Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Sports Medicine
On-line version ISSN 2078-516X
Print version ISSN 1015-5163
SA J. Sports Med. vol.28 n.1 Bloemfontein 2016
http://dx.doi.org/10.17159/2078-516x/2016/v28i1a465
ORIGINAL RESEARCH
CASE STUDY
An atypical presentation of myositis ossificans
M BultheelI, II; JH KirbyIII; JT ViljoenIV; PL ViviersV
IMD, M Med (Sports Med); Campus Health Service and the Centre for Human Performances Sciences, Stellenbosch University, South Africa
IIMD, M Med (Sports Med); Department of Physical Medicine and Rehabilitation, Catholic University of Leuven, Belgium
IIIMBChB, MSc (Sports Med); Campus Health Service and the Centre for Human Performances Sciences, Stellenbosch University, South Africa
IVBSc (Physio), MPhil (Exercise Sci); Campus Health Service and the Centre for Human Performances Sciences, Stellenbosch University, South Africa
VMBChB, M Med Sc, MSc (Sports Med), FACSM; Campus Health Service and the Centre for Human Performances Sciences, Stellenbosch University, South Africa
ABSTRACT
In the following case study an atypical presentation of myositis ossificans (MO) in the superior anterolateral thigh of a young soccer player is discussed. This case demonstrates that MO can present without obvious history of trauma, which makes the diagnosis of this condition more challenging. The most important differential diagnosis is malignant osteosarcoma or soft-tissue sarcoma, which usually presents without trauma. Additionally both pathologies typically occur in the same population.
Keywords: case report, ossification, osteosarcoma
Myositis ossificans (MO) is defined as a localised formation of heterotopic non-neoplastic bone in muscle or soft tissue.[1] It usually presents as a complication of traumatic muscle injury and thus is most likely to develop in high-risk sites of injury such as the quadriceps and biceps muscle. It is most readily seen in adolescent and young adult men as a result of sport-related blunt trauma.
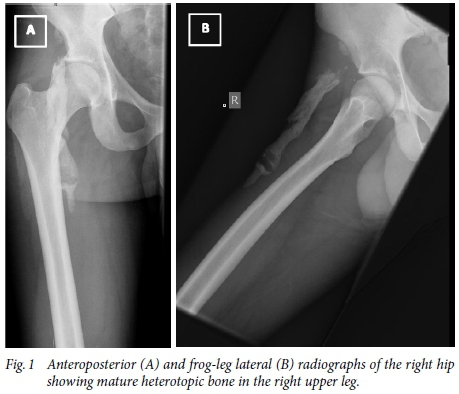
A 21-year-old male recreational soccer player presents with a three-week history of right hip pain during kicking, sprinting and climbing stairs, preceded by eight months of stiffness. He noticed a hard lump in the upper thigh on which he unsuccessfully performed self-facilitated massage to release the area. He reports previous minor muscle strains in the area but no direct blunt trauma. There is no pain at rest or at night, nor does he report weight loss, night sweating or generalised malaise. Moreover, his medical and family history is insignificant. Clinically, this appears to be a healthy young man with normal gait and full range of motion of the hips. However, resisted hip flexion and abduction as well as the Thomas test reproduce pain. The nodule feels firm and is not tender upon palpation. Ultrasound demonstrates a hyper reflective peripheral rim suggesting calcification of the nodule. Two areas of ossification were reported following plain radiographs, one in the soft tissues posterior to the hip joint and the other over the lateral aspect of the superior acetabular rim (see Figure 1, A & B). Furthermore, areas of central lucency were identified and no connection was found between the mass and the femur. Considering the patient's history and mature aspect of the lesion upon imaging the diagnosis of end stage MO was made. Conservative treatment with physiotherapy failed to resolve the patient's symptoms and there was functional impairment with exercise, hence the calcification was removed surgically. Since then the patient has recovered to his previous level of participation in sport, however he does occasionally report pain and stiffness during high intensity sporting activities. To date (20 months post-surgery) no reappearance has been reported.
Discussion
MO is a known complication of muscle injury where calcification proceeds to ossification in muscle or soft tissue.[2] The exact aetiology is still unknown and several theories have been proposed. It has been hypothesised that rapidly proliferating mesenchymal cells, in the presence of localised tissue anoxia, ultimately differentiate into bone-forming cells and osteoblasts, producing ectopic bone and cartilage. In addition, muscle damage leads to prostaglandin synthesis, which attracts inflammatory cells to the site of injury, fostering the formation of MO.[3] An alternative theory is that mechanical injury can cause the osteoblast-containing periosteum to be pushed into the muscle which results in ectopic calcification.[4,5]
The incidence of MO after muscle contusion has not been well documented, but has been reported to be 9-17%. The occurrence is thought to be related to the severity of injury and is higher in males 30-40 years old.[6] The physical signs suggesting impending MO are localised tenderness and swelling, a palpable mass and loss of flexibility.[5]
Differential diagnosis may include a muscle haematoma, abscess and malignant primary or secondary soft tissue tumours. The most important differential diagnosis is extra-skeletal osteosarcoma, which has similar clinical and pathological characteristics.[6-8]
Various imaging techniques are available to evaluate the presence and progression of MO including musculoskeletal ultrasound (MSU), radiography, computed tomography, magnetic resonance imaging and skeletal scintigraphy. It is important to note that the radiologic features evolve as the lesion matures. MSU is a sensitive modality and may have the capability to detect early phases of MO approximately two weeks prior to radiographic evidence.[5] MSU can also monitor progression throughout the course of MO where peripheral rim-like calcification and sheet-like or lamellar calcification are very suggestive of MO. Calcification that is more centrally located is nonspecific, and may be seen with a soft tissue tumour. MSU can also be used to guide surgical removal of a lesion as total reflection of the MSU beam from the peripheral rim indicates that the lesion is mature. Conversely reappearance is more likely if a lesion is removed when it is metabolically active (not fully reflective).[6,9] The most important diagnostic feature on X-rays is the zoning pattern of peripheral maturation, indicating that the lesion is benign. The finding of this radiopenic centre and the absence of connection to the adjacent bone, the so called cleavage plane, further aids in the differentiation of MO from malignant lesions of bone.[9]
Management of early MO consists of rest, ice, compression and elevation followed by physiotherapy to regain strength, proprioception and flexibility. During this stage aggressive stretching should be avoided.[3] Indomethacin, a non-steroidal antiinflammatory has been proposed to inhibit further formation of new bone.[7] The natural history of MO is of benign nature and it may even regress after several months. Surgical intervention is thus only indicated when there is functional limitation, persistence of pain after the inflammatory phase, neurovascular compromise or severe disfigurement. It should only be performed on mature heterotopic bone. However even during the mature phase there is a risk of reoccurrence following resection.[7]
Conclusion
This case report demonstrates that MO can have an insidious onset without a clear history of blunt traumatic muscle injury. Therefore diagnosis can be more challenging, especially when differentiating MO from a malignant lesion such as an osteosarcoma.
Understanding the pathophysiological development of MO, namely its typical peripheral to central ossification process is imperative in making the correct diagnosis. Treatment is usually conservative and involves physiotherapy and anti-inflammatories. Large lesions with functional limitations may be managed surgically.
Funding: None.
Conflict of interest: None.
References
1. Gindele A, Schwamborn D, Tsironis K, et al. Myositis ossificans traumatica in young children: report of three case and review of literature. Pediatr Radiol 2000;30:451-459. [http://dx.doi.org/10.1007/s002479900168] [ Links ]
2. Yazici M, Etensel B, Gürsoy H, et al. Nontraumatic myositis ossificans with an unusual location: case report. J Pediatr Surg 2002;1621-1622. [http://dx.doi.org/10.1053/jpsu.2002.36196] PMID: 12407551. [ Links ]
3. Busell P, Coco V, Notarnicola A, et al. Shock waves in the treatment of post- traumatic myositis ossificans. Ultrasound Med Biol 2010;36:397-409. [http://dx.doi.org/10.1016/j.ultrasmedbio.2009.11.007] [ Links ]
4. Kim SW, Choi JH. Myositis ossificans in psoas muscle after lumbar spine fracture. Spine 2009;34:367-370. [http://dx.doi.org/10.1097/BRS.0b013e31819b30bf] [ Links ]
5. King, JB. Post-traumatic ectopic calcification in the muscles of athletes: a review. Br J Sports Med 1998;32:287-290. [http://dx.doi.org/10.1136/bjsm.32.4.287] PMID: 986397. [ Links ]
6. Yochum A, Reckelhoff K, Kaeser M. Ultrasonography and radiography to identify early post traumatic myosistis ossificans in an 18-year-old male: a case report. J Chiropr Med 2015;13:134-138. [http://dx.doi.org/10.1016/j.jcm.2014.06.004] [ Links ]
7. Lau J, Hartin CW jr, Ozgediz DE. Myositis ossificans requires multiple diagnostic modalities. J Pediatr Surg 2012;47:1763-1766. [http://dx.doi.org/10.1016/j.jpedsurg.2012.05.009] PMID: 22974621. [ Links ]
8. El Bardouni A, Boufettal M, Zouaidia F, et al. Non-traumatic myositis ossificans circumscripta: A diagnosis trap. J Clin Orthop Trauma 2014;5:261-265. [http://dx.doi.org/10.1016/j.jcot.2014.09.005] PMID: 25983509. [ Links ]
9. Parikh J, Hyare H, Saifuddin A. The imaging features of post-traumatic myositis ossificans, with emphasis on MRI. Clin Radiol 2002;57:1058-1066. [http://dx.doi.org/10.1053/crad.2002.1120] PMID: 12475528. [ Links ]
 Correspondence:
Correspondence:
PL Viviers
plv@sun.ac.za














