Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Sports Medicine
On-line version ISSN 2078-516X
Print version ISSN 1015-5163
SA J. Sports Med. vol.30 n.1 Bloemfontein 2018
http://dx.doi.org/10.17159/2078-516x/2018/v30i1a5020
ORIGINAL RESEARCH
A four-week home-based exercise programme is effective in treating subacute low back pain in adults
M J LumbI; L LateganII
IHons; Department of Sport and Movement Studies, Faculty of Health Sciences, University of Johannesburg, Cnr Joe Slovo Drive and Beit St, 2001 Doornfontein, Johannesburg Gauteng, South Africa
IIPhD; Department of Sport and Movement Studies, Faculty of Health Sciences, University of Johannesburg, Cnr Joe Slovo Drive and Beit St, 2001 Doornfontein, Johannesburg Gauteng, South Africa
ABSTRACT
BACKGROUND: Low back pain (LBP) is a prevalent condition affecting a large portion of the population worldwide and it is one of the leading causes of morbidity and work absenteeism.
OBJECTIVES: To investigate the effectiveness of a four-week, home-based exercise programme in treating subacute LBP in adults.
METHODS: A quantitative experimental research design was used. Twenty male and female adults (between 18 and 65 years) with subacute LBP were recruited by means of advertisements and word of mouth and allocated into either a control group (CG) or a home-based exercise group (HG). Both groups underwent a pre-test that consisted of answering two questionnaires, the Visual Analogue Scale for Pain (VASP) and the Oswestry Low Back Pain and Disability Questionnaire. The CG received no intervention over the four-week intervention period, while the intervention group (HG) was given an exercise programme and instructed to perform the exercises at home, three times a week for four weeks. After four weeks (post-test), the two questionnaires were repeated. After eight weeks (the follow-up test) both groups again completed the two questionnaires. Descriptive statistics, non-parametric inferential statistics and Cohen's effect size (d) were used to analyse the data and statistical significance was set at a confidence level of 95% (p<0.05).
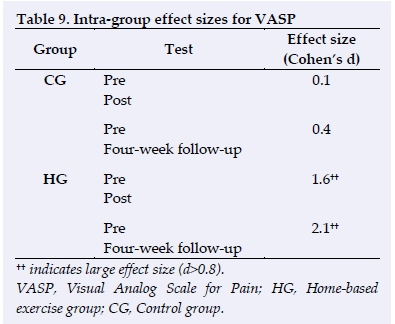
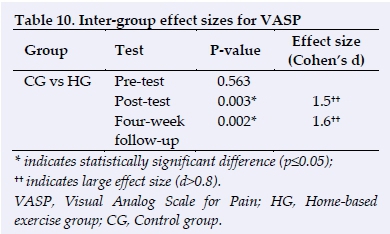
RESULTS: Following the home-based exercise intervention there were significant improvements observed in low back pain and function for the HG. The HG's Oswestry scores improved significantly (p=0.005) and their VASP also showed a significant improvement (p=0.011). Significant improvements also occurred between the pre-test and four-week follow-up for the HG's Oswestry score (p=0.021) and for the HG's VASP (p=0.005). No significant improvement was found for the CG between pretest and post-test or between pretest and the four-week follow-up. Large effect sizes (d>0.8) were also observed for the HG between the pretest and the post-test (d=1.6), as well as between the HG and the CG at post-test (d=1.5) and at the four-week follow-up (d=1.6).
CONCLUSION: The exercise intervention resulted in statistically significant and clinically significant improvements in both function and pain in adults with subacute LBP.
Keywords: musculoskeletal rehabilitation, spine, function, movement
Low back pain (LBP) is a prevalent condition affecting a large portion of the population worldwide. [1] It is pain that is experienced in the lumbar spine region. It is also one of the leading causes of morbidity and work absenteeism and therefore, cost-effective strategies used to treat this condition are important. [1] Over 70% of the global population will experience LBP during their lifetime. [1] Low back pain is a very common health problem, peaking between the ages of 35 to 55 years old. [1]
Numerous studies have demonstrated the favourable effects of rehabilitative exercise on reducing subacute (four weeks to three months) and chronic (longer than three months) LBP.[2,3] Some studies have also demonstrated that rehabilitative exercise is not effective when treating acute (<4 weeks) LBP.[2,3] Rehabilitative exercise combined with education is considered essential when treating LBP and is regarded as the ideal intervention in its prevention.[4,5,6] Other interventions, such as education alone, shoe inserts and back braces/belts, do not seem to prevent cases of low back pain[6]. In developing countries like South Africa, where more than 55% of its population live below the poverty line and are not covered by medical insurance, finding cost-effective and evidence-based strategies to treat LBP are important. [7]
Exercise therapy has numerous benefits in treating LBP, specifically subacute [2,3,8] and chronic LBP [2,3], as it aims to correct biomechanical discrepancies and muscle imbalances. [2,3,8]. Exercise helps to develop core stability and increases range of motion. [2] A combination of aerobic, strength and stretching exercises have been reported to be more effective in treating LBP than leaving it untreated. [2] Certain studies have displayed the effectiveness of non-supervised exercise in the reduction of chronic low back pain and functionality at work. [9] Exercise therapy has been shown to be more cost-effective than other treatments in the treatment of chronic and subacute low back pain. [10] However, few studies have explored the effectiveness of unsupervised, home-based exercises in patients with subacute LBP.
Methods
Study design
A quantitative, experimental, randomised controlled trial design was used in this research. The groups were matched by gender and age, and the participants were blinded in terms of group allocation. The effectiveness of a four-week home-based exercise programme was compared to a control group at posttest. Both groups were followed for a further four weeks after the intervention period to assess the effectiveness of the exercise programme. Thus, the whole experiment was conducted over an eight-week period. At the end of the study, the control group was offered the same protocol that was given to the exercise intervention group. The study protocol was approved by the University of Johannesburg's Faculty of Health Sciences Research Ethics Committee (South Africa) (REC-241112-035).
Participants and selection criteria
The research population consisted of male and female adults (18-65 years) who suffered from subacute LBP. Prospective participants were given an information letter explaining the research project and an informed consent form which was signed by the participants indicating their willingness to take part in the research project. Participants completed a medical history questionnaire to determine if they met the inclusion criteria: namely, that participants had to be between the ages of 18 and 65 years, and suffered from non-specific LBP [11 for more than four weeks but less than three months. All participants had to be able to communicate in English. The diagnosis was determined by the researcher. The participant's medical history and exclusion criteria were also examined by the researcher The exclusion criteria included spinal surgery within the last year, a positive straight leg raise test indicative of referred pain, cauda equina syndrome, any contraindications to exercise, and symptoms such as the following: swelling and acute inflammation, the inability to perform activities of daily living, bowel or bladder dysfunctions, rheumatoid arthritis, metabolic or malignant bone diseases, pregnancy, and uncontrolled cardiovascular disease.
A sample of 20 individuals (35.8±15.6 years; 11 males and 9 females) with subacute LBP who either responded to advertisements or heard about the study through family, friends or acquaintances were included. The participants were randomly assigned to either a control group (CG) or a home-based exercise group (HG) and, apart from gender, no attempt was made to match the two groups. Participants were blinded in terms of group allocation while the researcher was not.
Study procedure
Participants completed two questionnaires: a standard 10 cm Visual Analog Scale for Pain (VASP) and the Modified Oswestry LBP Disability Questionnaire (Oswestry). The validity and reliability of these two questionnaires have been previously established. [12,13] Both the VASP and the Oswestry questionnaires were completed prior to the intervention (pretest), at the end of the four-week intervention (post-test), and at the end of eight weeks (follow-up test). In addition, the VASP was completed by both groups at the end of each of the four intervention weeks to monitor the pain level of each participant.
Intervention
The HG received an exercise programme and were requested to perform the exercises three times a week for four weeks. The HG participants received one explanation and demonstration of the exercises and a printed copy of the exercise programme (with written instructions and pictures). The CG participants took part in all the testing procedures, but they did not receive any intervention other than the advice to rest. Both groups provided feedback (via SMS or email) on a weekly basis regarding their VASP.
The current study utilised aerobic warm-up exercises, static stretches and resistance exercises from previous research studies (Table 1). [14-19] The resistance exercises changed in Week Three and Week Four to allow for progression. Each week the exercises were also progressed by the researcher (as indicated in the programme) in terms of either repetitions, sets, duration, or type of exercise. The researcher also had to be satisfied that the participants were able tolerate the progressions (based on weekly VASP feedback).
Data analysis
The research used descriptive statistics. Tests of normality (Shapiro-Wilk test) were conducted for each of the dependant variables. Based on the results of the Shapiro-Wilk test, non-parametric statistical tests were performed, including the Mann-Whitney U test, Friedman test, and the Wilcoxon Signed Rank Test. The Mann-Whitney U test was used to test differences between two independent groups. The Friedman test was used to assess the participants at three or more points in time. The Wilcoxon Signed Rank test was used to assess participants on two occasions under two different conditions.
Furthermore, inter-group and intra-group effect sizes were calculated using Cohen's d formula. The level of confidence for statistical significance was set at 95% (p ≤ 0.05) and the level of clinical significance was set at a "large effect size" (d>0.8).
Results
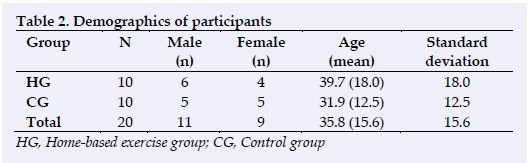
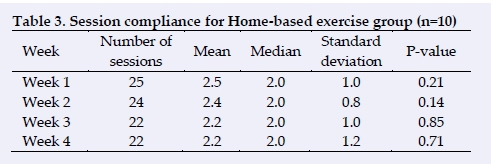
As previously mentioned, the CG consisted of five males and five females and the HG consisted of six males and four females (Table 2). All 20 participants who started the study completed it. The HG completed an average of 2.5±1 sessions in the first week, 2.4±0.8 sessions in the second week, 2.2±1 sessions in the third week and 2.2±1.2 sessions in the final week of the intervention period. (Table 3).
At pretest the CG Oswestry score was 15.4±10.5% (two outliers were present; however, they were included in the statistical analysis) and HG Oswestry score was 15.8±4.7%. The CG VASP was 4.7±1.4 cm and the HG VASP was 4.2±1.8 cm. The corresponding post-test Oswestry scores were as follows: CG 4.6±2.4% and HG 1.5±1.6%, while the VASP results were CG 4.6±2.4 cm and HG 1.5±1.6 cm. At the four-week follow-up the CG Oswestry score was 16.2±13.2% and the HG Oswestry score was 8.0±7.7%. The four-week follow-up VASP score for the CG was 4.0±2.3 cm and the HG VASP score at the four-week follow-up was 1.1±1.1 cm. The increase in Oswestry scores from the post-test to the four-week follow-up test could have been due to the non-compliance of the exercise programme post study. While not significant on a statistical level, "rest' may have played a role in the reduction of Oswestry scores for the CG when comparing pretest to posttest results. (Tables 5 and 6).
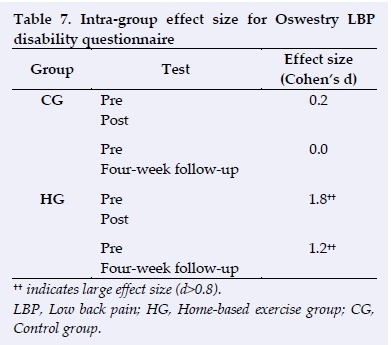
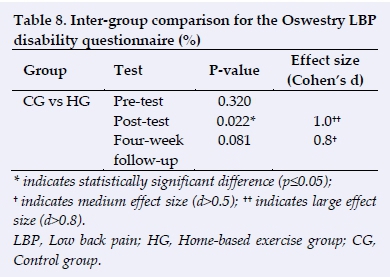
Thus following the four-week, home-based exercise intervention, there were significant improvements in the Oswestry scores for the HG from the pre- to the post-test (p=0.005), as well as between the pretest and four-week follow-up test (p=0.021). No significant improvements were observed in the CG between the pre- and post-test (p=0.095) or between pretest and the four-week follow-up test (p=0.766) for Oswestry. Large effect sizes were observed in the HG for the Oswestry between pre- and post-test (d=1.8) and between the pretest and the four-week follow-up test (d=1.2). There was also a large effect size (d=1.0) when the HG was compared to the CG at post-test, and a medium effect size (d=0.8) at the four-week follow-up test (Tables 7 and 8).
Significant improvements also occurred in the HG VASP from pre to post-test (p=0.011) and between the pretest and the four-week follow-up test (p=0.005). Large effect sizes were observed for the HG between the pre and the post-test (d=1.6) and between the pretest and the four-week follow-up test (d=2.1). There were also large effect sizes when comparing the CG to the HG at post-test (d=1.5) and between the two groups at the four-week follow-up test (d=1.6) (Tables 9 and 10).
Discussion
The current study investigated the effectiveness of home-based exercise in treating subacute LBP. The statistically significant improvements in both pain and functional ability reported following four weeks of home-based exercises for participants with subacute LBP were supported clinically by the large effect sizes. In addition, these benefits lasted for at least four weeks after the conclusion of the intervention period, as confirmed by the follow-up test. Thus it may be deduced that the home-based exercise programme was a clinically beneficial treatment in the short term (i.e. over eight weeks) for subacute LBP. This may provide an effective alternative treatment for subacute LBP patients who cannot afford or struggle to access supervised rehabilitation.
In accordance with previous studies, the intervention programme was designed to strengthen the abdominals, paraspinal muscles, gluteal muscles, hamstrings and multifidi as well as to stretch the erector spinae, hamstrings, hip flexors and quadratus lumborum muscles. [14-19]
The current study used a four-week intervention period which compared favourably with that of other studies between four and eight weeks long. [18,19] This study requested that the patients perform the exercises three times per week. This compared favourably with previous studies that implemented exercise programmes between two and five times a week. [18,19] Although the compliance of the participants in the current study was favourable, full adherence to the requests of three sessions a week were not followed by all the participants as indicated in Table 4.
The hypothesis behind the programme was that by stabilising the pelvic and lumbar region through the implementation of strength exercises that focused on the transverse abdominis, multifidus, hamstrings, gluteal muscles and back extensors pain would decrease, and functional ability improve. Furthermore, by combining strength exercises with flexibility that focused on stretching and mobilising the erector spinae, hamstrings, hip flexors and quadratus lumborum muscles, a more successful result would be achieved. The aerobic component of the programme was implemented for a warm-up, as well as to improve lower limb and pelvic stability dynamically.
Limitations
Numerous limitations are present in the current study such as, the small sample size, absence of a long-term follow-up assessment, the reduced accuracy of extrapolating the data to rural communities in South Africa, lack of education regarding spinal care and correct posture [20], lack of psychological consideration and treatment [21], and levels of activity and fitness prior to the study. The reasoning for over- or under-compliance towards the home programme was also not requested.
In future studies, researchers should attempt to determine the effects of a longer intervention period, as well as to monitor the longer-term benefits (six months to two years) exercise has on reducing subacute low back pain. Monitoring the recurrence of low back pain will be beneficial to fully understanding the prolonged effects exercise rehabilitation has on low back pain. It will be useful if future research also investigates the effects of exercise on subacute low back pain in different age groups, different socio-economic backgrounds and work environments (e.g. blue- vs. white-collar workers). Furthermore, future studies should look at the prevalence of low back pain in rural settings, as well as approaching low back pain from a multidimensional perspective where the following factors are taken into consideration: modifiable (emotions, behaviours, loading demands, lifestyles etc.), non-modifiable (social, economic, culture, history and genetics), neuroimmune, endocrine and comorbidity health factors [22].
Conclusion
The results of the present study confirmed that a four-week home-based exercise programme is effective in improving function and reducing pain in patients with subacute LBP. However, since the study was limited by a small sample size, future studies using larger samples are needed to confirm the present study's findings.
Acknowledgements
The authors wish to thank the participants for their contribution to this study.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no conflicts of interest to declare.
References
1. McIntosh G, Hall H. Low back pain (acute). BMJ Clin Evid 2011; pii:1102. [PMCID: PMC3217769] [ Links ]
2. Hayden JA, van Tulder MW, Malmivaara AV, et al. Meta-analysis: exercise therapy for nonspecific low back pain. Ann Intern Med 2005;142(9):765-775. [doi: 10.7326/0003-4819-142-9200505030-00013] [ Links ]
3. Smidt N, de Vet HC, Bouter LM, et al. Effectiveness of exercise therapy: A best-evidence summary of systematic reviews. Aust J Physiother 2005; 51(2):71-85. [doi: 10.1016/s0004-9514(05)70036-2] [ Links ]
4. Linton SJ, van Tulder MW. Preventive interventions for back and neck pain problems: what is the evidence? Spine J 2001; 26(7):778-787. [doi: 10.1097/00007632-200104010-00019] [ Links ]
5. van Tulder M, Malmivaara A, Esmail R, et al. Exercise therapy for low back pain: a systematic review within the framework of the Cochrane collaboration back review group. Spine J 2000; 25(21):2784-2796. [doi: 10.1097/00007632-200011010-00011] [ Links ]
6. Steffens D, Maher CG, Pereira LS, et al. Prevention of low back pain: a systematic review and meta-analysis. JAMA Intern Med 2016; 176(2):199-208. [doi: 10.1001/jamainternmed.2015.7431] [ Links ]
7. Statistics South Africa. Poverty trends in South Africa: an examination of absolute poverty between 2006 and 2015. Report No. 03-10-062015. Pretoria: Statistics South Africa, 2014:26,71. http://www.statssa.gov.za/publications/Report-03-10-062015 (accessed 19 November 2018) [ Links ]
8. Saner J, Kool J, Sieben JM, et al. A tailored exercise program versus general exercise for a subgroup of patients with low back pain and movement control impairment: A randomised controlled trial with one-year follow-up. Man Ther 2015; 20(5):672-679. [doi: 10.1016/j.math.2015.02.005] [ Links ]
9. Haufe S, Wiechmann K, Stein L, et al. Low-dose, non-supervised, health insurance-initiated exercise for the treatment and prevention of chronic low back pain employees. Results from a randomized controlled trial. PLoS One 2017; 12(6): e0178585. [doi: 10.1371/journal.pone.0178585] [ Links ]
10. Miyamoto GC, Lin CC, Cabral CM, et al. Cost-effectiveness of exercise therapy in the treatment of non-specific neck pain and low back pain: a systematic review with meta-analysis. Br J Sports Med 2018; p.ii: bjsports-2017-098765. [doi: 10.1136/bjsports-2017-098765] [ Links ]
11. Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet 2017; 389(10070):736-747. [doi: 10.1016/S0140-6736(16)30970-9] [ Links ]
12. Boonstra AM, Schiphorst Preuper HR, Reneman MF, et al. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res 2008;31(2):165-169. [doi: 10.1097/MRR.0b013e3282fc0f93] [ Links ]
13. Davidson M, Keating JL. A comparison of five low back disability questionnaires: reliability and responsiveness. Phys Ther 2002;82(1):8-24. [doi: 10.1093/ptj/82.1.8] [ Links ]
14. Cho KH, Beom JW, Lee TS, et al. Trunk muscles strength as a risk factor for nonspecific low back pain: a pilot study. Ann Rehabil Med 2014; 38(2):234-240. [doi:10.5535/arm.2014.38.2.234] [ Links ]
15. Saper RB, Sherman KJ, Delitto A, et al. Yoga vs. physical therapy vs. education for chronic low back pain in predominantly minority populations: study protocol for a randomized controlled trial. Trials 2014;15(1):67. [doi: 10.1186/1745-6215-15-67] [ Links ]
16. Chen HM, Wang HH, Chen CH, et al. Effectiveness of a stretching exercise programme on low back pain and exercise self-efficacy among nurses in Taiwan: a randomized clinical trial. Pain Manag Nurs 2014;15(1):283-291. [doi: 10.1016/j.pmn.2012.10.003] [ Links ]
17. Shnayderman I, Katz-Leurer M. An aerobic walking programme versus muscle strengthening programme for chronic low back pain: A randomized controlled trial. Clin Rehabil 2013;27(3):207-214. [doi: 10.1177/0269215512453353] [ Links ]
18. Stankovic A, Lazovic M, Kocic M, et al. Lumbar stabilisation exercises in addition to strengthening and stretching exercises reduce pain and increase function in patients with chronic low back pain: randomized clinical open-label study. Turk J Phys Med Rehab 2012; 58(3):177-183. [doi: 10.4274/tftr.22438] [ Links ]
19. Masharawi Y, Nadaf N. The effect of non-weight bearing group-exercising on females with non-specific chronic low back pain: a randomized single blind controlled pilot study. J Back Musculoskelet Rehabil 2013; 26(4):353-359. [doi: 10.3233/BMR-130391] [ Links ]
20. Dankaerts W, O'Sullivan P, Burnett A,et al . Differences in sitting postures are associated with nonspecific chronic low back pain disorders when patients are subclassified. Spine J 2006; 31(6):698-704. [doi: 10.1097/01.brs.0000203532. 76925.d2] [ Links ]
21. O'Keeffe M, George SZ, O'Sullivan PB, Psychosocial factors in low back pain: letting go of our misconceptions can help management. Br J Sports Med 2018; pii: bjsports-2018-099816. [doi:10.1136/bj sports-2018-099816] [ Links ]
22. O'Sullivan P, Caneiro JP, O'Keeffe M, et al. Unraveling the complexity of low back pain. J Orthop Sports Phys Ther 2016;46(11):932-937. [doi:10.2519/jospt.2016.0609] Buell JL, Franks R, Ransone J, et al. National Athletic Trainers' Association position statement: evaluation of dietary supplements for performance nutrition. J Athl Train 2013;48(1):124-136. [doi: 10.4085/1062-6050-48.1.16] [ Links ]
 Correspondence:
Correspondence:
M J Lumb
michaeljameslumb@gmail.com














