Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.114 n.3 Pretoria Mar. 2024
http://dx.doi.org/10.7196/SAMJ.2024.v114i3.702
RESEARCH
Determination of anti-COVID-19 IgG and IgM seroprevalence among pregnant women at Pietersburg Hospital, Limpopo Province, South Africa
I RukashaI, II; S T S PheehaIII, IV; M R LekalakalaV, VI; P MalopeVII
IPhD; Division of Medical Microbiology, Department of Pathology, Faculty of Health Sciences, University of Limpopo, South Africa
IIPhD; Department of Medical Microbiology, National Health Laboratory Services, Polokwane, South Africa
IIIFCPath (Haem); Division of Medical Microbiology, Department of Pathology, Faculty of Health Sciences, University of Limpopo, South Africa
IVFCPath (Haem); Department of Haematology, National Health Laboratory Services, Polokwane, South Africa
VMMed (Micro); Division of Medical Microbiology, Department of Pathology, Faculty of Health Sciences, University of Limpopo, South Africa
VIMMed (Micro); Department of Medical Microbiology, National Health Laboratory Services, Polokwane, South Africa
VIIMSc; Division of Medical Microbiology, Department of Pathology, Faculty of Health Sciences, University of Limpopo, South Africa
ABSTRACT
BACKGROUND: COVID-19 has been a major public health concern globally, leading to a higher mortality rate, especially among immunosuppressed individuals, who include pregnant women, people with HIV and people living with other comorbidities. Pregnant women are considered to be a special population group owing to their specific susceptibility to some infectious diseases.
OBJECTIVE: To determine the seroprevalence of anti-SARS-CoV-2 antibodies among pregnant women attending an antenatal clinic.
METHOD: This was a descriptive cross-sectional study that tested blood samples from pregnant women who attended the antenatal clinic from March to July 2022 using the Orient Gene Biotech lateral flow immune-chromatographic assay according to manufacturer instructions. The assay detects IgM and IgG antibodies against SARS-CoV-2.
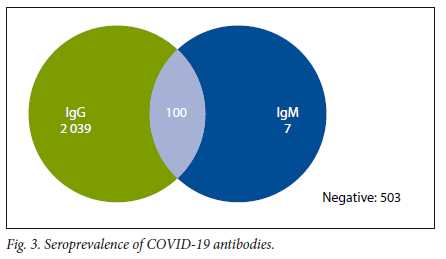
RESULTS: A total of 2 649 blood samples were tested; 2 039 (77.0%) samples tested positive for IgG, 7 (0.3%) tested positive for IgM, and 100 (3.7%) tested positive for both IgG and IgM. The study found a seroprevalence of 80.7% of IgG.
CONCLUSION: The study findings showed evidence of acute COVID-19 infection in our patient population despite the consensus that COVID-19 infection is dissipating.
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), the causative agent of COVID-19, has ravaged the world within a short period, leaving an unprecedented crisis the world has never seen before.[1.2] Globally, >468 million cases of COVID-19 were confirmed, and >6 million fatalities were reported by 20 March 2022.[3] The African continent accounted for 8 170 474 of the total cases, with 170 822 fatalities, with 3 704 784 of the confirmed cases and 99 890 fatalities being from South Africa (SA).[3,4]
COVID-19 has disproportionately impacted the lives of immuno-compromised patients, including pregnant women, people with immunodeficiency disorders and those with comorbidities such as hypertension and diabetes.[5] Pregnant women are considered a special population group due to the general physiological immunosuppression that characterises pregnancy.[6,7] During pregnancy, there is a natural physiological alteration of immunity and the cardiopulmonary system that may be affected by a wide variety of viruses, including SARS-CoV-2.[6,7] Studies reported a two-fold increase[8] in admission rates to the intensive care unit and a 1.3-fold increase[9] in maternal death in pregnant women with COVID-19 compared with those without the disease.
Understanding the epidemiology of SARS-CoV-2 infection is essential to inform future planning and management of the ongoing COVID-19 pandemic.[10] Seroprevalence surveys of SARS-CoV-2 may provide a better understanding of the disease burden at a population level.[11] Repeated seroprevalence studies can be used extensively to track the COVID-19 epidemic in sub-Saharan Africa and to derive population-based prevalence estimates. The antibodies against SARS-CoV-2 can be detected in the early 4 - 8 days (lgM), middle and later stage 14 days (lgG) of COVID-19.[12] Worldwide, there is a wide variation in prevalence in antenatal clinics. In Africa, the seroprevalence was found to be 36.7%, 50% and 77%, in pregnant women in Mogadishu, Nairobi and Yaoundé, respectively.[13-15] In SA, the seroprevalence of SARS-CoV-2 infection in pregnant women was found to be between 31% and 46% in the Western Cape Town Metropolitan subdistricts,[10] while in Johannesburg, a prevalence of 64% was reported.[16] To date, seroprevalence studies have been done on small samples. Therefore, there is a need for large cohorts to ascertain the true prevalence of antibodies against SARS-CoV-2. Thus, the aim of this study was to determine the seroprevalence of IgM and IgG in pregnant women attending the antenatal clinic in Pietersburg Hospital, Limpopo Province, South Africa.
Methods
Data collection
Prospective testing of consecutive blood samples based on scheduled routine visits was done from March to July 2022 in the haematology section of the laboratory in Limpopo Province, SA. All blood samples obtained from pregnant women attending the antenatal clinic were sent to the haematology laboratory for analysis. The patients' demographic data were recorded from the laboratory request forms submitted with the samples.
The blood was tested using the COVID-19 IgG/IgM rapid test cassette, a lateral flow immune-chromatographic assay (Orient Gene Biotech, China). The test cassette is a solid-phase immune-chromatographic assay used for the qualitative and differential detection of IgG and IgM antibodies to SARS-CoV-2 in blood or plasma. Test assay was performed according to the manufacturer's instruction within 72 hours of the specimen being received in the haematology laboratory. Two trained technicians independently interpreted each result. When reading the assay, the technicians were blinded to the results of other assays as well as to each other's results. Discordant reads between technicians were arbitrated by consultation with a third technician. The test cassette contains colloidal gold conjugated to recombinant COVID-19 antigens (COVID-19 conjugates). When a specimen followed by assay buffer is added to the sample well, IgM and/or IgG antibodies, if present, bind to COVID-19 conjugates, making antigen antibodies a complex. This complex migrates through the nitrocellulose membrane by capillary action. When the complex meets the line of the corresponding immobilised antibody (anti-human IgM and/or anti-human IgG), it is trapped, forming a burgundy-coloured band that confirms a reactive test result. The absence of a coloured band in the test region indicates a non-reactive test result.
Data analysis
A total of 3 000 blood specimens were included in the study. Unique identifiers, which included national identity numbers and date of birth, were used to remove duplicate samples. A total of 310 specimens were found to be duplicates, while 41 were of unknown age and gender and therefore removed from the study (Fig. 1).
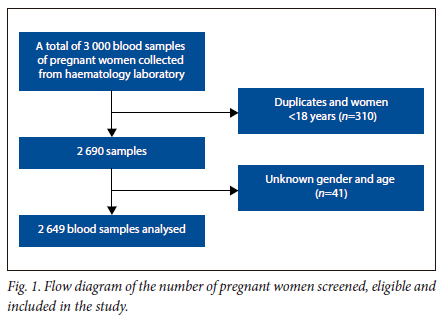
A total of 2 649 patients' data met the inclusion criteria and were included for further analysis and imported to SPSS version 27.0 (SPSS, USA). Categorical variables were described as numbers and percentages. Figures were used to show the pictorial presentation of the data. Descriptive statistics were used, and continuous variables were expressed as median and interquartile range. The frequencies of anti-COVID-19 IgG and IgM were determined and the seroprevalence was calculated. Logistic regression was used to determine the association between age and anti-COVID-19 IgG and IgM outcomes and p<0.05 was considered significant.
Ethical approval
Ethical approval was granted from the Turfloop Research Ethics Committee of the University of Limpopo (ref. no. TREC/496/2022: UG).
Results
Age distribution
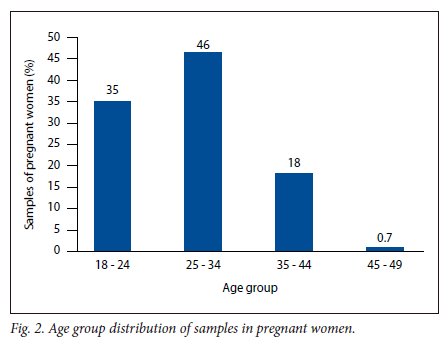
A total of 2 649 samples from pregnant women were included in the study, with a median age of 27 years, ranging from 18 to 49 years. The majority of the samples were from patients within the age group of 25 - 34 years, with 1 216 (45.9%) samples, while the lowest was within 45 - 49 years, with 18 (0.7%) (Fig. 2).
Distribution of anti-SARS-CoV-2 IgG and IgM
Of the 2 649 samples, 2 039 (77.0%) tested positive for IgG, and 7 0.3%) were positive for IgM, while 100 (3.7%) tested positive for both IgG and IgM. A total of 503 (18.9%) samples were found to be negative for both IgG/IgM (Fig. 3).
Seropositivity by age group
The data were further classified based on the seropositivity per age group. For IgG seropositivity, the age group 25 - 34 years had the majority of participants with 962 (45.0%), while the age group 45 - 49 years had the lowest seropositivity with 17 (0.8%). Based on IgM, the highest seropositivity was detected in the age group 25 - 34 years, which had 50 (47%) positive cases, followed by the age group 18 - 24 with 32 (30%), while the age group 35 - 44 had 25 (23%) positive cases. Following the distribution of IgG and IgM, the highest positive cases for both IgG and IgM were 46 (46.0%), which was detected among the age group 25 - 34 years, followed by the age group 18 - 24 with 30 (30.0%) positive cases, while the age group 35 - 44 had 24 (24.0%) positive cases. The association between seropositivity and age was not statistically significant (Table 1).
Discussion
SARS-CoV-2 has been circulating in the population over the past years and claimed many lives, including pregnant women. In SA, the most recent COVID-19 wave was driven by the Omicron variant.[17] However, the true epidemiological parameters of the pandemic are not known. Thus, the current study was conducted in the second and third quarter of 2022, a period correlating with the aftermath of the fourth wave of COVID-19 in SA. Thus, the study sought to determine COVID-19 seroprevalence in pregnant women attending the antenatal clinic at Pietersburg Hospital. To the best of our knowledge, this study contained the largest number of pregnant patient samples studied for COVID-19 seroprevalence in SA.
The study reports an IgG seroprevalence of 80.7% in pregnant women for anti-SARS-CoV-2.
The general population pooled seroprevalence in SA has been found to be lower compared with the current study, with seroprevalence estimated to be around 60% in a rural community and 73% in an urban community,[18,19] while in the whole of Africa, pooled seroprevalence was found to be lower, ranging from 0% to 63%.[20] The variation in the seroprevalence of the studies may be indicative of the time at which the studies were conducted.
The study was conducted mid-year of 2022, after the fourth wave in SA. The high seroprevalence detected in this study may be due to the cumulative infections that occurred during the first to the fourth waves of SARS-CoV-2. Furthermore, the higher seroprevalence reported in this study compared with the general population may be due to the current study including only pregnant women. Pregnant women are known to be at increased risk of acquiring viral infections, hence the high seroprevalence in this study.[6,21-24]
The study indicates positive news for Limpopo antenatal sector that herd immunity had been reached at 80.7% positivity, in a region with a 13% vaccination rate in the adult population.[25] Herd immunity is defined as resistance to the spread of an infectious disease within a population based on the pre-existing immunity of a high proportion of individuals as a result of previous infection or vaccination.[26-28] Herd immunity occurs when more than three-quarters of the community (the herd) has acquired antibodies to the disease and has become immune.[26,27]
However, the idea of herd immunity via natural infection rather than vaccination is controversial, as it is unclear how long antibodies will last and whether re-infection or reactivation of the virus can occur after the antibodies begin to lower in the body,[29] although antibody titres can wane within weeks after infection. However, the magnitude of antibody neutralisation in asymptomatic people decreases faster than in symptomatic people.[29,30] In this regard, it is with caution that we interpret herd immunity. The caution with which we should interpret herd immunity is also highlighted in the study, where 3.7% of patients were found to have both IgM and IgG. IgM in the current study indicates recent infection, while IgG represents past infection. Therefore, the presence of both antibodies can be interpreted as study participants with past infections having been re-infected, or indicating a recent primary infection.
It was interesting to note that 0.3% of the population had IgM antibodies, which represent infection within ~4 days and <14 days; IgM also lasts for about 2 weeks since the onset of symptoms.[31] The presence of IgM antibodies in this study suggests that the virus is still in circulation and being transmitted. Recent infection is still being reported, regardless of the World Health Organization newsletter of 15 September 2022 indicating that 'Pandemic's end may be near.'
It is imperative that clinicians remain vigilant and be on the lookout for COVID-19 symptoms.[3] Future studies must focus on improving this study by engaging SARS-CoV-2 genomics for comparison of the genomic sequences of the virus in various geographical locations.
Limitations
This study had several limitations. Firstly, it was conducted at a single antenatal facility within Limpopo Province, representing a limited geographical area, potentially limiting generalisability to other provinces and countries. Secondly, the study was conducted when COVID-19 restrictions were still in place in most hospital wards, prohibiting contact with patients. Thus the study was limited to being a laboratory study. Lastly, we did not collect information on comorbidities and risk factors for SARS-CoV-2 diseases such as diabetes, HIV status, obesity and socioeconomic status, which have been found to be associated with SARS-CoV-2 seropositivity in other studies in SA.[16,33]
Conclusion
In conclusion, the current study showed a high COVID-19 seroprevalence among pregnant women. The study also indicated the presence of recent infections despite the consensus that COVID-19 infection is dissipating. Furthermore, the study showed that re-infection with COVID-19 is possible, therefore herd immunity may need to be interpreted cautiously.
Declaration. None.
Acknowledgements. The authors would like to thank M Modjiadji, J Maunye and T V Makondo from the University of Limpopo, for assisting in assay testing and data capturing.
Author contributions. IR and PM conceptualised, designed, oversaw dataset administration and analysis. IR and PM wrote the first draft of the manuscript. All authors substantially contributed to manuscript revision and approved the final version for submission.
Funding. The study was fully funded by the South African Medical Research Council Self-initiated Grant awarded to IR.
Conflicts of interest. None.
References
1. Al Mansoori H, Alsaud AB, Yas H. The impact of COVID-19 on increasing the cost of labor and project price in the United Arab Emirates. Artic Int J Pharm Res Sch 2021;13(01):5069-5076. https://doi.org/10.31838/ijpr/2021.13.01.691 [ Links ]
2. Li H, Cao Y. The bright side of the COVID-19 pandemic: Public coughing weakens the overconfidence bias in non-health domains. Pers Individ Dif 2021;178(2021). https://doi.org/10.1016/j.paid.2021.110861 [ Links ]
3. World Health Organization. Coronavirus Disease (COVID-19) Situation Reports. Geneva: WHO, 2022. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed 26 November 2022). [ Links ]
4. NICD. National COVID-19 daily report. Pretoria: NICD, 2022. https://www.nicd.ac.za/diseases-a-z-index/disease-index-covid-19/surveillance-reports/national-covid-19-daily-report/ (accessed 26 November 2022). [ Links ]
5. Sanyaolu A, Okorie C, Marinkovic A, et al. Comorbidity and its impact on patients with COVID-19. SN Compr Clin Med 2020;2(8):1069-1076. https://doi.org/10.1007/s42399-020-00363-4 https://linkspringer.com/article/10.1007/s42399-020-00363-4 (accessed 26 November 2022). [ Links ]
6. Salma U. Relationship of COVID-19 with pregnancy. Taiwan J Obstet Gynecol 2021;60(3):405-411. https://doi.org/10.1016/j.tjog.2021.03.005 [ Links ]
7. Reynolds RM, Stock SJ, Denison FC, Maybin JA, Critchley HOD. Pregnancy and the SARS-COV-2 pandemic. Physiol Rev 2022;102(3):1385-1391. https://doi.org/10.1152/physrev.00003.2022 [ Links ]
8. Allotey J, Stallings E, Bonet M, et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: Living systematic review and meta-analysis. BMJ 2020;370(1):1-17. https://doi.org/10.1136/bmj.m3320 [ Links ]
9. Chmielewska B, Barratt I, Townsend R, et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: A systematic review and meta-analysis. Lancet Glob Heal 2021;9(6):759-772. https://doi.org/10.1016/S2214-109X(21)00079-6 [ Links ]
10. Tomaselli V, Ferrara P, Cantone GG, et al. The effect of laboratory-verified smoking on SARS-CoV-2 infection: Results from the Troina sero-epidemiological survey. Intern Emerg Med 2022;17(6):1617-1630. https://doi.org/10.1007/s11739-022-02975-1 [ Links ]
11. Fairlie L, Sawry S, Patel F, et al. COVID-19 in pregnancy in South Africa: Tracking the epidemic and defining the natural history. S Afr Med J 2020;110(8):729-731. https://doi.org/10.7196/SAMJ.2020.v110i9.15012 [ Links ]
12. Demey B, Daher N, François C, et al. Dynamic profile for the detection of anti-SARS-CoV-2 antibodies using four immunochromatographic assays. J Infect 2020;81(2):6-10. https://doi.org/10.1016/j.jinf.2020.04.033 [ Links ]
13. Lucinde R, Mugo D, Bottomley C, et al. Sero-surveillance for IgG to SARS-CoV-2 at antenatal care clinics in two Kenyan referral hospitals. medRxiv 2021;2021.02.05.21250735. https://doi.org/10.1101/2021.02.05.21250735 [ Links ]
14. Maryan MA, Dahie HA, Hassan NA, et al. Seroprevalence of SARS-CoV-2 virus antibodies and sociodemographic features of pregnant women in Mogadishu, Somalia: A cross-sectional survey study. BMJ Open 2022;12(6):1-11. https://doi:10.1136/bmjopen-2021-059617 [ Links ]
15. Mansuy JM, Kenfack MT, Burel S, et al. High SARS-CoV-2 IgG seroprevalence among pregnant Cameroun women 14 months after the beginning of the pandemic. Public Health 2022;(April 2020):2020-2022. https://doi.org/10.22541/au.164873379.97139041/v1 [ Links ]
16. Sawry L, Le Roux J, Wolter N, et al. High prevalence of SARS-CoV-2 antibodies in pregnant women after the second wave of infections in the inner-city of Johannesburg, Gauteng Province, South Africa. Int J Infect Dis 2022;125:241-249. https://doi.org/10.1016/j.ijid.2022.10.036 [ Links ]
17. Basu JK, Chauke L, Magoro T. Maternal mortality from COVID 19 among South African pregnant women. J Matern Neonatal Med 2021; 35(25):5932-5934. https://doi.org/10.1080/14767058.2021.1902501 [ Links ]
18. Madhi SA, Kwatra G, Myers JE, et al Population immunity and COVID-19 severity with omicron variant in South Africa. N Engl J Med 2022;386(14):1314-1326. https://doi.org/10.1056/NEJMoa2119658 [ Links ]
19. Bingham J, Cable R, Coleman C, et al. Estimates of prevalence of anti-SARS-CoV-2 antibodies among blood donors in South Africa in March 2022. Res Sq 2022. https://doi.org/10.21203/rs3.rs-1687679/v2 [ Links ]
20. Lewis HC, Ware H, Whelan M, et al. SARS-CoV-2 infection in Africa: A systematic review and meta-analysis of standardised seroprevalence studies, from January 2020 to December 2021. BMJ Glob Heal 2022;7(8):e008793. https://doi.org/10.1136/bmjgh-2022-008793 [ Links ]
21. Ferdinands JM, Rao S, Dixon BE, et al. Waning 2-dose and 3-dose effectiveness of mRNA vaccines against COVID-19-associated emergency department and urgent care encounters and hospitalisations among adults during periods of Delta and Omicron variant predominance - VISION network, 10 states, August 2021 - January 2022. Morb Mortal Weekly Rep 2022;71(7):255. https://doi.org/10.15585%2Fmmwr.mm7107e2 [ Links ]
22. Vale AJM, Fernandes ACL, Guzen FP, Pinheiro FI, de Azevedo EP, Cobucci RN. Susceptibility to COVID-19 in pregnancy, labor, and postpartum period: Immune system, vertical transmission, and breastfeeding. Front Glob Women's Heal 2021;2:8. https://doi.org/10.3389/fgwh.2021.602572 [ Links ]
23. Cervantes O, Cruz Talavera I, Every E, et al. Role of hormones in the pregnancy and sex-specific outcomes to infections with respiratory viruses. Immunol Rev 2022;308(1):123-148. https://doi.org/10.1111/imr.13078 [ Links ]
24. Vizheh M, Muhidin S, Aghajani F, et al Characteristics and outcomes of COVID-19 pneumonia in pregnancy compared with infected nonpregnant women. Int J Gynecol Obstet 2021;153(3):462-468. https://doi.org/10.1002/ijgo.13697 [ Links ]
25. Mbombi MO, Muthelo L, Mphekgwane P, et al. Prevalence of COVID-19 vaccine hesitancy in a rural setting: A case study of DIMAMO Health and Demographic Surveillance Site, Limpopo Province of South Africa. J Respir 2022;2(2):101-110. https://doi.org/10.3390/jor2020008 [ Links ]
26. Britton T, Ball F, Trapman P. A mathematical model reveals the influence of population heterogeneity on herd immunity to SARS-CoV-2. Science 2020;369(6505):846-849. https://doi.org/10.1126/science.abc6810 [ Links ]
27. Ghosh D, Jonathan A, Mersha TB. COVID-19 pandemic: The African paradox. J Glob Health 2020;10(2):1-6. https://doi.org/10.7189%2Fjogh.10.020348 [ Links ]
28. Goldblatt D. SARS-CoV-2: From herd immunity to hybrid immunity. Nat Rev Immunol 2022;22(6):333-334. https://doi.org/10.1038/s41577-022-00725-0 [ Links ]
29. Goel RR, Painter MM, Apostolidis SA, et al. mRNA vaccines induce durable immune memory to SARS-CoV-2 and variants of concern. Science 2021;374(6572). https://www.science.org/doi/10.1126/science.abm0829 (accessed 27 November 2022). [ Links ]
30. Seow J, Graham C, Merrick B, et al. Longitudinal observation and decline of neutralizing antibody responses in the three months following SARS-CoV-2 infection in humans. Nat Microbiol 2020;5(12):1598-1607. https://doi.org/10.1038/s41564-020-00813-8 [ Links ]
31. Li Z, Yi Y, Luo X, et al. Development and clinical application of a rapid IgM-IgG combined antibody test for SARS-CoV-2 infection diagnosis. J Med Virol 2020;92(9):1518-1524. https://doi.org/10.1002/jmv.25727 [ Links ]
32. George JA, Khoza S, Mayne E, et al. Sentinel seroprevalence of SARS-CoV-2 in Gauteng Province, South Africa, August - October 2020. S African Med J 2021;111(11):1078-1083. https://doi.org/10.7196/SAMJ.2021.v111i11.15669 [ Links ]
 Correspondence:
Correspondence:
I Rukasha
Ivy.rukasha@ul.ac.za
Accepted 2 December 2023














