Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Agricultural Extension
On-line version ISSN 2413-3221
Print version ISSN 0301-603X
S Afr. Jnl. Agric. Ext. vol.42 n.2 Pretoria Dec. 2014
A comparative analysis of two land reform models: The Mashishimale Farm Management Model and the Nkumbuleni Strategic Partnership Model, South Africa
Terblanché S. E.I; Stevens J. B.II; Sekgota M. G.III
ISenior lecturer, Dept of Agricultural Economics, Extension and Rural Development, University of Pretoria
IISenior lecturer, Dept of Agricultural Economics, Extension and Rural Development, University of Pretoria
IIIMSc Student, Dept of Agricultural Economics, Extension and Rural Development, University of Pretoria
ABSTRACT
The Sustainable Restitution Support - South Africa (SRS-SA) program aimed at the development of a post-settlement support model that could be used to support beneficiaries of land reform in South Africa, especially those who received the land through restitution. The two land restitution claims were identified namely Mashishimale in the Limpopo Province and Nkumbuleni in KwaZulu Natal Province in South Africa. The main objective of the study is to determine the essential elements of two post-settlement support models to successfully implement and manage land reform projects in a sustainable manner namely: Mashishimale Farm Management Model (FMM) and Nkumbuleni Strategic Partnership Model (SPM). The data was collected through meetings and interviews with different stakeholders or role players.
The study reveals that the following actions are essential for the successful post-settlement to restitution farms:
- The execution of baseline study (survey) to determine the socio-economic situation in a community (beneficiaries).
- The appointment of an independent project facilitator/coordinator to ensure effective and efficient communication.
- A well-defined management structure and the appointment of a knowledgeable, skilful and experienced farm manager(s) or strategic partner.
- The development of a business plan for the farm with the support of professional agriculturist.
- The identification of qualified professional extension advisor to provide advice and guidance to the manager(s) or strategic partner.
- Appointment of a mentor to guide advice and train the manager(s) or strategic partner.
- Financial support to manage the farm (Grants; Comprehensive Agricultural Support Program; financial institutions and specifically the Land Bank).
Keywords: Land reform, farm management, strategic partnerships, support services (extension)
1. INTRODUCTION AND BACKGROUND TO LAND REFORM IN SOUTH
Land reform is a process of transferring the land from one owner to another through certain legislation that governs the entire process. According to Oxford dictionary, the word "reform" means to make better by removal of imperfections, faults or errors (The Concise Oxford Dictionary, 1979). Land reform in South Africa is regarded as part of the Reconstruction and Development Programme (RDP) and as such it has a contributory factor towards the national reconciliation, growth and development in the country. The program commenced in 1994 immediately after the first and new democratic government came into power. Land reform in South Africa is a lawful process that is being guided by policies (Department of Land Affairs, 1997). The Land Reform Programme is structured around three pillars:
- Land Redistribution - aims to create equality by providing black people with access to land for either productive or residential purposes;
- Land Restitution - aims to return land to black South Africans who were forcibly removed from their land by the apartheid system; and
- Land Tenure - aims to provide labour tenures with secure tenure (ownership or occupancy rights) of land (DLA, 1997).
According to Monama (2006), many farms that were used to contribute to critical food supply in the country and that have been transferred to land claim beneficiaries in Limpopo Province have collapsed due to a lack of a financial support from government, lack of farming knowledge and skills, and more worse, internal squabbles and fighting. According to Monama (2006), in some instances, land is bought but the farm machinery required for farming is excluded. The Department of Agriculture (Agriculture, Forestry and Fisheries) and Department of Land Affairs (Rural Development and Land Reform) realized that there was a need to establish a different program called Land and Agrarian Reform Project (LARP). Government came up with a new approach namely "Profit-sharing partnership", which was seen to improve the success of land reform programs. The new approach to land reform encourages the commercial farmers to establish partnership with the land reform beneficiaries in South Africa (Hofstatter, 2010).
In 2005 the Chief Land Claims Commissioner requested the Centre for Land Related Regional and Development of Law and Policy at the University of Pretoria, and the Centre for Property Studies in New Bruwnswick, Canada to develop an evidence based settlement and support strategy for land agrarian reform in South Africa to assist people regaining land rights through the restitution process. Two land restitution claims were identified namely Mashishimale in the Limpopo Province and Nkumbuleni in KwaZulu Natal Province in South Africa.
This paper draws data from two related case studies undertaken by the authors to determine the essential elements of two post-settlement support models to successfully implement and manage sustainable land reform projects: namely Mashishimale farm management model and Nkumbuleni strategic partnership model.
The following specific objectives were set for the study:
- To describe two different models with regard to land restitution; and
- To determine the factors that led to failures and/or successes in each model.
2. LITERATURE REVIEW ON LAND REFORM WITH SPECIAL REFERENCE TO RESTITUTION CLAIMS AND AFTER CARE SUPPORT
2.1 Post-settlement support models for the South African situation
Although there are several models of post-settlement support such as equity schemes and mentorship programs, this research study focused on the use of a Farm Management Model and a Strategic Partnership Model.
Farm Management Model
There are many definitions and descriptions of farm management, but they all focus on achieving the set objectives of a farming enterprise or business. "Farm management can be described as the rational decision-making to achieve the objectives of the particular farming enterprise" (van Reenen and Marais, 1992: 2). According to van Reenen and Marais (1992), a farm manager should concentrate on formulation of the farm business objectives and making decisions that will also help to achieve those objectives. "Farm Management can be regarded as the process whereby a farmer plans, organizes, coordinates and controls all the production factors of a farm business, namely land, labour and capital, in order to attain certain objectives such as maximum profit growth, sustainability and an improved standard of living" (Van Zyl, Kirsten, Coetzee & Blignaut, 1999: 3).
Some of the land claim communities find it important and necessary to employ knowledgeable and skilful farm managers to assist them to manage the farms on their behalf. However, it does not seem to be so much helpful. According to Zvomuya (2005), the farm was bought and handed over to the community but three years after transferring of land and rights the farm was none operational and none productive. The outsiders blame the community for letting the farm to fall into ruins while the community blamed the Trust for theft and mismanagement; on the other side the Trust is blaming the managers for being white and sabotaging government's effort and squandering the funds while the managers are blaming the chief for misusing the funds. Zvomuya (2005: 62) reported "Today, it's a ghost farm; its fields overgrown with khaki bush and deep erosion dongas disfiguring its once beautiful landscape".
Strategic Partnership Model
The Oxford dictionary (1979) defines partner as "person associated with others in business of which he shares risks and profits" This definition is giving a clearer background of most of the definitions that were given by different authors or writers. According to the Department of Land Affairs (1997: 39), "Private sector initiatives in land reform are partnerships between recipients of the settlement/Land Acquisition Grant and owners of private business, which broaden the base of land ownership, offer security of tenure and raise incomes of the grantees. Eweg (2006) suggest that a few important key elements should be considered for a successful partnership in farming business, which are also discussed by van Reenen et al (1995) as explained below:
(i) The partnership agreement should be well defined and be in a written form;
(ii) The contributions of each partner should be well defined and recorded for future reference; and
(iii)The method of remuneration should be clearly defined to avoid confusions and argument when is time to share the profit made or loss incurred.
Several examples exist of relatively successful joint ventures between land owners whose lands/farms are under claims and beneficiaries:
- Raats (2008) reported about a Mr Spencer Drake who who decided to go for a partnership with the beneficiaries of Magoebaskloof farms. He shared his knowledge, skills and expertise with the beneficiaries. He was later joined by his neighbouring farmer, who trained and mentors the beneficiaries running their business on timber treatment.
- According to Hofstatter (2007) two farmers who sold their farms to the land reform beneficiaries of Marulaneng at Hoedspruit in Limpopo Province formed a joint venture with the beneficiaries. They were quoted by Hofstatter (2007) whereby stating: ''We wanted to sell some of our land to the government for this purpose, but without compromising on agricultural productivity." They helped the community in identifying and registering the beneficiaries and the formation of the Communal Property Association (CPA). The partnership was established to last for a period of ten years, after which the CPA will buy them out and run the company as community property (Hofstatter, 2007).
- Phillips of Farmers Weekly (2010) reported that Ngcolosi Community at Kranskop in KwaZulu Natal has been given their land back through restitution in 2005 and decided to form the Ngcolosi Community Trust (NCT) to manage its properties. The NCT decided to form a farm management company, Ithuba Agriculture. The general manager of Ithuba Agriculture who is spearheading the development, improvement and production is suggesting the following tips that could bring about success on post-settlement of restitution farms:-
- Partner with proven farming companies;
- Employ experienced farm management team while developing the available staff through training and mentorship;
- Maximise outputs through effective agricultural practices;
- Make use of the experience of the successful land reform farms to set up a new farming ventures; and
- Good record keeping and accounting practices could be used when applying for bridging finance.
- The Transvaal Suiker Beperk (TSB) Strategic Partnership Model
TSB is one of the biggest sugar-producing companies in South Africa. It is situated on the east of Malelane town in the Nkomazi District of Mpumalanga Province. Some of its farms (notably sugar cane farms) were part of the biggest restitution claims of Tenbosch in Mpumalanga Province. The Siphumulele Community (formed Siphumelele Tenbosch Trust) and the Ingwenyama Community (formed Ingwenyama Simhulu Trust) are two of the communities that have benefited from the Tenbosch restitution. They realized that they lack proper knowledge and skills on the management of sugarcane farming. With this in mind they entered into a partnership agreement with TSB through their respective Trusts. TSB entered into a partnership with the Trusts through its Agricultural services company known as Shubombo Agricultural Services (Chiyoka, 2009). The partnership agreement was clearly defined whereby each partner's contribution was clearly stipulated.
3. METHODOLOGY
According to the introductory discussion it is clear that a large number of land reform projects have failed in South Africa because of poor governance structures and with little or no post-settlement support or after care services to the beneficiaries. The following contributory factors have been identified and outlined by Kressirer and Ngomane (2006) in post land reform areas of Mpumalanga and Limpopo Provinces namely:-
- Limited technical farming expertise;
- Poor physical infrastructure;
- Poor access to finance;
- Limited farm management expertise; and
- Poor organizational arrangements and leadership skills
In 2005 the Chief Land Claims Commissioner requested the Centre for Land Related Regional and Development of Law and Policy at the University of Pretoria, and the Centre for Property Studies in New Bruwnswick, Canada to develop an evidence based settlement and support strategy for land agrarian reform in South Africa to assist people regaining land rights through the restitution process. Two land restitution claims were identified namely Mashishimale in the Limpopo Province and Nkumbuleni in KwaZulu Natal Province in South Africa.
This paper draws data from two related case studies undertaken by the authors to determine the essential elements of two post-settlement support models to successfully implement and manage sustainable land reform projects: namely Mashishimale farm management model and Nkumbuleni strategic partnership model.
A semi structured questionnaire was used to collect data at the several meetings held with the representatives of the Community Property Association; Community Trust; Beneficiaries (community members); The Tribal Authorities (TA); Regional Land Claim Commission; Department of Land Affairs; Department of Agriculture (provincial level); Women Clubs; Consultants and other institutions of the Mashishimale and Nkumbuleni communities. A number of specific key questions were developed beforehand to ensure that relevant information was collected. This was followed by a focus group discussion held with the CPA and Trust members to understand the challenges being faced.
4. CASE STUDY 1: THE MASHISHIMALE COMMUNITY PROPERTY ASSOCIATION (CPA) -< THE FARM MANAGEMENT MODEL
In 1999 the Mashishimale Community lodged a claim with the Limpopo Regional Land Claims Commission (RLCC) in Limpopo in compliance with section 11(1) and 2(1) of the Restitution of Land Rights Act of 1994 for 35 350 hectares of land. The claimant community was comprised of approximately 1 885 households who could trace their ancestry to the original inhabitants, plus 99 other households who had migrated into to area after the forced removals (SRS-SA, 2008). The owners of the farms were willing to sell 16 353 hectares back to the community, while the remaining 18 997 hectares are still in the process of being transferred. The 16 353.2 hectares of land were valued at a total of R148 620 000 (SRS-SA, 2008). The Community Property Association (CPA) was established in 2004.
4.1 Structure and responsibilities of Mashishimale CPA
According to White Paper on South African Land Policy, a CPA could be defined as, "Legal body through which members of disadvantaged and poor communities may collectively acquire, hold and manage property in terms of a written constitution" (Department of Land Affairs, 1997: 51). The CPA must draw up the constitution which will help to provide good governance and management of the properties. The Mashishimale CPA structure comprises of the following positions:-
- Chairperson;
- Deputy Chairperson;
- Secretary;
- Deputy Secretary;
- Treasurer;
- Three (3) additional members;
- Two (2) Ex-officio members (TA member and the Chief).
Responsibilities of the Mashishimale CPA
- Manage all the properties/ projects on behalf of the community and report progress and challenges;
- Manage the finance and prepare all the necessary reports;
- Continue with claiming of the remaining lands, still outstanding;
- Arrange and organise community and stakeholder meetings;
- Represent the community in all other meetings;
- It is the decision making body;
- To create jobs;
- It serves as a link between the community and other stakeholders;
- Appointment of knowledgeable, skilful and experienced CEO and farm managers; and
- Establish a Finance Committee and two (2) steering committees.
The perceived success of the Mashishimale CPA
- The salvaging of the falling citrus farm by appointing a knowledgeable farm manager.
- Appointed a skilful manager to revive the Game Ranch;
- Apply successfully for a production loan from an Exporters Association;
- Communication channels and cooperation with the community is smooth and there is trust among all role players; and
- Working relationship with the TA, RLCC and community is a success.
Challenges and problems identified/ experienced after settlement
- The former land owner moved out of the farm without notice, the commissioner was informed but did not react. The farm was three (3) months without maintenance;
- There were no fertilizer, pesticides, pumps were not working, and irrigation could not take place.
- No funds to pay farm workers their monthly salaries;
- The community cattle owners (farmers) wanted land for grazing and herbalists wanted permission to enter the farm to collect medicinal plants for their medicines;
- The post settlement payment was delayed and as such affecting the operational program and payment of farm workers; and
- CPA members did not receive any training on farm management.
Financial management and support
- There is a Steering Committee responsible for the finances and to report to the CPA;
- The CEO keeps all financial records ( purchases and payments), however there is no actual financial system in place; and
- The CPA is not prepared to sign any documents and also to stand for any surety for financial loans. Due to frustration, the CEO and Game Ranch farm manager have stand for surety for the loans in their private capacity.
- Interim Business Plan
- An interim business plan was developed with the assistance of the Project facilitator/coordinator and Agricultural specialists from University of Pretoria;
- A knowledgeable and skilful farm manager was recruited to manage the citrus farm; and
- Capital investment for Croc Ranch in order to operate effectively is estimated at R4 160 000.
4.2 Meeting with community stakeholders and structures (roles, needs and expectations)
a) Meeting with the Tribal Authority (TA) Chief and the Council
- They helped to lodge the land claim;
- The Chief help to transport committee members to meetings; and
- Encouraging community and business people to make financial contributions in the community.
b) Meeting with business people (women)
- There is a group of people in the community that is going all the way out to make a living out of small businesses. However selling the same products within the community where they stay, competing against one another.
- The women and men making handcrafts need urgent support for the establishment of a site at the entrance gate to the Kruger National Park.
- They use social grants to buy materials and other products to either make handcrafts or to resell them to their fellow community members.
c) Meeting with community elders
- The community elders were crucial in the identification of the significant areas; and
- They also help in the formation of the family trees.
d) Meeting with religious people
- It was noted that there was only one church member who attended the meeting. He indicated that it was very difficult to raise funds within the community which is already in the deep end of poverty.
e) Meeting with social clubs
- The social clubs include the Burial Societies; and
- The social club, Stokvel society, wherein members of that society contribute R100.00 as a monthly subscription.
f) Meeting with traditional healers
- Traditional healers made it clear that they want access to the farms to collect medicinal plants (muti);
- They would like to perform rituals for their ancestors who were buried in those farms;
- They indicated that they can collect medicinal plants from certain areas but they experience transport problems;
- Medicines can only be prepared on an open wood fire and as such there is a need to have access to fire wood from the farms; and
- As a group they are interested to grow medicinal plants in a nursery.
g) Meeting with cattle owners
- They need the land for ploughing and plant crops and the need of land for grazing for their animals (cattle, goats, sheep, etc.); and
- There is no grazing management system in place and there are no fences that could help them to control grazing of animals.
4.3 Meeting with project facilitator / coordinator
SRS-SA appointed Womiwu Rural Development which in turn appointed an independent consultant as a project facilitator/coordinator to assist the CPA. The facilitaor was coordinating the project functions such as training (capacity building on governance, management and finance), building and maintaining good working relationship with the stakeholders.
i) Profile of the Projectfacilitator/Coordinator
- Agriculturally educated with farming experience.
- A person with trainer/mentor knowledge and experience.
- An experienced person with skills to work with people.
ii) Specific role and functions
The Project Facilitator/Coordinator became part of the project by being an independent person to make a difference, render support to the project and make it successful and to coordinate all the SRS-SA activities.
iii) Observations made by the Project Facilitator/Coordinator
- The community is aware of what is happening on the farm;
- The community identified other needs that need to be addressed;
- The role of the Chief in the CPA should not be underestimated;
- The RLCC did not really do what was expected and promised to the community through the CPA, always giving excuses; and
- The financial challenges of the CPA were not addressed.
iv) Lessons learnt by the Project Facilitator/Coordinator
- The RLCC made promises and create expectations that seldom fulfil;
- Community members have divergent views and perspectives on land use which must be catered for accordingly;
- The aims and objectives of each project must be communicated properly to the community;
- There is no feedback from government officials or structures to the broader communities;
- Not all the deliverables are attainable (need to be more flexible);
- The FMM is replicable; it could be used at other places; and
- The beneficiaries have insufficient funds, or no funds and expertise to manage the farm effectively and efficiently.
4.4 Meeting with executive of farm
a. Chief Executive Officer (CEO)
i) Management responsibilities
- The CEO is the senior manager of the entire Mashishimale farm business. All managers of different sections report to him;
- He is responsible for ensuring good financial management, keep all purchasing, payments and other financial transaction records.
- The management of the farm business meet regularly with the Steering Committee (Finance) of the CPA;
ii) Identified problem areas
- No job description as CEO, making it difficult to execute functions properly;
- No specific meeting schedule or plan with his managers (ad hoc);
- No actual financial system in place; and
- CPA is not prepared to sign documents and stand surety for financial loans.
iii) Recommendations by the CEO
- The development of job descriptions demands urgent attention;
- CPA is responsible to apply for loans not the managers/workers; and
- CPA members need to be trained on the basic principles of all business activities.
b. The Game Ranch Manager
i) Management responsibilities
- The Game Ranch manager resigned as CPA member when appointed as Game Ranch manager.
- He does not have any previous experience in terms of game farming but his willingness and commitment to the business is his drive;
- 27 staff members under his supervision and they meet once a week;
- Managers' report directly to the CEO however there is no specific meeting program or schedule;
- He attended an intensive six weeks Veld Rangers Training program in the Kruger National Park and was nominated as the best trainee;
- CPA meets with the community on quarterly basis. Meetings are well attended and young people form part of the meetings; and
- A Development Committee was established responsible for development aspects specifically for the development of the youth.
ii) Identified problem areas
- Meetings with CPA are frustrating especially with finance, decisions making is slow and committee members has very little knowledge about the farm as a business;
- Staff members do not have job descriptions; and
- Casual workers received a salary which is below the minimum wage as described in the Labour Act.
iii) Recommendations by the Game Ranch Manager
- The development of job descriptions are essential;
- A structured meeting program between the CEO and two managers needs to be implemented;
- There is a need to establish a nursery to grow medicinal plants for the traditional healers;
- Meet with SANPARKS to discuss the possibility to open a shop at the Phalaborwa gate to the Kruger National Park; and
- The development of a cultural village as part of a full eco-tourism project needs urgent discussion and planning.
c. Mogotle Citrus Farm and Pack House Manager
i) Management responsibilities
- 32 full-time staff members under his supervision.
- Ensure that staff members have to be registered in terms of the necessary legislation;
- Farm workers must sign worker's contract with the management as soon as possible;
- Workers' Committee which meet once a week to discuss training needs, tasks, reporting and challenges/problems;
- The manager is providing the in-house (in-service) training; and
- Responsible for all citrus farming operational activities.
ii) Identified problem areas
- The manager is not involved in the long-term strategic planning of the farming business;
- Meetings with the CEO are not official, ineffective and unstructured;
- The manager recruits people from the community to work on the farm, but they were not interested.
- Experience serious financial problems to manage the farm and pack house effectively;
- 10 essential vacancies at the farm, which need urgent attention;
- The manager needs to join farmers' study group to improve his knowledge and skills;
- The development of a Workplace Skills Plan for all staff members;
- There is no career path and job description for the staff members;
- There is insufficient irrigation water available at the farm; and
- The dilapidated pack house and irrigation system need urgent repair.
iii) Recommendations by the Mogotle Citrus Farm and Pack House Manager
- He has farming experience but needs support in a form of a mentor;
- He should stay on the farm to be able to manage all activities effectively and efficiently;
- The development of job descriptions and workplace skills plans needs urgent attention; and
- A structured meeting program should be developed and implemented between the CEO and two farm managers.
4.5 Post settlement support
The following role players played or could play a role in the post settlement support of the Mashishimale community.
- Agricultural Extension services
Local municipality officers are non-existence.
- Limpopo PDA
CPA is not familiar with the extension services from the extension officers of Limpopo Department of Agriculture.
- Community organisations
There are no Community Based Organisations that are rendering support services except the Traditional Council and traditional healers.
- SANPARKS
SANPARKS has promised to supply game for the game farming, but nothing happened.
- Other Government Departments
The local structures such as Local Government are only coming when invited and talk about Integrated Development Program but there is absolutely no delivery at all.
- Phalaborwa Mining Company
Phalaborwa Mining Company has promised to adopt the farm, but nothing happened.
4.6 Job creation
- The CPA is looking forward to bring about development and improvement of the people of Mashishimale by upgrading of school buildings, roads, clinics, houses for the poor and also to save money for an education trust.
- The game farm, citrus farm and lodge have opened job opportunities for the Ba-Phalaborwa community.
4.7 Communication channels or systems
The CPA had a very strong and reliable communication pattern namely, quarterly mass meetings with the community while urgent matters are sent to the community through the radio and notices or the community announcer.
4.8 Specific training needs
The broader community requires training in production management and procedures, marketing strategies, leadership, project management, financial management, and conflict management.
5. CASE STUDY 2: THE NKUMBULENI COMMUNITY TRUST - STRATEGIC PARTNERSHIP MODEL
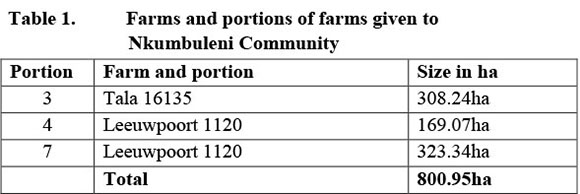
The Nkumbuleni Community consists of 250 households who were removed from the land but only 211 households were verified whereby approximately 20% is headed by women (SRS-SA, 2008). The community established the Nkumbleni Community Trust (CT) three years before the land could be transferred to them. The community made claims for a number of farms but they could only be given the following few farms because the other farms were disputed by the current owners.
5.1 Structure and responsibilities of community trust
Structure of Community Trust (CT)
This legal body is entrusted to hold and manage the land or properties of the groups of people or communities on their behalves. The Trust does not have its own constitution and it is currently using the Trust Deed to guide its functioning. The structure of the CT consists of the following portfolios:-
- Chairperson;
- Deputy Chairperson;
- Secretary;
- Deputy Secretary;
- Treasurer;
- Public Relations' Officer;
- Chaplain; and
- Additional members (6)
Responsibilities of the CT
- The main role of the CT is to manage the property on behalf of the community;
- The CT has to ensure that the project progresses well;
- The CT also strengthened the relationship and cooperation with the partners and other stakeholders;
- The chieftainship is also often informed about all the development and related activities at the projects;
- This is the decision-making body that is also responsible for the organisation of meetings and dissemination of information; and
- It is also responsible for the settlement of outstanding claims on behalf of the community.
Perceived success of the CT
- The CT has managed to attract and appoint the strategic partner;
- It is following up on the remaining land claims;
- The strategic partner successfully brought the failing farm to its normal production state.
- The strategic partner model is a pillar of strength and success for the farm;
- There is a good working relationship with all the role players;
- The communication channels with the community is smooth and it is bringing about strong support and trust to the CT.
Challenges and problems identified after settlement
- The election of the CT members was not democratically done;
- The community members are staying far away from the farms;
- There is high rate of theft, especially farm equipment;
- The farm demanded an absolute resuscitation with special attention to the deteriorated citrus production;
- The project need farm machinery such as tractors;
- The main challenge to address is a lack of funding and the knowledge about possible funding.
- The Trust has been struggling to access funding from the government but all in vain;
- The strategic partner injected R2 800 000.00 which has rescued the project;
- Members of the Trust have other commitments outside the project, and as such they compromise their time to fulfil their commitments at work and for the project to be successful;
- Promises made by the Department of Agriculture and Conservation with regard to funding have not materialised; and
- The CT is planning to select members from the community (especially the youth) to be trained as farm managers.
Financial management and support
- The Restitution Discretion Grants (R633 000) and Settlement Planning Grants (R303 840) for 211 households were applied for, but unsuccessful to date;
- A submission was made for additional funds (R2 400 000). The submission bounced back because of a problem in the structure;
- A grant to the value of approximately R632 449 has been paid to the Trust and this money was paid back to the strategic partner;
- There is no settlement plan and funding to manage the farms available;
- Nothing has materialized (within 9 months) with regard to the application for CASP funds;
- The only positive aspect is that the Department of Agriculture and Conservation identified the project as one of its flagships, but the support is rated zero;
- The irrigation system was upgraded with funds made available by the strategic partner;
- It became evident that the Department did not use the business plan to develop a CASP financial plan;
- The strategic partner clearly indicated his frustration with the current situation;
- A business company was established and consists of five directors. It is however important that all Trust members and the community must clearly understand the role of the business company; and
- The project coordinator and Agricultural specialists from University of Pretoria, assisted the Community Trust to develop the Interim Business Plan.
5.2 Meeting with Tribal Authority
The Chiefs helped and supported the motion to lodge the land claim with the RLCC. The elders of the community were allowed by the chieftainship to identify the historical areas that would serve as the evidence during the lodging of the land claim. The Chiefs and Indunas do not usually attend the meetings but they are kept abreast about the entire development on the projects.
5.3 Meeting with project facilitator/coordinator
A project facilitator/coordinator was appointed to assist the community and the Trust to coordinate the project functions. The project coordinator is playing a vital role in the current success of the project.
i) Profile of the Project facilitator/coordinator
- Agriculturally educated with farming experience;
- Project facilitator/coordinator has trainer/mentor knowledge and experience; and
- She has experience and skills to work with people.
ii) Specific role and functions of the Projectfacilitator/coordinator
- The project facilitator/coordinator became part of the project to make a difference, render support to the project and make it successful; and
- To coordinate all SRS-SA activities at the project level (detailed functions of the project facilitator/coordinator: Box 1)
iii) Observations made by the project facilitator/coordinator
- Elections of the Community Trust members were not democratically done;
- The CT committee is focusing only on one item, the farming business and citrus enterprise. Other enterprises are falling apart;
- Beneficiaries are staying far away from the farming project, which becomes an expensive exercise when people are supposed to go to work on daily basis;
- The CT committee is sometimes delaying issues which need urgent attention, which ultimately result in more damage to the project;
- In some instances the beneficiaries are taking advantage of the partnership and relax where it is not necessary to do so;
- The expenditure is not explained in detail and cash flow statement is too difficult for the beneficiaries to understand;
- The RLCC is contributing towards the failure of the project. It does not really guide people in terms of the necessary support that they need. They only come to the meeting when invited and stand to defend their superiors and their offices thereof;
- Government is only dealing with prescriptive documentations without proper assistance to the beneficiaries, there is nothing happening;
- The training that was done by the consultants was very much incompatible with the training needs of the community (and the language used during training was very difficult to be understood by the trainees/trustees);
- There is a dire need for the youth to be trained in different categories of governance especially training of facilitation skills; and
- It is the intension of the CT that all new farming projects will be implemented and managed by CT themselves and with the support from the community. The intension is therefore not to appoint a strategic partner for new projects.
iv) Lessons learnt by the Projectfacilitator/coordinator
- The community that does not have the relevant knowledge and suitable skills to provide any physical contributions to the project ("beggars are not choosers");
- RLCC must release the appropriate funds in time. Too many excuses by the government officials defending their superiors;
- Government must provide initial training to the trustees in time;
- Farmers must be monitored by government before they leave or transfer their farms to the claimant beneficiaries or community; and
- Government must help to create and promote a good relationship between the former farm owner and the claimant community.
5.4 Meeting with strategic partner
Nkumbuleni formed a partnership with a knowledgeable, skilful and experienced neighbouring farmer. The following are the view points of the strategic partner on this partnership:
i) Establishing the partnership
The strategic partner offered two (2) possible ventures to the CT and the communities namely:
a) The community lease the farm to him; or
b) The farm is managed together as a joint venture.
The CT and the community decided to manage the farm together and form a partnership on the 50:50 bases and a legal contract was drawn and signed by both parties for a period of ten (10) years.
ii) Investments invested by the strategic partner
The strategic partner made his farming knowledge, management advice, tractors, equipment and transport available and invested more than R 2 800 000 in cash into the project. His main objective is to ensure that the Citrus farm must become the most successful farm in KwaZulu Natal Province.
iii) Factors strengthening the partnership
A positive and cooperative relationship has developed between the partners and they trust each other. Trustees have been trained by the strategic partner in business management and to be able to take over the business in the future.
iv) Stumbling blocks affecting the partnership negatively
The Government department's promises financial support - but very little has materialized. The strategic partner is currently responsible for the running cost of the farming operation. He has to take a bigger share in the farming business and the community perceived it very negatively. There was a rumour that one of the families want to withdraw from the partnership. It has been noticed that there is a lack of willingness among the trust members and broader community to learn and it is a known fact that an unwilling person can never be empowered.
v) The role of the stakeholders
The RLCC did attend meetings without making any positive contributions. No services were provided by the Extension service of the Provincial Department of Agriculture. The strategic partner makes use of private consultants to advise them on technical farming issues.
vi) The importance of communication
The strategic partner emphasizes the good communication between himself and the trustees as critical and it does exist. It is further the trustees' responsibility to communicate effectively with the broader community.
vii) Additional aspects affecting the success of the partnership
- The CT represents the community and their communication with the community is critical;
- The project facilitator/coordinator is a necessity to the project. She made things happened. She played a vital role and supported the strategic partner and the CT to build a relationship of understanding and trust;
- The strategic partner's motto in life is: "how much can I make for other people";
- The success of a partnership depends on a relationship, it is like a marriage;
- Both partners must have a love for farming;
- Mutual trust between the partners (including the community) is essential; and
- It was not always possible to keep to the Interim Business Plan, but it did give clear directions and an essential element of any farming operation.
5.5 The interim business plan for Nkumbuleni CT
Agricultural specialists from University of Pretoria in close cooperation with the Strategic Partner and the CT developed an Interim Business Plan for the citrus farming enterprise. The project facilitator/coordinator was responsible for the communication of the plan to the broader Nkumbuleni Community. The Interim Business Plan addresses specific day to day needs and activities of the farming enterprise such as financial and production management, marketing management, and human resource management. The Interim Business Plan was followed by the Strategic Plan which was also developed by the specialists from University of Pretoria in cooperation with the Strategic Partner and the CT.
5.6 Post settlement support services
The following role players played a role in the post settlement support of the Nkumbuleni community:
a) Agricultural extension services
The Trust members are uncertain about the role that the division of Agricultural Extension can play to support them in their farming activities.
b) KwaZulu Department of Agriculture and Conservation
- An official from the Department of Agriculture and Conservation is attending meetings with the CT and the community;
- An application for CASP funds has been made but after a period of nine (9) months nothing has materialised; and
- A delegation from the Trust should meet with senior management from the Department to clear all possible stumbling blocks as soon as possible.
c) Other Government Departments
- Department of Land Affairs (Rural Development and Land Reform) through The Regional Land Claims Commission has been coordinating the land claim for the community of Nkumbuleni;
- The RLCC is visiting the project and give advices where possible and necessary. They also attend to the CT and community monthly meetings especially when invited; and
- It has been noted by the CT that the release of funding is completely difficult and delaying. The delayed payment to the previous farm owner and/or the new owner(s) of the farms has been experienced as a serious factor responsible for the degradation of the farms. The RLCC assisted the CT in drawing up the terms and conditions of agreement with the strategic partner.
d) Commodity organisations
- Citrus Growers Association (CGA)
No support was received from the CGA. The CT expected direct support from CGA hence they are supporting other citrus growers in the country
- South African Sugar Association (SASA)
CT could not identify any support from South African Sugar Association.
5.7 Training and capacity building
The community and the CT have not received any training either about governance or management of the farming business from government. There is no work place skills plan developed for the farm workers to build their capacity and skills. The Community requires training in production management and procedures, marketing strategies, leadership, project management, financial management, and conflict management.
5.8 Job creation
There were no specific jobs created except those that were for the people to work on the farm. However, it was mentioned that the farm is far away from the community and as such it is expensive for them to travel to the farm on daily basis. The Trust is planning to select some members of the community to be trained as managers, especially the youth. It does not have any development programme that is in place and functional.
5.9 Communication channels
The project coordinator communicates with the Trust members regularly through meetings. Trust members often invite the community for information and sharing of the development or progress made at the farm. The Chiefs attend the meetings whenever invited by the Trust.
6. CONCLUSION AND RECOMMENDATION
6.1 Farm Management Model: Mashishimale community
The Mashishimale Farm Management Model has a definite management structure that was responsible for various activities on the farm. Three steering committees were established to manage Ngulube lodge; Game Ranch Safaris and Mogotle Citrus farm. The financial committee is responsible to manage the finance and prepare all the necessary reports which include financial and progress reports. A bookkeeper has been appointed responsible for audit of all financial books of the farm.
An Interim Business Plan (IBP) was developed with the support of the University of Pretoria agricultural specialists in cooperation with the CPA and CEO. The Interim Business Plan covers the marketing, operational, management, human resource and financial resource plan as well as SWOT analysis of the enterprises of Croc Ranch and Mogotle Citrus farm operations. The University of Pretoria agricultural specialists with the help of project facilitator/coordinator helped CPA to develop a financial plan which included capital investment estimated at R4 160 000 for Game Ranch, while Mogotle Citrus farm requires capital investment of R1 233 700 per annum.
The Mashishimale beneficiaries received support from Citrus growers Association (CGA), even though it was on seasonal basis. Officials from the Department of Agriculture attended meetings on the farm when invited, but there was very little extension service rendered by Department of Agriculture (Provincial). SANPARKS rendered support by assisting CPA to buy clean buffalo. The Project facilitator/coordinator facilitated training (veld management, business management, and financial management) for the CPA and the Mashishimale community members.
The community was informed or invited to meetings, through the radio, written notices (that were often plugged at the busy centres such as taxi ranks and shopping centres), the councillors and the community announcers. The CPA held community mass meetings on quarterly basis whereby feedback was given and new mandates were taken. There was no communication with Department of Agriculture except when they were invited to a meeting. CPA met weekly with CEO and managers as per schedule.
6.2 Strategic Partnership Model: Nkumbuleni community
The Nkumbuleni Community Trust (CT) has appointed a strategic partner which together with Nkumbileni CT formed a company consisting of five (5) directors aimed to manage the farm as a business. There was no specific structure implemented at farm level. A legal contract is in place for a period of ten (10) years.
An Interim Business Plan was developed with the support of the University of Pretoria in cooperation with the CT, the Strategic Partner and the farm manager. The Interim Business Plan included the upgrading of the irrigation system, a pack house, development of additional 10 ha of citrus and 100 ha sugarcane. The financial plan included the upgrading of 80ha irrigation system (R1 3000 000), pack house (R500 000), development of 10ha citrus (R600 000) and 100ha of sugar cane (R1 500 000). The CT has applied for CASP funding, but their application was only approved a year too late. CT has successfully applied for Restitution Discretion Grants and Settlement Planning Grants of which R632 449 was paid to them. The Strategic Partner invested R2 800 000 to rescue the citrus enterprise.
There was no support received from the CGA. An official from the KZN Provincial Department of Agriculture and Conservation was attending meetings with the CT and the community. No extension service was rendered by Department of Agriculture and Conservation. The Project facilitator/coordinator facilitated training (capacity building on governance, human resource management, and finance) and helped the CT to develop good governance structure.
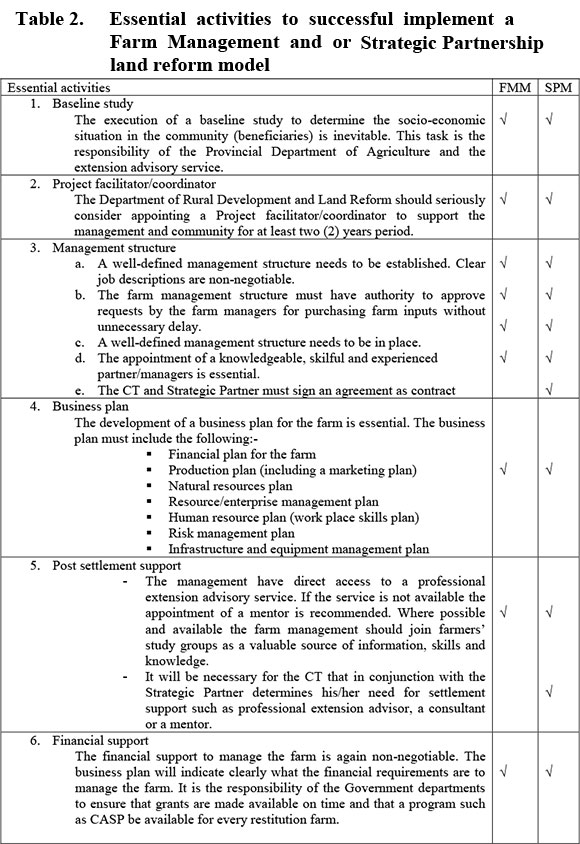
The following recommendations are made based on the study findings of the two case studies (Table 2).
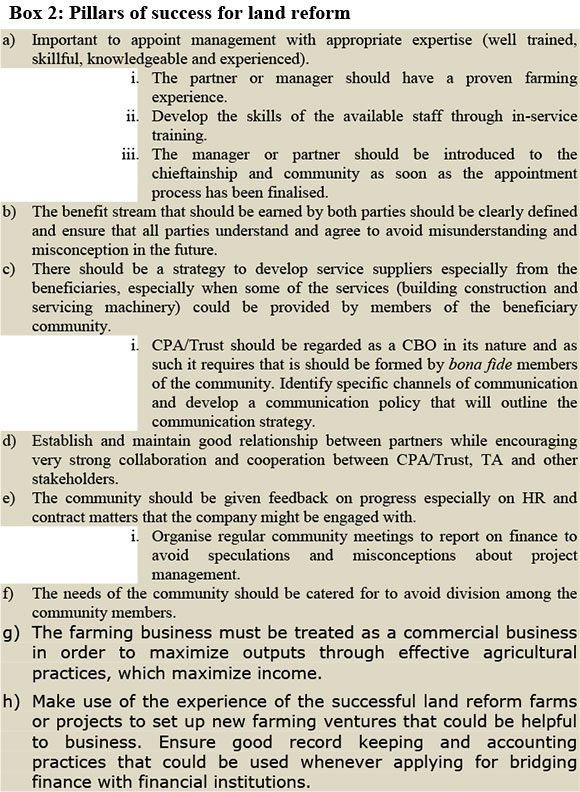
Based on authors experience over a period of three years and the findings the following pillars of success for a land reform project are recommended (Box 2):
REFERENCES
CHIYOKA, T., 2009. TSB Agriculture Beneficiaries Development Program, Personal interview. Communal Property Association Act 28 of 1996. [ Links ]
DEPARTMENT OF LAND AFFAIRS, 1997. White Paper on South African Land Policy. [ Links ]
DÜVEL, G. H., 2002. Programme and Project Development, University of Pretoria, Pretoria, Republic of South Africa [ Links ]
EWEG, M. 2006, Defining partnerships in South African agriculture, Proceedings of the 43th Conference, South African Society for Agricultural Extension. [ Links ]
FOOD AND AGRICULTURE ORGANISATION, 2007. Market-orieted farm management for trainers of extension workers, Viale delle terme di Caracalla, Rome, Italy. [ Links ]
HOFSTATTER, S., 2007."Hoedspruit land claim: coming to fruition", Farmers' Weekly, 3 August. [ Links ]
HOFSTATTER, S., 2010. "Government takes new, realistic approach on land reform", Farmers' Weekly, 5 May. [ Links ]
KRESSIRER, R., AND NGOMANE, T., 2006. Agro-based local economic development in post land reform areas of Mpumalanga and Limpopo Province, South Africa, Eschborn Juli [ Links ]
LAND CLAIMS COMMISSION, 2003. Land Restitution in South Africa: Our Achievements and Challenges. [ Links ]
MONAMA, M., 2006. "Farm casualties:beneficiaries need skills", City Press, 7 May. [ Links ]
PHILIPS, L., 2010. "A land reform success!", Farmers' Weekly, 30 July. [ Links ]
RAATS, L., 2008. "Magoebaskloof tries to survive restitution", Farmers' Weekly, 25 January. [ Links ]
THE CONCISE OXFORD DICTIONARY, 1979. Oxford University Press, Oxford, London. [ Links ]
UNIVERSITY OF PRETORIA AND SUSTAINABLE RESTITUTION SUPPORT FOR SOUTH AFRICA, 2008. Mashishimale Baseline Survey. [ Links ]
UNIVERSITY OF PRETORIA AND SUSTAINABLE RESTITUTION SUPPORT FOR SOUTH AFRICA, 2008. Mophela Baseline Survey. [ Links ]
UNIVERSITY OF PRETORIA AND SUSTAINABLE SUPPORT FOR SOUTH AFRICA, 2010. Restitution Implementation Manual: Partnership for Sustainable Pre- and Post-Settlement Support. [ Links ]
VAN REENEN, M. J. & MARAIS, A. DE K. 1992. Farm Management: Financial Planning, Analysis and Control, JL Van Schaik, Pretoria, Republic of South Africa. [ Links ]
VAN REENEN, M. J., MARAIS, A. DE K. & NEL, P. S., 1995. Farm Management: Financing, Investment and Human Resource Management, JL Van Schaik, Pretoria, Republic of South Afscrica. [ Links ]
VAN ZYL, J., KIRSTEN, J. F., COETZEE, G.K. & BLIGNAUT, C. S., 1999. Finance and Farmers: A Financial Management Guide for Farmers, The Agricultural Segment of The Standard Bank of South Africa Limited, Johannesburg, Republic of South Africa. [ Links ]
ZVOMUYA, F., 2005. "Mandela's farm in ruins", Farmers' Weekly, 6 May. [ Links ]
 Correspondence:
Correspondence:
Dr S E Terblanché
Phone: +27 12 4204623
Fax: +27 12 420 4958
fanie.terblanche@up.ac.za
Dr J B Stevens
Phone: +27 12 4203249
Fax: +27 12 420 4958
joe.stevens@up.ac.za














