the dogs admitted as either alert or depressed survived (12), whereas 3 of 4 of the dogs admitted as collapsed, died (P = 0.004).
Incidence of glucose abnormalities
The medians and inter-quartile ranges of plasma glucose concentrations and the proportion of dogs that were hypo-, normo-and hyperglycaemic at each given collection time point, are shown in Table 2.
On admission, 1 dog was hypoglycaemic, 8 were normoglycaemic and 11 were hyperglycaemic. None of the dogs showed hypoglycaemia during the remainder of the study period. The median plasma glucose concentration at each of the 10 collection points was consistently in the hyperglycaemic range (5.8-6.2 mmol/ℓ), excluding the 56-hour (5.4 mmol/ℓ) and the 64-hour collection points (5.5 mmol/ℓ), which were normoglycaemic. No dogs were found to be severely hypo-(<2.2 mmol/ℓ) or severely hyperglycaemic (>10 mmol/ℓ) during the study.
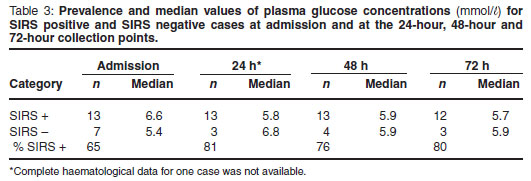
Systemic inflammatory response syndrome
The prevalence of SIRS at the 24-hour, 48-hour and 72-hour collection points is shown in Table 3. No significant differences in median plasma glucose concentrations between SIRS-positive and SIRSnegative dogs were detected at any collection point (Table 3).
Putative risk factors/predictor variables
No significant differences (P > 0.05) in the plasma glucose concentration were found, when assessing the groups within the different risk factors/predictor variables, with the exception of:
Habitus
• At the 32-hour collection point (depressed dogs = 5.6 mmol/ℓ; collapsed dogs = 6.3 mmol/ℓ).
Age
• On admission (puppy=7mmol/ℓ ; adult = 5.4 mmol/ℓ) .
• At the 8-hour collection point (puppy =7.6 mmol/ℓ ; adult = 5.7 mmol/ℓ) .
• At the 16-hour collection point (puppy = 7 mmol/ℓ ; adult = 6 mmol/ℓ) .
Body condition
• On admission (thin dogs = 6.8 mmol/ℓ ; fat dogs = 4.7 mmol/ℓ)
• At the 16-hour collection point (thin dogs = 6.9 mmol/ℓ; fat dogs = 4.5 mmol/ℓ)
A number of significant correlations were found between clinical or haematological variables and plasma glucose concentration:
• A positive correlation with respiratory rate (r s = 0.63; P = 0.0051) only on admission.
• A negative correlation (r s = -0.5467; P = 0.0126) with the total red cell count on admission; a negative correlation (r s = -0.5184; P = 0.0477) with the total red cell count at the 72-hour collection point.
• A negative correlation (r s = -0.5663; P = 0.0092) with haematocrit on admission; a negative correlation (r s = -0.5135; P = 0.0503) with haematocrit at the 72-hour collection point.
• A positive correlation (r s = +0.5406; P = 0.0306) with eosinophil count only at the 24-hour collection point.
DISCUSSION
This study has found a significantly lower survival rate in bite wound cases that presented in a collapsed state. The low survival rate of collapsed animals should be investigated further as this may prove to be a relevant measure of severity and predictor of outcome of dog bite wounds, as was found in a recent study in 100 dogs with virulent canine babesiosis3.
In contrast with the babesiosis study, no association was found between hypoglycaemia and collapse at presentation22. The low prevalence of hypoglycaemia might be attributed to the low case numbers. This study found no association between the degree of hypo-or hyperglycaemia and the eventual outcome, which was similar to a study on head trauma41.
Median plasma glucose concentrations were never in the hypoglycaemic range and hypoglycaemia was only encountered in 1 case on admission. The low incidence of hypoglycaemia found in this study was surprising, considering the fact that hypoglycaemia has been associated with profound metabolic illness and severe sepsis in dogs6,32,40.
A consistently high median plasma glucose concentration was found at all collection points, except at 56 and 64 hours (Table 2). Plasma cortisol levels in healthy hospitalised (stressed) dogs would provide additional information if it can be compared with the plasma cortisol levels in dogs with dog bite wounds. Stress during hospitalisation might thus have contributed to the hyperglycaemia and could perhaps explain why 40 % of dogs that presented with normal glucose levels subsequently developed hyperglycaemia.
During the post-traumatic 'ebb phase', the body's initial response is centred on the release of glycogen, the mobilisation of lipid stores and reducing energy expenditure. The metabolic rate declines during this phase, but increases later. The final stage of the ebb phase is recognised by marked sympatho-adrenal discharge, lasts approximately 24 hours and can be associated with hyperglycaemia13,32. If the animal survives this 'ebb phase', it progresses to the 'flow phase', which is characterised by an increased metabolic rate and enhanced breakdown of lean body mass. The afferent signals from the wound via pain and other peripheral receptors, as well as cytokines, interleukin 1 and tumour necrosis factor, initiate the process13,15,18. These signals are integrated in the hypothalamus and stimulate the secretion of glucagon, cortisol, catecholamines and growth hormone12,38. The net effect of these hormones, coupled with a defective suppression of gluconeogenesis and resistance to the peripheral action of insulin, is hyperglycaemia. This is all part of the hypermetabolic response to trauma12,30,34, which may last for 7-10 days12. This phenomenon has been described in human medicine in response to acute injury and has been termed 'diabetes of injury'42. A positive correlation has been found between the degree of hyperglycaemia and the risk of death in human trauma and cardiac patients42. In human critical care medicine, insulin resistance has been implicated as a major contributor to this phenomenon1,25,26,42. Aggressive control of even mildly elevated glucose concentrations, using insulin therapy, has shown a significant decline in death rates in human intensive care units, from 20.2 % to 10.6 %42. Insulin has been shown to counteract the metabolic changes in sepsis. It is hypothesised that insulin protects the endothelium (thereby contributing to the prevention of organ failure), modulates inflammatory pathways, protects cells from direct glucose toxicity, preserves hepatic mitochondrial function, improves dyslipidaemia and shows an anabolic effect by suppressing proteolysis and activating protein synthesis1,23,26,42. Although benefits have been documented with insulin therapy in humans, the use of insulin in small animal patients cannot yet be recommended due to the lack of supporting evidence23.
A high prevalence of SIRS was encountered (Table 3) on admission and during the study period. Sepsis has been defined as SIRS with an associated infection of the host by microorganisms. All bite wounds should be considered contaminated or dirty and infected and the local environment of the wound is ideal for bacterial replication and infection10,20,35, with subsequent bacteraemia and or endotoxaemia. A previous report states that these syndromes are frequently seen in dogs with bite wounds20, but no significant statistical differences in the median plasma glucose concentrations could be established between dogs with and without SIRS in our study. The trend seems to be the same as that in a previous retrospective study done on dogs with bacteraemia, in which 81.7 % of the dogs met the criteria for SIRS17. The criteria used for classification of SIRS19,44 have been questioned, because a large percentage of clinically healthy dogs have respiratory rates higher than 2017.
A limited number of significant associations were found between the predictor variables and plasma glucose concentration. It is interesting to note that puppies and thin dogs tended to have higher plasma glucose concentrations than adult or obese dogs, respectively, particularly during the 1st 16 hours of trauma. The authors hypothesise that these dogs might differ in their cortisol responses to traumatic scenarios or have age-related differences in their cortisol feedback mechanisms.
The differences in response to cortisol can also be the result of differing sensitivities of the GLUT 4 transport proteins to cortisol and glucagon. The positive correlation between respiratory rate on admission and the blood glucose levels can potentially be related to stress on admission. Higher cortisol and glucagon levels can result in a decrease in GLUT 4 activity23.
Increased utilisation of glucose by bacteria and polymorphonuclear leucocytes has been implicated in hypoglycaemia associated with sepsis6. Consequently, it is surprising that this study did not find any correlation between glucose concentration and leucocyte counts. The negative correlation between plasma glucose and haematocrit and the total red blood cell count can be the result of post-traumatic bleeding. Haemolysis can also be the result of infection due to an increase in the production of antibodies against red blood cells and the activation of the complement-and phagocytic systems. It has also been shown that certain bacteria produce haemolysins during septicaemia (Leptospira spp., Clostridium spp., Streptococcus spp. and Staphylococcus spp.)16 These bacteria made up 30 % of the aerobic and 36 % of the total bacteria cultured from dog bite wounds in a study conducted in the same hospital as our current study, in which 84 % of bite wounds yielded positive cultures31.
Due to the clinical and ethical nature of the study, all animals were maintained on Lactated Ringers solution (Ringers lactate, Fresenius Kabi) as intravenous infusion. Lactate can act as a precursor for glucose and, although unlikely, may have influenced the plasma glucose concentrations40.
Food, although standardised where possible, was allowed ad lib, but removed 2 hours before sampling and could have influenced the plasma glucose concentrations. It is believed that this is unlikely, because the dogs had very poor appetites due to the severity of their illness. Furthermore, feeding small amounts was only commenced after 24 hours, by which time the median glucose concentrations were already in the mild hyperglycaemic range and showed no appreciable increase after this time point. It would be unlikely for varying degrees of food intake to influence plasma glucose in such a consistent manner and we suggest that this phenomenon should be more thoroughly investigated in veterinary medicine. A study on normal beagles showed that 1-2 hours of food deprivation was sufficient to discount the intake of food's influence on blood glucose concentrations28. Other potential limitations of the study include:
• Low numbers of patients used with no control group for comparison.
• The differing levels of severity (although an attempt was made to select the most severely bitten animals) and the current unavailability of a meaningful severity score for bite wound cases.
• The influence of stress induced by hospitalisation.
• The low specificity of the SIRS criteria used.
CONCLUSIONS
The low incidence of hypoglycaemia is surprising considering the high incidence of SIRS encountered. There was no significant difference between the plasma glucose concentrations of the SIRS-positive and SIRS-negative cases. The results show an almost uniformly high median plasma glucose concentration over the 72-hour sampling period. Although the study has its limitations regarding other potential causes of the mild hyperglycaemia encountered, this could possibly be ascribed to the 'diabetes of injury' response as reported in the human ICU literature. This may warrant exploration in future larger studies, because the use of insulin in these human cases has shown a significant reduction of fatalities resulting from acute injury. Few important associations were made between historical and clinical variables and plasma glucose concentration. However, the high incidence of death in the collapsed group and the higher plasma glucose concentrations found in puppies and thin dogs warrants future investigation with a larger group of animals.
ACKNOWLEDGEMENTS
The authors would like to thank Mss Elsbe Myburgh and Gertie Pretorius of the Clinical Pathology Laboratory, Department of Companion Animal Clinical Studies (DCACS), for the analyses of samples. Gratitude is also extended to Dr M van Schoor of DCACS and Srs Y De Wit and L Coetzer of the ICU section, OVAH, for their help with the collection of the samples.
REFERENCES
1. Andersen S K, Gjedsted J, Christiansen C, Tønnesen E 2004 The role of insulin and hyperglycemia in sepsis pathogenesis. Journal of Leucocyte Biology 75: 413-421 [ Links ]
2. Atkins C E 1984 Disorders of glucose homeostasis in neonatal and juvenile dogs: Hypoglycemia - Part I. Compendium on Continuing Education for the Practicing Veterinarian 6: 197-208 [ Links ]
3. Böhm M, Leisewitz A L, Thompson P N, Schoeman J P 2006 Capillary and venous Babesia canis rossi parasitaemias and their association with outcome of infection and circulatory compromise. Veterinary Parasitology 14: 18-29 [ Links ]
4. Bone R C, Balk R A, Cerra F B 1992 Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest 101: 1644-1655 [ Links ]
5. Brady C A, Hughes D, Drobatz K J 2004 Association of hyponatremia and hyperglycemia with outcome in dogs with congestive heart failure. Journal of Veterinary Emergency and Critical Care 14: 177-182 [ Links ]
6. Breitschwerdt E B, Loar A S, Hribernik T N, McGrath R K 1981 Hypoglycemia in four dogs with sepsis. Journal of the American Veterinary Medical Association 178: 1072-1076 [ Links ]
7. Chandler M L, Greco D S, Fettman M J 1992 Hypermetabolism in illness and injury. Compendium on Continuing Education for the Practicing Veterinarian 14: 1284-1290 [ Links ]
8. Cowell A K, Penwick R C 1989 Dog bite wounds: a study of 93 cases. Compendium on Continuing Education for the Practicing Veterinarian 11: 313-318 [ Links ]
9. Crane S W 1989 Nutritional aspects of wound healing. Seminars in Veterinary Medicine and Surgery (Small Animal ) 4: 263-267 [ Links ]
10. Davidson E B 1998 Managing bite wounds in dogs and cats - Part I. Compendium on Continuing Education for the Practicing Veterinarian 20: 811-820 [ Links ]
11. Devey J J, Crowe D T 1997 The physiologic response to trauma. Compendium on Continuing Education for the Practicing Veterinarian 19: 962-974 [ Links ]
12. Douglas R G, ShawJHF 1989 Metabolic response to sepsis and trauma. British Journal of Surgery 26: 115-122 [ Links ]
13. Feldman E C, Nelson R W 1996 Beta cell neoplasia: insulinoma. In Canine and feline endocrinology and reproduction (2nd edn). W B Saunders, Philadelphia: 616-644 [ Links ]
14. Fowler D J 1989 Wound healing: an overview. Seminars in Veterinary Medicine and Surgery (Small Animal ) 4: 256-262 [ Links ]
15. Gienna E M, Davidson J R 2003 Nutritional support of hospitalized cats and dogs. In Slatter D (ed.) Textbook of small animal surgery Vol. 1. Elsevier Science, Philadelphia: 87-113 [ Links ]
16. Giger U 2005 Regenerative anaemias caused by blood loss or hemolysis. In Ettinger S J, Feldman E C (eds) Textbook of veterinary internal medicine Vol. 2. Elsevier Science, St. Louis, Mo.: 1886-1907 [ Links ]
17. Greiner M, Wolf G, Hartmann K 2008 A retrospective study of the clinical presentation of 140 dogs and 39 cats with bacteraemia. Journal of Small Animal Practice 49: 378-383 [ Links ]
18. Hackner S G 1999 Endocrine and metabolic emergencies. In King L, Hammond R (eds) BSAVA manual of canine and feline emergency and critical care . British Small Animal Veterinary Association, Cheltenham: 177-190 [ Links ]
19. Hauptman J G, Walshaw R, Olivier N B 1997 Evaluation of the sensitivity and specificity of diagnostic criteria for sepsis in dogs. Veterinary Surgery 26: 393-397 [ Links ]
20 Holt D E, Griffin G 2000 Bite wounds in dogs and cats. Veterinary Clinics of North America: Small Animal Practice 30: 669-679 [ Links ]
21. Jackson, R F, Bruss, M L 1980 Hypoglycemia - Ketonemia in the pregnant bitch. Journal of the American Veterinary Medical Association 177: 1123-1127 [ Links ]
22. Keller N, Jacobson L S, Nel M, de Clerq M, Thompson P N, Schoeman J P 2004 Prevalence and risk factors of hypoglycemia in virulent canine babesiosis. Journal of Veterinary Internal Medicine 18: 265-270 [ Links ]
23. Knieriem M, Otto C M, Macintire D 2007 Hyperglycemia in critically ill patients. Compendium on Continuing Education for the Practicing Veterinarian 29: 360-372 [ Links ]
24. Kolata R J, Kraut N H, Johnston D E 1974 Patterns of trauma in urban dogs and cats: a study of 1000 cases. Journal of the American Animal Hospital Association 164: 499-502 [ Links ]
25. Krinsley J S 2003 Association between hyperglycemia and increase hospital mortality in a heterogenous population of critically ill patients. Mayo Clinical Proceedings 78: 1471-1478 [ Links ]
26. Langouche L, Vanhorebeek I, Vlasselaers D, Vander Perre S, Wouters P J, Skogstrand K, Hansen T K, Van den Berghe G 2005 Intensive insulin therapy protects the endothelium of critically ill patients. The Journal of Clinical Investigation 115: 2277-2286 [ Links ]
27. Leifer C E, Peterson M E Hypoglycemia. 1984 Veterinary Clinics of North America: Small Animal Practice 14: 873-889 [ Links ]
28. McKelvie D H, Powers S 1966 Microanalytical procedures for blood chemistry - a long term study on beagles. American Journal of Veterinary Research 27: 1405-1412 [ Links ]
29. McMicheal M, Dhupa, N 2000 Pediatric critical care medicine: specific syndromes. Compendium on Continuing Education for the Practicing Veterinarian 22: 353-359 [ Links ]
30. Mĕszăros K, Lang C H, Bagby G J, Spitzer J J 1987 Contribution of different organs to increased glucose consumption after endotoxin administration. Journal of Biological Chemistry 262: 10965-10970 [ Links ]
31. Meyers B, Schoeman J P, Goddard A, Picard, J 2008 The bacteriological and antimicrobial susceptibility of infected and non-infected dog bite wounds: fifty cases. Veterinary Microbiology 127: 360-368 [ Links ]
32. Mizock B A 1995 Alterations in carbohydrate metabolism during stress: a review of the literature. American Journal of Medicine 98: 75-83 [ Links ]
33. Oncken A E, Kirby R, Rudloff E 2001 Hypothermia in critically ill dogs and cats. Compendium on Continuing Education for the Practicing Veterinarian 23: 506-521 [ Links ]
34. Patiño J F, de Pimiento S E, Vergara A, Savino P, Rodríguez M, Escallón J 1999 Hypocaloric support in the critically ill. World Journal of Surgery 23: 553-559 [ Links ]
35. Pavletic M M, Trout N J 2006 Bullet, bite and burn wounds in dogs and cats. Veterinary Clinics of North America: Small Animal Practice 36: 873-893 [ Links ]
36. Pavletic M M 1996 Gunshot wound management. Compendium on Continuing Education for the Practicing Veterinarian 18: 1285-1299. [ Links ]
37. Remillard R L, Martin R A 1990 Nutritional support in the surgical patient. Seminars in Veterinary Medicine and Surgery (Small Animal ) 5: 197-207 [ Links ]
38. Rosin E 1981 The systemic response to injury. In M J Bojrab (ed.) Disease mechanisms in small animal surgery (1st edn). Lipincott, Williams and Wilkins, Philadelphia: 3-11 [ Links ]
39. Shamir M H, Leisner S, Klement E, Gonen E, Johnston D E 2002 Dog bite wounds in dogs and cats: a retrospective study of 196 cases. Journal of Veterinary Medicine 49: 107-112 [ Links ]
40. Sonnenwirth A C, Jarett L 1980 Clinical chemistry. In Gradwohl's clinical laboratory methods and diagnose s (8th edn). CV Mosby, St Louis: 218-234 [ Links ]
41. Syring R S, Otto C M, Dobratz K J 2001 Hyperglycemia in dogs and cats with head trauma: 122 cases (1997-1999). Journal of the American Veterinary Medical Association 218: 1124-1129 [ Links ]
42. Van den Berghe G 2004 How does glucose control with insulin save lives in intensive care? Journal of Clinical Investigation 114: 1187-1195 [ Links ]
43. Walters P C, Drobatz K J 1992 Hypoglyceamia. Compendium on Continuing Education for the Practicing Veterinarian 14: 1150-1158 [ Links ]
44. Welzl C, Leisewitz A L, Jacobson LS, Vaughan-Scott T, Myburgh E 2001 Systemic inflammatory response syndrome and multiple-organ damage/dysfunction in complicated canine babesiosis. Journal of the South African Veterinary Association 72: 158-162 [ Links ]
45. Woolf L I, Groves A C, Duff J H 1979 Amino acid metabolism in dogs with E. coli bacteremic shock. Surgery 85: 212-218 [ Links ]
Received: January 2011.
Accepted: March 2011.
* Author for correspondence. E-mail: johan.schoeman@up.ac.za














