Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Agricultural Extension
On-line version ISSN 2413-3221
Print version ISSN 0301-603X
S Afr. Jnl. Agric. Ext. vol.42 n.2 Pretoria Dec. 2014
Creating youth employment through modern beekeeping: Case study of selected youth trained in Moro Local Government Kwara State, Nigeria
Yusuf S. F. G.I; Lategan F. S.II; Ayinde I. A.III
IPhD Research Fellow, Department of Agricultural Economics and Extension, University of Fort Hare, Alice Campus, Eastern Cape South Africa
IIAssociate Professor: Agricultural Economics and Extension, Department of Agricultural Economics and Extension, University of Fort Hare, Alice Campus, Eastern Cape South Africa.
IIIDepartment of Agricultural Economics and Farm Management, University of Agriculture, Abeokuta Ogun State, Nigeria
ABSTRACT
The study evaluated the impact of training offered on beekeeping by Fayolam Farms in 2007 to selected youth in the Moro Local Government of Kwara State, Nigeria. The training was offered as part of a Corporate Social Responsibility (CSR) program. Structured interview schedules were used to collect data from 116 respondents who participated in the training and who were still active in beekeeping. The results showed high levels (93%) of adoption among the males relative to their female counterparts. The mean age of participants was 28.6 years, mostly (89. 65%) were married, 44.82% had junior secondary education and were predominantly (79.31%) farmers. Hive acquisition increased progressively after the training from 5 to 30 hives on average while the total revenue generated on individual aggregate was ₦ 119, 275.00 with the share of male participants as high as 63.16%. Production challenges faced by the trainees include destruction of hives by fire, pest and diseases, pilfering and absconding of bees. It is recommended that community policing should be encouraged to address pilfering. Further training should focus on areas of challenges and also research on less aggressive bee species should be carried out for introduction
Key words: Beekeeping; agribusiness, training evaluation, youth
1. BACKGROUND
Beekeeping or modern apiculture is the art and science of rearing, breeding and managing honey bee colonies in artificial hives for economic benefits (Ikediobi, Obi & Achoba, 1985; Morse, 1989; Ahmad, Joshi & Gurung, 2007). The most common species utilized for this purpose is Apis mellifera (Hymenoptera: Apidae) of which about 25 species of economic importance occur in Europe, Middle East of Asia and Africa (Segeren, 1997). A. Mellifera adansonii, a native species of West Africa, is the one most commonly used in Nigeria (Extension Research Liaison Service [ERLS], 1995). Beekeeping has evolved into a farming enterprise that involves the use of sophisticated and artificial techniques to keep honey bees for bee products such as honey, propolis, wax, pollen, bee venom and royal jelly (Ojeleye, 1999). It contributes significantly to securing sustainable livelihoods by assisting in transforming vulnerabilities into security (Ahmad et al., 2007:4). Beekeeping is also carried out by small farmers, and it is particularly suitable for under-privileged landless and lowincome, low-resource individuals and groups. According to Ahmad and Partap (2009), beekeeping requires minimal start up investment and generally yields profits within the first year of operation. In addition to the direct income from bee products, beekeeping enterprise stimulates various sectors within a society like hive carpentry, honey trading, renting and hiring of bee colonies for pollination, and other bee value addition (Chazovachii et al, 2013:127)
Beekeeping does not require large size of land nor fertile land to produce as hives can be located on poor land, on top of trees, and rocky areas.
Poverty and unemployment are a common phenomenon in Nigeria. The report of the National Bureau of Statistics (NBS) (2011) indicates that Nigerians living in poverty line rose from 68.7m to 112.5 m (63.7% rise in poverty incidence) between 2004 and 2010 while the population rose from 139.2m to 158.6m (13.9% rise in population) over the same period. The report of BGL Research and Intelligence (2012) indicates that in 2011, Nigerians ages 15-24 (37.7%) and of those between ages 25-44 (22.4%) that are willing to work cannot find jobs with the youth accounting for more than 75 percent (NBS, 2010). Over the years, government has addressed the problem with various programs, amongst which are National Directorate of Employment (NDE), the Family Support Program (FSP), Better Life for Rural Women (BLRW), the National Agricultural Land Development Agency (NALDA), Directorate for Food, Roads, and Rural Infrastructure (DFRRI), Family Economic Advancement Program (FEAP) and National Poverty Eradication Program (NAPEP) (Osinubi, 2003). However, poverty and unemployment remained unabated (Oyekanle, 2011).
1.1 Problem statement
The problem of youth unemployment is largely evident in Nigeria (Okafor, 2011). The implementation of the various programs at poverty reduction and creation of job has not focus much attention into beekeeping as an enterprise. More so, access to large acres of land in the rural area is becoming unattainable due to the tenure system of inheritance where land has been excessively fragmented. Ayinde (2011) argues that this phenomenon needs to be arrested by injecting less land-demanding farm business opportunities which are relatively easy to set up with a modest capital outlay and less-demanding administrative skills. Beekeeping therefore fit in well. Beekeeping technology is not complex and tedious, it requires a relatively small amount of time input as against crop or livestock farming, thereby making it viable for utilization in relief program (Cadwallader, Hewey, Isaza & Simsek 2011:2). It also plays an important role in sustainable agricultural development through increase in resources without changing environmental balance (Moniruzzaman & Rahman, 2009: 109). The potentiality of rebuilding and kick starting sustainable livelihood endeared it to many interest groups because of its multi beneficial benefits. It was on these bases that Fayolam Farms (FF) situated in Fala village in an effort at supporting government in poverty reduction embarked on training of youth in modern beekeeping technology. The idea behind was based on the Corporate Social Responsibility (CSR) of the company. Four years after the training, the program was assessed to determine the current position of the trainees.
2. GENERAL OBJECTIVES
The study was aimed at critical assessment of the progress ensuring capacity development and the challenges of the beekeepers trained in 2007 who had no background in modern beekeeping.
2.1 Specific objectives are:
1. To determine the socio-economic profile of the trained beekeepers.
2. To determine the adoption rate and assess the current position of the beekeepers
3. To determine the level of progress (increase in the number of hives, harvest, market accessibility, return on investment) attained by the beekeepers.
4. To determine the challenges the beekeepers are facing in the management of the apiary and suggest possible solutions.
3. RESEARCH METHODOLOGY
3.1 Description of the Study Area
Bode Saadu is the headquarters of Moro Local Government Area (MLGA), Kwara State, Nigeria. It is located on 80 56! 00. 00!!N and 4 0 47! 00.00!! E (Google Earth, 2009). It is made up of several villages amongst which are Fallah, Bielesin, Oloru and Olokiti from where the trainees were selected. The MLGA has an estimated population of about 108, 792 and an estimated total land area of about 3272 km square (NPC, 2008). It is populated by rural settlements who are majorly domiciled farmers.
3.2 Data Collection Technique
Data was collected from 116 beekeepers out of the 185 trained in 2007 representing 62.70%. There was no survey design because the respondents were already known. Semi structured interview schedule was used, which was face-validated by an extension officer of Kwara State Agricultural Development Program (KWADP). It was pre-tested using a small sample of 12 respondents from members of Beekeepers Association of Nigeria (BAN), Ilorin Branch. The internal consistency reliability estimate of the instrument was calculated using Cronbach's Coefficient (α=0. 92) and the data was analysed using Statistical Package for Social Science (SPSS) program.
4. RESULTS AND DISCUSSION
4.1 Socio-economic characteristics of Respondents
The social characteristics of the beekeepers indicate that majority (93%) are male. This finding corroborated that of Matanmi, Adesiji & Adegoke (2008) that majority (90%) of beekeepers in Nigeria are male. The mean age of the beekeepers was 28.6 years while majority (89.65%) are married and attainment of primary school educational standard and above was common to all respondents (Table 1). Given that education is an important factor in technology adoption, ability to read and write was used as one of the criteria for the selection of trainees. Age has been described as an important factor that influences the probability of adoption of new technologies (Akudugu, Guo & Dadzie, 2012:3) while education is thought to create a favourable mental attitude for acceptance of new technologies (Caswell et al., 2001).

The majority (79.31%) of the respondents were full-time farmers and engaged in crop production (Table 2). Access to farmland is one of the major problems of most new entrants into farming enterprise, but with beekeeping, land has not constituted a big challenge. Hives were located on poor uncultivable land, on top of trees, and rocky areas. This became advantages to the beekeepers as expansion was observed in the number of hives.

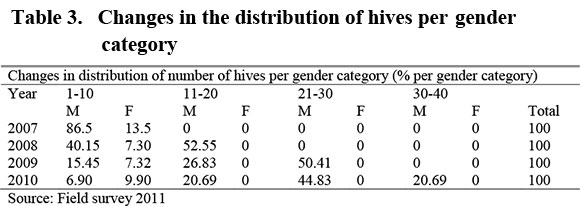
4.2 Hive Acquisition according to Gender
Table 3 indicates that male acquire more hives than their female counterpart within the period of 2007 to 2010 (Table 3). The decline in the female participation could be attributed to the specie of the bees Apis Millifera scutellata with the characteristics of aggressiveness common to the Nigeria apiary colony. As a result, further research may be needed to introduce the less aggressive species. Colony management is best carried out for this type of bees either late in the night or early in the morning to reduce attack, and these period conflicts with the female core duties to the household.
4.3 Honey Production
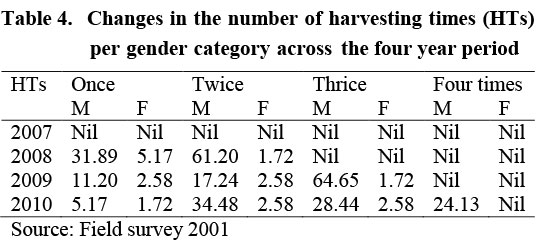
Harvesting of honey commenced in July 2008 after the initial setback of hives destruction by fire in November and December 2007. Table 4 gives a breakdown which shows the number of times of harvesting as increasing from twice to four times in a year. The increase was an indication of good apiary management and availability of nectar and pollen within a coverage distance 500 meters for the bee workers.
4.4 Quantity of Honey Harvested Per Respondents
Honey flow was good with more than five liters per hive as indicated in Table 5. This shows signs of good honey yield in the study area despite the fire destructions of some hives in 2007.

4.5 Economic Returns from Beekeeping Investment
Table 6 indicates economic returns on yield of honey from 2008 to 2010. The average yield per respondent according to gender shows clearly that male respondents performed better in terms of efficiency of honey production given the same set of input used. This translated to higher revenue to the male respondents than their female counterpart. The highest revenue (₦9, 880.00) was obtained in the month of November. On a general note, yield of honey was highest in 2010, which shows an indication that the respondents were gradually mastering the skill of beekeeping. Market accessibility was supported through the introduction of two major buyers to the beekeepers as this decreased marketing problem.
Table 7 shows the gradual increase from revenue accruing from honey harvest from 2008 to 2010. The highest revenue was obtained in 2010. The average male respondents had revenue of ₦ 75, 335.00 (63.16%) compared to the female with average of ₦ 43, 940.00 (36.84%). The female beekeepers low output was attributed to the conflicting time of apiary management and harvesting with the core household activities.

4.6 Utilization of Revenue Obtained from Beekeeping
Feedback from the trained beekeepers indicates that their livelihood had actually been transformed. Most of the beekeepers are targeting to own between 150 to 200 hives before the end of 2014, while most boast of the ability to pay the school fees and medical bill of the household. The training has proven the assertion of Ahmad and Partap (2009) that honey production through beekeeping could be a useful avenue for improving and transforming the rural economy and providing sustainable means of rural livelihood.
4.7 Challenges Faced by Respondents on the Program
The majority (89.6%) of the respondents complained of various challenges confronting their maximum production to include pests, predators and eventual absconding of bees. These factors were also identified by Workneh, Ranjitha & Ranjan (2008) and Yirga & Ftwi (2010) of the challenges confronting beekeepers. The destruction of the hives during Harmattan brought about by indiscriminate bush burning, hive destruction by wild animals (honey mongers) and pilfering by honey hunters were other problems of significant importance as described by the respondents.
5. CONCLUSION AND RECOMMENDATIONS
The evaluation of farmers and youth trained in beekeeping practices in 2007 was influenced by different factors. The minimum input requirement for training and market linkage were success factors. The challenges of hive destruction through fire outbreak, bees absconding and stealing by honey hunters notwithstanding, had proved that with the right training for the bee farmers and new entrants into the enterprise, in place, the rural economy could be transformed. This study has demonstrated that beekeeping is a proven technology, adaptable to most farming systems, low capital investment, good returns, and environmental friendly. And where access to land for cultivation is posing big challenge, beekeeping does not require such. It is therefore recommended that community policing should be encouraged to address pilfering. Further training should focus on areas of challenges and also research on less aggressive bee species should be carried out for introduction. Government should as a matter of urgency enforces the edict on indiscriminate bush burning that often destroy the biodiversity that depletes forest resources.
REFERENCES
AHMAD, F., JOSHI, S. R. & GURUNG, M, B. 2007. Beekeeping and Rural Development International Centre for Integrated Mountain Development Khumaltar, Lalitpur, Kathmandu, Nepal [ Links ]
AHMAD, F. & PARTAP, U. 2009. Improving Livelihoods through Beekeeping: knowledge partnerships and value chains for bee products and services in the Himalayas. International Centre for Integrated mountain Development, Lalipur, Nepal. Info. Sheet No 4/09 [ Links ]
AKUDUGU, M. A., GUO, E., & DADZIE, S. K. 2012 Adoption of modern agricultural production technologies by farm households in Ghana: What factors influence their decisions? Jnl of Bio., Agriculture and Healthcare Vol. 2(3), pp. 1-13. [ Links ]
AYINDE, A. F. O. 2011. Analysis of Ageing Farming Population and Agricultural Productivity among Cassava Farmers in the Rural Areas of Ogun and Ekiti States, Nigeria. Unpublished PhD Thesis, Department of Agricultural Extension and Rural Development, Federal University of Agriculture, Abeokuta, Nigeria [ Links ]
BGL RESEARCH AND INTELLIGENCE 2012. Economic Note: The Nigeria's paradox of growth amidst high poverty incidence. http://research.bglgroupng.com/Documents/EconomicNote/ECONOMIC%20NOTE%20Nigeria's%20Par adox%20of%20Growth%20amidst%20high%20incidence%20of%20Po verty.pdf Accessed 11/30/2012 [ Links ]
CADWALLADER, A., HEWEY, V., ISAZA, S., & SIMSEK, E. 2012 Supporting Urban Beekeeping Livelihood Strategies in Cape Town. Bachelor of Science Project, Worcester Polytechnic Institute, http://www.wpi.edu/Pubs/E-project/Available/E-project-122411-213327/unrestricted/CT11_Bees_Final_Report.pdf Accessed 02/13/2013 [ Links ]
CASWELL, M., FUGLIE, K., INGRAM, C., JANS S. & KASCAK C. 2001. Adoption of Agricultural production practices: Lessons learned from the US. Department of Agriculture Area Studies Project. US Department of Agriculture, Resource Economics Division, Economic Research Service, Agriculture Economic Report No. 792. Washington DC [ Links ]
CHAZOVACHII, B., CHUMA, M., MUSHUKU, A., CHIRENJE, A., CHITONGO, L & MUDYARIWA, R. 2013. Livelihood Resilient Strategies through Beekeeping in Chitanga Village, Mwenezi District, Zimbabwe. Sustainable Agriculture Research; Vol. 2 (1):124-132 [ Links ]
EXTENSION RESEARCH LIAISON SERVICE. 1995. Beekeeping technologies for Nigerian farmers. Extension Bulletin. Ahmadu Bello University. Zaria, Nigeria http://www.ifpri.org/sites/default/files/publications/nssppn29. Accessed 11/30/2012 [ Links ]
GOOGLE EARTH 2009. Google map. [ Links ] [O]. http://google-earth-pro.en.so(Earth2009)ftonic.com Accessed 02/12/ 2013.
IKEDIOBI, C. O., OBI, V. C & ACHOBA, I. A. 1985. Beekeeping and Honey Production in Nigeria. The Nigerian Field, 50: 59-70. In: Oyerinde, A. A and Ande, A.T. Distribution and impact of honey bee pests on colony development in Kwara State, Nigeria. Jnl. Agric. Soc. Sci., 5: 85-88 [ Links ]
MATANMI, B. M., ADESIJT, G. B & ADEGOKE, M. A. 2008. An analysis of activities of bee hunters and beekeepers in Oyo state Nigeria. African Jnl. of Livestock Extension 6:7- 11. [ Links ]
MONIRUZZAMAN, M & RAHMAN, M. S. 2009. Prospects of beekeeping in Bangladesh. Jnl. Bangladesh Agril. Univ. 7 (1): 109-116 [ Links ]
MORSE, R. A. 1989. History of Subsection; Beekeeping and Social insects". Bulletin Entomol. Soc. America, 35: 116-118 in Oyerinde, A.A and Ande, A.T.Distribution and impact of honey bee pests on colony development in Kwara State, Nigeria. Jnl. Agric. Soc. Sci., 5: 85-88 [ Links ]
NATIONAL BUREAU OF STATISTICS. 2011. Social Statistics in Nigeria. Abuja: The NBS Publication. [ Links ]
NATIONAL BUREAU OF STATISTICS. 2010. Statistical News: Labor Force Statistics No. 476. Abuja: The NBS Publication. [ Links ]
OJELEYE, B. 1999. Foundation of Beekeeping in the tropics. CEBRAD press Ibadan Nigeria. [ Links ]
OKAFOR, E. E. 2011. Youth unemployment and Implications for stability of democracy in Nigeria. Jnl. of Sustainable Development in Africa Vol. 13, No.1 [ Links ]
OSINUBI, T. S. 2003. Urban Poverty in Nigeria: A Case Study of Agege Area of Lagos State, Nigeria. Unpublished paper [ Links ]
OYEKANLE, T. O. 2011. Impact of Poverty Reduction Programs on Multidimensional Poverty in Rural Nigeria. Jnl. of Sustainable Development in Africa Vol. 13, No.6 [ Links ]
SEGEREN, P. 1997. Beekeeping in the tropics, Agrodok 32 publication. The Netherlands. [ Links ]
WORKNEH, A, RANJITHA P, & RANJAN, S. K. 2008. Adoption of improved box hive in Atsbi Wemberta district of Eastern zone, Tigray Region: Determinants and Financial Benefits, IPMS (Improving Productivity and Market Success) of Ethiopian Farmers Project. Working Paper. ILRI (International Livestock Research Institute), Nairobi, Kenya [ Links ]
YIRGA, G & FTWI, K. 2010. Beekeeping for Rural Development: Its Potentiality and Constraints in Eastern Tigray, Northern Ethiopia Agricultural Journal, Vol:5 (3): 201-204 [ Links ]
 Correspondence:
Correspondence:
flategan@ufh.ac.za














