Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.114 no.3 Pretoria mar. 2024
http://dx.doi.org/10.7196/SAMJ.2024.v114i3.1608
RESEARCH
Contribution of a bonded scholarship scheme to staffing rural health facilities
R G MacGregorI; A J RossII
IMSc, PhD; Umthombo Youth Development Foundation, Hillcrest, Durban, South Africa
IIMB ChB, FCFP; Discipline of Family Medicine, College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND: Local and international research has identified rural origin as an important reason why healthcare professionals (HCPs) work in rural areas, and in South Africa (SA) considerable effort has gone into recruiting and training rural-origin students. However, there is little information in the SA literature on where graduates supported by these initiatives work, and whether they contribute to the rural workforce long term.
OBJECTIVE: To determine the number of years that rural-origin Umthombo Youth Development Foundation (UYDF)-supported graduates of different disciplines worked at rural public healthcare facilities (PHCFs).
METHODS: A retrospective descriptive study reviewed work record data of 405 UYDF graduates, to calculate the number of years they worked at a rural PHCF. Data were analysed descriptively and presented in tables with totals and percentages.
RESULTS: Ninety percent (363/405) of UYDF-supported graduates returned to work at a rural PHCF. High percentages of social workers (85%), optometrists (80%), speech therapists, nurses (72%) and dental therapists (70%) worked for >5 years at a rural PHCF, while only 13% of audiologists, 14% of doctors, 29% of pharmacists, and 28% of dentists and occupational therapists worked at a rural PHCF for >5 years. Ten percent (42/405) of graduates did not work at a rural PHCF at all. A total of 110/124 (89%) of doctors supported by UYDF had worked at a rural PHCF, with 32% (40/124) working at a rural PHCF for >3 years. Overall, 54% of UYDF-supported graduates (219/405) worked for >3 years at a rural PHCF, and 38.5% (157/405) worked for >5 years at rural PHCFs. The majority of UYDF graduates had contributed towards long-term staffing of rural PHCFs. Lack of professional development opportunities at rural PHCFs as well as the reduced number of funded posts at rural PHCFs reduced the effectiveness of the UYDF initiative.
CONCLUSION: The UYDF Scholarship Scheme has shown that investment in rural students through a bonded scholarship can contribute to staffing rural PHCFs, as >90% of graduates worked at rural PHCFs, and for some disciplines >70% of graduates worked for >5 years at a rural PHCF. Allied HCPs worked on average for longer periods at rural PHCFs than doctors.
As in other parts of the world, a large proportion of the South African (SA) population live in rural areas, but are served by only 12% of the country's doctors and 19% of nurses.[1] There is an urgent need to find ways to staff rural healthcare facilities to ensure equitable access and provide quality services, as without staffing there can be no service.[2] The Human Resources for Health 2030 strategy has identified a need to 'revolutionise the selection and recruitment of health professional students' to overcome health workforce inequities between urban and rural areas,[3] as only ~35/1 200 SA medical graduates per annum remained in rural areas in the longer term, defined as 10 - 20 years in the Human Resources for Health Strategy 2012/13 - 2016/17.[1]
Local and international research has identified rural origin as an important reason why healthcare professionals (HCPs) work in rural areas,[4-6] and considerable effort has gone into recruiting and training rural-origin students. Factors other than rural origin, such as curricular exposure to rural healthcare[6] and a longitudinal clinical clerkship in rural areas, have also been shown to increase the number of HCPs who choose to work in rural areas.[7] However, there are other important push and pull factors, such as availability of posts, remuneration, adequate equipment, job satisfaction, promotional opportunities, feeling valued, suitable housing, jobs for spouses and schools for children, which influence the retention of rural HCPs[1,8,11] and also need to be addressed if staff are to be recruited and retained in rural areas.
In SA there have been a number of government, university and private sector initiatives aimed at addressing the staffing challenges in rural public healthcare facilities (PHCFs). These include provincial bursary programmes in KwaZulu-Natal, Limpopo, Eastern Cape and Free State provinces,[12] the Cuban collaboration programme between the SA government and the Cuban government [13] and a focus on selection of rural-origin students at universities (for example at the University of KwaZulu-Natal,[14] the Wits Initiative for Rural Health Education (WIRHE) programme run at the University of the Witwatersrand (Wits)[15] as well as the Umthombo Youth Development Foundation (UYDF) Scholarship Scheme.)[16] Although Motala[17] reported in 2019 that the graduates from Cuba were fulfilling their obligations to work in rural communities, this conclusion was based on interviewing only 20 graduates, of whom 19 had worked in rural healthcare facilities. An evaluation in 2012 of 20 graduates support by WIRHE reported that 85% (17/20) were working in rural areas.[18] Ross et al.[5] reported that in May 2014, all 185 UYDF-supported rural-origin graduates had spent time working in rural health facilities, and 71% (52/73) of those with no work-back obligations had continued to do so, as did 63% (91/145) in 2017.'161 Although these studies did not look at the duration that UYDF-supported graduates worked at rural hospitals, they concluded that the investment in rural-origin students has a positive effect on long-term staffing. A survey[11] of 135 of a possible 317 UYDF graduates in 2021 reported that 49% were working in rural healthcare facilities, the decrease being attributed to a combination of a lack of retention initiatives and funded posts at rural hospitals.
Apart from these small studies there is little information in the SA literature on where graduates supported by these initiatives work, and whether they contribute to the rural workforce long term (that is longer than the compulsory 1-year community service).
The SA landscape has changed significantly since 2018, which has impacted on the ability of UYDF to contribute to staffing of rural healthcare facilities. These include: the increasing number of UYDF graduates (488 as at March 2021), financial constraints faced by the KwaZulu-Natal Department of Health (KZN DoH)[19] and the changes in funding for tertiary education. The funding challenges faced by the KZN DoH has limited the opportunity for graduates to find employment at the hospital where they were initially selected owing to lack of funded posts, as well as the DoH no longer preferentially employing UYDF graduates in rural PHCFs as per agreement with the UYDF organisation. Since January 2018, the National Student Financial Aid Scheme (NSFAS) [20] has provided a full-cost bursary to all students whose families earn <ZAR350 000 annually (which is most of the rural students traditionally supported by UYDF), and graduates therefore no longer have a year-for-year work-back obligation to UYDF. As a result of these changes to funding of tertiary studies, the main intervention provided by UYDF since January 2018 is the provision of mentoring and limited financial support to complement their NSFAS bursary, paying for holiday work at the hospital where they were selected, as well as actively encouraging students to return to work in rural district hospitals upon graduation.
The aim of this study was to determine the number of years that rural-origin UYDF-supported graduates of different disciplines worked at rural PHCFs, thereby addressing the gap in the literature in this regard.
Methods
This was a retrospective descriptive study, which reviewed data from the UYDF database. The UYDF is a rurally based scholarship scheme, which has since 1999 been involved with the annual selection and support of 40 - 60 rural-origin students wishing to pursue a career in health sciences in priority health fields, as identified by their local participating district hospitals.[5,16] Details of all students and graduates supported by UYDF since inception of the scheme are captured in the UYDF database, and are updated annually regarding academic progress, date of graduation and graduate's place of work. This information is kept and analysed in order to track the students' progress at university and ensure that graduates meet their work-back obligations. Data for this study comprised the work records of 405 graduates from 2002 to 2020 and were analysed descriptively, and are presented in tables with totals and percentages. The number of years of work at a rural PHCF throughout the duration of their work history was calculated up to and including 2021. Rural areas are defined as having the following two characteristics: (i) sparsely populated areas in which people farm or depend on natural resources, including villages and small towns that are dispersed through these areas; and (ii) areas that include large settlements in the former homelands, which depend on migratory labour and remittances as well as government social grants for their survival, and typically have traditional land tenure systems.[21]
Results
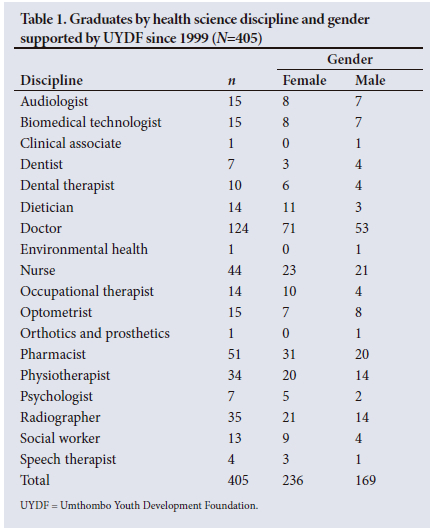
A breakdown of the 18 health science disciplines and gender of the 405 graduates included in the study is presented in Table 1. The majority of graduates were doctors (n=124, 31%), followed by pharmacists (n=51, 13%), then nurses (n=44, 11%), while females accounted for 58% of all graduates and 57% of the doctors.
In terms of understanding how many years graduates could work at a rural PHCF, Table 2 provides a breakdown by discipline of the year that graduates started work (after internship).
At the time of the study, 10% of graduates were in their first year of work, while 65% (2002 - 2017) had been working for >5 years (Table 2). Table 3 provides a breakdown of the number of years that graduates of different disciplines have worked at a rural PHCF.
In total, 363 of the 405 (90%) UYDF-supported rural-origin graduates have returned to work in rural areas and have contributed to the service delivery in these areas (Table 3). High percentages of social workers (85%), optometrists (80%), speech therapists, nurses (72%) and dental therapists (70%) have worked for >5 years at a rural PHCF. In contrast, only 13% of audiologists, 14% of doctors, 29% of pharmacists and 28% of dentists and occupational therapists have worked at a rural PHCF for >5 years, while 10% of graduates have not worked at a rural PHCF at all, including for their community service. Forty-three percent of dentists have not worked at a rural PHCF at all (Table 3). Although 57% of pharmacists worked at a rural PHCF for 1 -2 years, there is a particularly sharp decrease in the number working in rural PHCFs in years 3 - 4 (decreased from 29 to 2) (Table 3). In total, 110/124 (89%) (Table 3) doctors supported by UYDF had spent time working in rural healthcare facilities, with 32% (n=40/124) working at a rural PHCF for >3 years.
Discussion
The aim of the study was to determine the number of years that rural-origin health science graduates supported by the UYDF organisation have worked at rural PHCFs as of December 2021. There is overwhelming local and international evidence that the investment in rural health science students is one of the best options in producing health professionals willing to work in rural areas,[4-6] which has been the aim of the UYDF.[16] This study confirms that a large percentage of rural-origin graduates return to work in rural areas. However, there is limited information about the duration that rural-origin health science graduates work in rural PHCFs, which this study seeks to address.
It is encouraging to note that 54% of UYDF-supported graduates (n=219/405) worked for >3 years at rural PHCFs, and 38.5% (n=156/405) worked for >5 years at rural PHCFs. More than 70% of graduates of certain health disciplines (social workers (85%), optometrists (80%), speech therapists, nurses (72%), dental therapists (70%)) have spent >5 years working at rural PHCFs, indicating that rural-origin students do return to work long-term in rural areas. In contrast, there were no obvious reasons for the low numbers of audiologists, dentists or occupational therapists working for an extended period at rural PHCFs, although for dentists, the lack of equipment for any services other than extractions was an issue, which needs further study to determine reasons for this. Pharmacists have been particularly negatively affected by the moratorium on employment post community service, and in some cases have been unable to secure posts in the public sector, requiring them to enter the private sector. A 2021 survey of 135 of 317 UYDF graduates confirmed that the lack of funded posts was the main reason that UYDF graduates were not working at rural PHCFs, followed by a lack of professional development opportunities.[11]
The findings of this study show that a higher percentage of rural-origin graduates supported by UYDF returned to work in rural areas than was reported in the tracking study undertaken by George et al.[6]
They reported that only 21/75 (28%) of rural-origin students enrolled at Wits between 2007 and 2011 were working in rural areas, and that only 33 (7%) of the 417 doctors tracked were working in rural areas. George et al.[6]concluded that being male, black and of rural origin was the strongest predictor of working in a rural area, but the low percentage of rural students who return to work in rural areas suggests that rural student selection alone is no guarantee that rural-origin graduates will work in rural areas. UYDF, in addition to rural recruitment, continually makes students aware of their obligation to serve their community on graduation, and exposes them to rural practice throughout their studies, which UYDF does by the compulsory 4 weeks per annum work exposure at their local rural hospital.[16] Further studies are needed to determine the role of these other measures in encouraging rural-origin students to work in rural areas. It is interesting to note that despite George et al.[6] identifying rural origin as a strong predictor of working in rural areas, only 18% (75/417) of these cohorts at Wits were of rural origin, suggesting that greater effort needs to be put into selecting rural-origin students if the university is serious about addressing the staffing situation at rural healthcare facilities.
It was disappointing to note that 10% of UYDF graduates did not return to work in rural areas at all. Further study is needed to determine the reasons for this, but anecdotal reports, and the 2021 survey results,[11] suggest that this is due to the lack of funded posts in rural areas, including community service placements, rather than an unwillingness by UYDF graduates to work in rural areas. In addition, despite all being of rural origin, only 32% of doctors continued working in a rural PHCF for more than 3 - 4 years, with only 14% working at a rural PHCF for >5 years. Lack of professional development opportunities, including the opportunity to specialise (career development) was cited a major reason why UYDF graduates did not remain at rural PHCFs.[11] Currently, all specialist training (except some family medicine training) is based at tertiary and regional hospitals situated in urban areas, and therefore necessitates a move to an urban area.
To address the long-term issues of staffing rural PHCFs, it is important for local hospital management and the Provincial DoH to address the pull factors that encourage HCPs to remain in rural areas, as well as the push factors that encourage HCPs to leave, and not rely on bonded scholarship graduates to fill posts at their hospitals, or on 1-year community service placements.[1,26] Although the employment of doctors is a key factor in service delivery at rural healthcare facilities, by supporting 18 different health science disciplines, the UYDF graduates have reduced staff shortages across all major departments at participating rural hospitals, thus helping to ensure a comprehensive health service, as opposed to a doctor-centric approach, in line with the delivery of primary healthcare.[1,24]
The biggest challenge facing the success of this initiative is the availability of funded posts for graduates in the public health sector. Since 1999, the UYDF has worked with the KZN Provincial DoH to identify priority training areas and select and support students wanting to train in these fields. Despite shortages of health personnel and calls to increase numbers of HCPs over the last decade, especially those willing to work in rural and underserved areas, there has been little growth in clinical posts in the public sector.[1,3] In addition, the introduction of austerity measures,[19,23] which has resulted in health science graduates, especially the allied healthcare disciplines, post community service not being employed by the DoH, is a lost opportunity, as rural-origin HCPs who are willing to work in rural areas and deliver healthcare services to indigent communities are being forced to obtain employment elsewhere. The impact of these measures potentially negates the benefits derived from rural bonded scholarships for staffing rural hospitals. Reid[25] concludes that compulsory community service is an effective strategy for recruiting health professionals to rural and underserved areas, but it is ineffective for retaining them in the absence of complementary longer-term human resource interventions, with the same being said of the UYDF scholarship scheme.[11]
Limitations
There are limited studies reporting on the duration that rural-origin health professionals work at a rural PHCF in SA, and therefore no comparison with this study could be made. Furthermore, although the Human Resources for Health document[1] defines long as 10 - 12 years, there is no consensus as to what working 'longer term' at a rural PHCF means, and what would be considered an ideal period.
Conclusion
The UYDF has shown that the investment in rural youth through a bonded scholarship can be an important strategy to provide much-needed staff at rural PHCFs in SA, as >90% of graduates worked at rural PHCFs, while 54% (219/405) worked for >3 years, with allied HCPs working on average for longer periods than doctors. For several disciplines, >70% of graduates worked for >5 years at a rural PHCF, contributing to long-term staff stability. However, to address the long-term challenges of staffing rural healthcare facilities, an integrated approach is needed, including selecting, supporting and orientating rural students towards rural practice, ensuring the availability of funded posts, addressing the common retention factors and addressing the other push and pull factors.
Declaration. None.
Acknowledgements. None.
Author contributions. AR and GM both contributed to the protocol development, analysis of the data and the final write-up. GM was responsible for the data extraction.
Funding. None.
Conflicts of interest. None.
References
1. Human Resources for Health South Africa: HRH Strategy for the Health Sector 2012/13 - 2016/17. Pretoria: National Department of Health, South Africa, 2011. [ Links ]
2. World Health Organization. A universal truth: No health without a workforce. Geneva: WHO, 2013. [ Links ]
3. National Department of Health, South Africa. 2030 human resources for health strategy: Investing in the health workforce for universal health coverage. Pretoria: NDoH, 2020. [ Links ]
4. Wilson NW, Couper ID, de Vries E, Reid S, Fish T, Marais BJ. A critical review of interventions to redress the inequitable distribution of healthcare professionals to rural and remote areas. Rural Remote Health 2009;9(2):1060-1082. https://doi.org/10.22605/RRH1060 [ Links ]
5. Ross A, MacGregor G, Campbell L. Review of the Umthombo Youth Development Foundation scholarship scheme, 1999 - 2013. Afr J Primary Healthcare Fam Med 2015;7(1):1-6. [ Links ]
6. George A, Blaauw D, Thompson J, Green-Thompson L. Doctor retention and distribution in post-apartheid South Africa: Tracking medical graduates (2007 - 2011) from one university. Hum Resource Health 2019;17(100):1-9. https://doi.org/10.1186/s12960-019-0439-4 [ Links ]
7. Russell D, Mathew S, Fitts M, et al. Interventions for health workforce retention in rural and remote areas: A systematic review. Hum Resource Health 2021;19(1): 1- 24. https://doi.org/10.1186/s12960-021-00643-7 [ Links ]
8. Ross A. Working in rural areas - the experiences of Umthombo Youth Development Foundation graduates. Afr J Primary Healthcare Fam Med 2014;6(1):e1-e7. https://doi.org/10.4102/phcfm. [ Links ]
9. Purohit B, Bandyopadhyay T. Beyond job security and money: Driving factors of motivation for government doctors in India. Hum Resource Health 2014;12(12):1-13. https://doi.org/10.1186/1478-4491-12-12 [ Links ]
10. Afriyie DO, Nyoni J, Ahmat A. The state of strategic plans for the health workforce in Africa. BMJ Glob Health 2019;4(Suppl 9):1- 5. https://doi.org/10.1136/bmjgh-2018-001115 [ Links ]
11. MacGregor RG, Ross A. The effects of various retention factors on the choice of where rural origin Umthombo Youth Development Foundation health science graduates work. Rural and Remote Health 2024;24:1-11. https://doi.org/10.22605/RRH8251 [ Links ]
12. KwaZulu-Natal Bursaries. KZN Department of Health, 2022. http://www.kznhealth.gov.za/bursaries.htm (accessed 24 January 2023). [ Links ]
13. Sui X, Reddy P, Nyembezi A, et al. Cuban medical training for South African students: A mixed methods study. BMC Med Educ 2019;19(1):1- 11. https://doi.org/10.1186/s12909-019-1661-4 [ Links ]
14. Slottow R. University of KwaZulu-Natal College of Health Sciences Guideline Document for Selection for the First Year Intake of 2016. University of KwaZulu-Natal, 2015. [ Links ]
15. Mapukata NO, Couper I, Smith J. The value of the WIRHE Scholarship Programme in training health professionals for rural areas: Views of participants. Afr J Prim Health Care Fam Med 2017;9(1):1-6. https://doi.org/10.4102/phcfm.v9i1.1488 [ Links ]
16. MacGregor RG, Ross AJ, Zihindula G. A rural scholarship model addressing the shortages of healthcare workers in rural areas. South African Health Review, Health Systems Trust. Durban Health Systems Trust; 2018:49-55. [ Links ]
17. Motala MJVW. Where are they working? A case study of twenty Cuban-trained South African doctors. Afr J Prim Health Care Fam Med 2019;21(11):1- 9. https://doi.org/10.4102/phcfm.v11i1.1977 [ Links ]
18. Smith J. Human resources for rural health - project evaluation. Pretoria: Swiss-South African Co-operative Initiative (SSACI), 2012. [ Links ]
19. KwaZulu-Natal Budget Policy Statement 2022/23. Pietermaritzburg, 2022. https://www.kznhealth.gov.za/Downloads/budget-speech-10052022.pdf (accessed 22 July 2022). [ Links ]
20. Apply for financial assistance from NSFAS. Pretoria, 2021. https://www.gov.za/services/tertiary-education/apply-financial-assistance-national-student-financial-aid-scheme-nsfas# (accessed 12 March 2021). [ Links ]
21. National Treasury. Delivering municipal services in rural areas. Chapter 12. Pretoria: National Treasury, 2011. www.treasury.gov.za/publications/igfr/2011/lg/15.%20rural%20services%202011%20lgber%20-%20final%20-%209%20sept%202011.pdf (accessed 12 March 2021). [ Links ]
22. De Vries E, Reid SJ. Do South African medical students of rural origin return to rural practice? S Afr Med J 2003;10(93):789-793. [ Links ]
23. KwaZulu-Natal Department of Health. Circular no G01/2022 - cost containment plan for 2021/22. Pietermaritzburg: KZN DoH, 2022 (accessed 14 July 2022). [ Links ]
24. Gumede DM, Taylor M, Kvalsvig J. Engaging future healthcare professionals for rural health services in South Africa: Students, graduates' and managers' perceptions. BMC Health Serv Res 2021;21(1):1-15. https://doi.org/10.1186/s12913-021-06178-w [ Links ]
25. Reid S. 20 years of community service in South Africa: What have we learnt? Durban: Health Systems Trust, 2018:41-50. [ Links ]
 Correspondence:
Correspondence:
A J Ross
Rossa@ukzn.ac.za
Accepted 12 December 2023














