Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.114 no.2 Pretoria feb. 2024
http://dx.doi.org/10.7196/SAfrMedJ..2024.v114i2.1176
RESEARCH
The burden and outcomes of firearm injuries at two district-level emergency centres in Cape Town, South Africa: A descriptive analysis
L BushI; C HendrikseI, II; C van KoningsbruggenI, II; K EvansI, II
IMB ChB, MMed; Division of Emergency Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
IIMB ChB, MMed; Emergency Centres, Mitchells Plain and Heideveld Hospitals, Cape Town, South Africa
ABSTRACT
BACKGROUND: In South Africa (SA), injuries are the second leading cause of years of healthy life lost, and interpersonal violence dominates the SA injury profile. Half of all injury-related deaths in SA are intentional, and firearms contribute to a quarter of these deaths. Injury surveillance systems are essential to develop, implement and monitor strategies that reduce preventable trauma
OBJECTIVES: To describe the burden of patients with firearm injuries and their outcomes at district-level emergency centres in the Western Cape
METHODS: This study was a retrospective analysis of a prospectively collected database. All patients who presented to two district-level emergency centres with a firearm injury over a 12-month period (1 January 2019 - 31 December 2019) were eligible for inclusion
RESULTS: Firearm injuries represented 5.7% of the trauma burden at the two district emergency centres. Of the 776 patients with firearm injuries who were included, the median age was 27 years, and 91% were male. A total of 520 (67%) patients self-presented, and there were 18 (2.3%) deaths in the emergency centre and a further 23 (3%) as inpatients. Of the total where wound location was determined (n=595), 30.4% sustained more than one firearm injury, and 112 out of the 167 admitted to Mitchells Plain Hospital required at least one visit to theatre. This accounted for 413 theatre hours and 1 376 inpatient bed days at Mitchells Plain Hospital. A significant proportion of patients (n=219, 29%) were transferred from the emergency centres to a tertiary service for further care
CONCLUSION: Firearm injuries represent a substantial proportion of the trauma burden at district emergency centres in the Western Cape Province. Managing patients with firearm injuries is resource intensive, as evident by their high acuity, the need for operative care, the long length of stay, the high burden on emergency medical services with interfacility transfers and the high demand for tertiary care. Data from this study aid our understanding of the prevalence and burden of firearm injuries at district level emergency centres, and multisectoral action, supported by evidence-based primary and secondary preventive strategies, is required to reduce the burden of firearm injuries, and mitigate their effects
Globally, 251 000 deaths, or 5.4% of all injury-related deaths, were due to firearm injuries in 2016, with 41% of deaths due to interpersonal violence as a result of a firearm, a 5.7% increase from 2006.[1] Interpersonal violence was estimated to account for 1.5 million hospital admissions, with a further 28 million managed as outpatients in 2016. While there has been a global decrease in interpersonal violence between 1990 and 2013, the south sub-Saharan and Oceania regions have seen an estimated 50% increase in interpersonal violence disability adjusted life-years (DALY).[2]
In South Africa (SA), injuries are the second-leading cause of years of healthy life lost, and interpersonal violence dominates the SA injury profile.[3] An estimated 49% of all injury-related deaths in SA are intentional, and firearms are involved in a quarter of these deaths.[4] Between 1990 and 2016, the SA firearm-related age-standardised death rate declined from 13.1 to 7.1 per 100 000,[5] with some of this decline attributable to the Firearms Control Act No. 60 of 2000.[4,6] Since 2013 there has been a 7.8% year-on-year increase in murders in the Western Cape Province of SA, with communities such as Philippi East, in the Cape Town metropole, recording a murder rate of 247 per 100 000 people.[7] This is more than 40 times the estimated global murder rate of 6.2 per 100 000 people.[8] Mortuary statistics in the Western Cape from 2015 revealed that firearm victims outnumbered victims due to road traffic crashes and penetrating injuries,[9] and in 2018/2019, 46% of all homicides were due to firearm injuries.[10]
Long-term mortality is likely higher for survivors of firearm injuries than other injury profiles,[11,12] and injury surveillance systems are essential to develop, implement and monitor strategies that reduce preventable trauma.[13] Unfortunately, barriers exist in low- and middle-income countries, and an attempt at implementing such a system at a district hospital in Cape Town concluded that it was not sustainable.[14] Beyond mortality data and without adequate injury surveillance, the available SA firearm injury literature is further limited in scope and depth. The focus is on pre-hospital,[15] hospital-specific,[16-21] or tertiary and orthopaedic services,[22-26] with little co-ordinated research documenting the complete burden of this injury profile on health services and society. There is no local research documenting rates of recidivism or strategies that reduce this, or the escalation of violent injury patterns that is suggested by the international literature.[27]
This study aims to describe the burden of patients with firearm injuries and their outcomes at district-level emergency centres in the Western Cape Province, SA.
Methods
Study design
A retrospective analysis of an observational database was performed, with missing data and additional variables from a subsequent chart review.
Study setting
Mitchells Plain Hospital (MPH) is a large district-level hospital about 30 km from Cape Town and the nearest trauma centre and tertiary hospital, Groote Schuur Hospital. It has around 300 beds and serves a population of approximately 600 000. Sixty-two percent of Mitchells Plain's population is <29 years of age, with 48% of households living below the poverty line and only 43% of the working-age population employed.[28] The reported violent crime rate of the area that MPH serves is 1 930/100 000 population,[28] and includes Philippi, a nearby informal settlement with a murder rate of 247 per 100 000 people.[7]
Heideveld Hospital (HEC) is the only stand-alone district level emergency centre in the Western Cape Province, ~20 km from Cape Town. Communities adjacent to Heideveld have deeply entrenched gangs, and much of the violent crime is related to inter-gang warfare and control of the local drug trade.[10] MPH and HEC are co-managed by a team of four emergency physicians and treat over 70 000 patients per annum - approximately 55% being of high acuity (red and orange triage category).[29]
Patients presenting to MPH Emergency Centre, depending on the level of care required, may be admitted to MPH, or be referred to the tertiary hospital. MPH has access to 24/7 operating theatres, two full-time general surgery consultants and one anaesthetic consultant. Outside of office hours, a medical officer or registrar manages cases with a consultant on call from home. MPH has no after-hours computed tomography scan service, nor does it have a high care or intensive care unit. HEC has no on-site surgical, anaesthetic support service or advanced radiology services, and patients requiring admission or operative care are referred to either MPH or the tertiary hospital, depending on the acuity. Neither facility has an on-site blood bank, with only limited O-positive and negative packed red cells and freeze-dried plasma immediately available for transfusion.
Sampling and study participants
A convenience sampling strategy was used. All patients with a firearm injury over a 12-month period (1 January 2019 - 31 December 2019) were included. These facilities were chosen because they share similar care pathways and a mutual tertiary facility. The SA National Defence Force (SANDF) was deployed from 17 July 2019 in several of the communities serviced by the two facilities to reduce gang-related violence.
Data collection and content management
The data collection process involved two phases. The first phase comprised of exporting demographic, triage and emergency centre process data for all patients with firearm injuries from the Hospital and Emergency Centre Tracking Information System (HECTIS) registry by performing an ICD-10 search (X93-95, W32-34, X72-74). Manually entered triage descriptors (gun, GSW, GWS) were also searched for, to ensure that no cases were excluded because of an inaccurate ICD-10 code. Phase 2 involved the collection of admission and outcome details from the Clinicom database and clinical details from the electronic content management system (ECM) database at MPH, and by scrutinising patient folders at HEC. Where available, the electronic continuity of care record (ECCR) provided discharge summaries for the MPH patients.
MPH and HEC utilise an electronic patient tracking and registration system called HECTIS. It was designed to streamline and track patient processes in the emergency centre, by collecting patient process times, triage scores, ICD-10 diagnosis assigned at disposition and disposition decisions. The data are stored electronically in an off-site Oracle database version 12.1.0.2.0 (Oracle Corp., USA). Clinicom is a patient administrative and billing system, and ECM provides scanned clinical records and ECCR summaries. Age categories were defined as per World Health Organization classification, and incident location and home address were retrieved to allow for geospatial analysis. All data were de-identified and exported to an Excel (Microsoft, USA) database stored in a protected University of Cape Town Microsoft OneDrive.
Statistical analysis
Descriptive statistics were used to describe the demographics and clinical details of patients. Categorical data were presented as frequency counts and proportions and assessed for non-random associations with the x2 test. The Shapiro-Wilk test was applied to assess the distribution of all numerical data and expressed as median and interquartile range if non-normal. Weekends were defined as Saturday and Sunday, after hours between 16h00 and 8h00, and time data presented as hours:minutes. Data were analysed with SPSS Statistics version 26.0 (IBM Corp., USA), and geospatial analysis presented as a Kernel density heatmap using ArcGIS software (Esri, USA). Statistical significance was defined as p<0.05.
Ethical considerations
Ethical approval was granted by the University of Cape Town Human Research Ethics Committee (ref. no. 044/2020) and facility approval was obtained via the National Health Research Database (ref. no. WC_202002_029).
Results
During the study period, MPH and HEC emergency centres attended to a total of 49 577 and 18 051 emergency visits, respectively, of which 9 629 (19%) and 4 035 (22%) were trauma related. Of the trauma-related presentations, 565 (5.9%) and 286 (7.1%) were because of firearm injuries at the two facilities, respectively, and therefore eligible for inclusion. Only 9 (1.5%) of the MPH folders were excluded because of incomplete or inaccessible clinical documentation (Fig. 1).
Demographics and process data
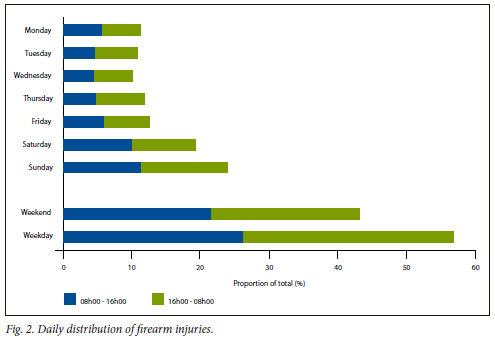
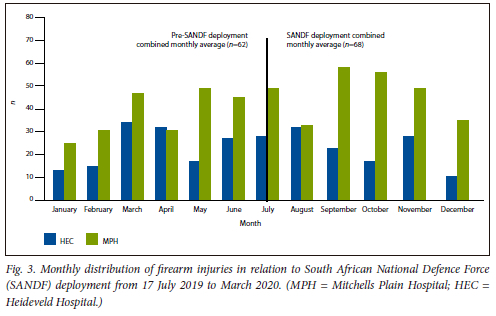
The age distribution was skewed to the right, with 80% of all patients <36 years old (Table 1). There was a strong male preponderance of 714 (91%), with a median age of 27 years (interquartile range (IQR) 21 - 34). A total of 89 (11%) were <18 years old, with 18 (2.3%) aged <13 years. Of the included sample, 520 (67%) arrived using their own transport, with 242 (31.2%) arriving by ambulance, either as a primary call or as an interfacility transfer. A total of 581 (74%) presented outside of office hours, with presentations on weekends totalling 340 (43.2%) (Fig. 2). The maximum daily numbers of patients with firearm injuries arriving at MPH and HEC were 14 and 6, respectively. The median emergency centre process times were arrival to triage 0:16 (IQR 0:31), triage to consultation 1:03 (IQR 3:09) and arrival to exit 8:00 (IQR 8:48). Fig. 3 depicts the monthly distribution of firearm presentations. It includes a period before and after the deployment of the SA National Defence Force, as a response to the apparent increasing levels of gang-related firearm violence at the time.[29]
Geospatial data
The home suburb, within the geographically defined service area of the facility, was determined for 593 patients, generating the heatmap in Fig. 4.
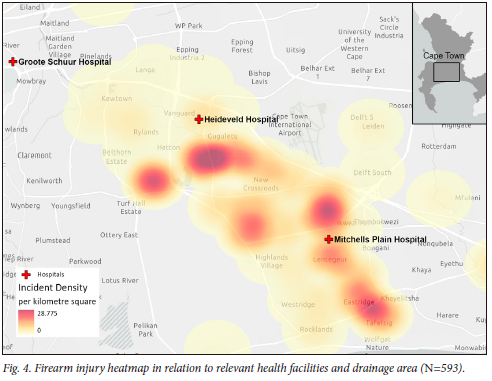
There were 52 records available where the distance between the street address and incident location could be accurately recorded from the ambulance record on ECM. Including those injured at home, the median incident distance from home was <1 km.
Clinical and outcome data
A total of 595 (30.4%) patients sustained more than one firearm injury, with 13.7% sustaining a head or neck injury, 22.4% a chest, 21.5% an abdominal and 66.9% an extremity injury (Table 2).
Overall, 18 (2%) patients died in the emergency centre, and of those that survived to emergency centre disposition (n=749), 313 (41.6%) were discharged home, 224 (29.7%) were transferred out and 167 (22.2%) admitted to a ward at MPH, accounting for 1 376 inpatient bed days. In total, 417 (55.3%) required an admission to hospital beyond their emergency centre care or following transfer to the tertiary centre trauma unit. A total of 30 (4%) patients required an admission to an intensive care unit (ICU).
More than a third of the patients at MPH were referred to the surgical team and almost one in five to the orthopaedic service. A total of 49 (9.5%) patients that presented to MPH emergency centre went directly from the emergency centre to theatre. Of the 167 patients admitted to MPH, 112 (67.1%) required at least one theatre visit, resulting in 125 operations, with a total of 413 hours of theatre time required. A total of 41(5.3%) patients died after arrival to both emergency centres, and almost a third (n=9, 1.2%) of those admitted to ICU died (Table 3).
The Triage Early Warning Score (TEWS) and SA Triage Scale (SATS) categories[30] showed marked variation in the proportion categorised to each colour code (Table 2). Almost a third of those triaged red died, and despite the variation in less urgent categories, there were no deaths in those triaged yellow or green (Table 3). The TEWS numeric score and the Shock Index (SI - heart rate divided by systolic blood pressure) also showed a difference in those surviving to discharge.
The Revised Trauma Score (RTS) could only be calculated from the MPH patients, and included 21 of the 28 deaths and total of 478 patients.
Discussion
This study set out to describe the burden of patients with firearm injuries and their outcomes at two district-level emergency centres in the Western Cape. A total of 776 patients with firearm injuries presented to the two facilities during the study period, comprising 6% of all trauma presentations. Because firearm injury victims presented with a high acuity (82% triage red and orange with SATS), they were prioritised and this resulted in resources, including staff and resuscitation room space, being redirected from the other patients. This is reflected in significantly shorter time to triage (16 minutes v. 30 minutes) and time to consultation (60 minutes v. 200 minutes) than the general patient population.[31] The burden on the hospitals and emergency medical services (EMS) was significant, with 43% requiring admission and half of these requiring transfer to the tertiary hospital. At the district hospital, 67% of admitted patients received operative interventions, with a resultant 413 theatre hours required (~4 hours per patient). A total of 5.3% died because of the firearm injury, and half of those occurred after being transferred to the tertiary hospital. The majority (78%) presented outside of traditional office hours, further straining the emergency centre during times when staffing numbers are usually more constrained.
The surgical burden is apparent by the high proportion of admissions and transfers out to a tertiary service for surgical care (1 in 5). This is partly a result of HEC not having access to any onsite surgical services. Limited after-hours surgical cover and the absence of advanced imaging, an onsite blood bank, high care or an ICU may have influenced decisions to transfer to a higher level of care. The fact that almost a third of patients who required admission at MPH went directly to theatre from the emergency centre highlights the significant onsite surgical requirements at district level, which may have deleterious effects on theatre access in general.
Most firearm injuries occurred in the same suburb in which the injured person lived. This is in keeping with international research,[32] and 67% (n=520) arrived at MPH/HEC using their own transport. If you include those transferred to MPH and HEC from primary healthcare, three out of every four patients self-presented to a primary or district level service, either to be managed at these facilities or transferred to a higher level of care. This is not unusual in low- and middle-income countries, where EMS systems are immature or access to prehospital care is limited,[33,34] and even in well-resourced settings, interfacility transfer of firearm injuries may result in better outcomes.[35] Considering the high proportion of transfers to the tertiary centres after presenting to the district hospital, one could argue that patients transported by EMS should go directly to the tertiary centres.[15] This argument is, however, complicated by unclear transfer guidelines and care pathways, with patients potentially too physiologically unstable to transport further than the nearest hospital. Wound location[36] and shock index may assist in recognising those at highest risk for deterioration.[37,38]
The young male predominance is consistent with data from other facilities in Cape Town.[17,20,21] It is apparent that triage for the majority of those injured occurred timeously, 0:16 (IQR 0:31) after arrival. With a median time from triage to consult at 1:03 (IQR 3:09), and arrival to exit at 8:00 (IQR 8:48), it is likely that this injury profile is prioritised both in terms of triage and other processes.[39] This may result in improved quality of care or rapid access to services for those with firearm injuries, but likely negatively affects other patients requiring emergency care, especially outside of office hours. The prioritisation of firearm injuries may theoretically have deleterious effects on patient safety in general, and may affect access to emergency care because of longer waiting times for the general population.
Almost a third of patients sustained more than one firearm injury, with 54% of the 741 wounds sustained to extremities, 11% to the head and neck, 18% to the chest and 17% to the abdomen. Expectedly, those sustaining multiple injuries or those with head, neck, or torso injuries were most likely to die.
The TEWS predicted critical outcomes and mortality more accurately than the SATS, specifically for the orange triage category. SATS was not created or validated to predict outcomes, but rather to sort patients in categories of priority. The SATS discriminator accounts for this variation. It is unclear as to the discriminators used, being subjective, without evidence base and not documented at triage.
A total of 50 patients (41 who arrived alive and 9 declared dead on arrival) went to the forensic mortuary. These deaths account for a very small portion of the total forensic burden caused specifically by firearms and violent deaths in general.[40]
It is unclear what practical interventions should be undertaken to reduce repeat and escalating patterns of violent injury for survivors of all violent injury, and how this should be integrated into hospital services. The international literature provides advice specific to firearm violence,[41] but local strategies including the tightening of gun laws, combatting gangsterism and drugs and specific alcohol and violence prevention interventions should be developed.[42-44] By reducing the number of those injured, the costs of implementing such strategies may be recovered from the direct and measurable healthcare cost savings without even considering the benefit to society. The total effect and cost on society of violent injury, specifically firearm injury, is unmeasured, and evidence-based primary and secondary preventive strategies must be integrated into government and civil society's response to this preventable epidemic of violent injury.[44]
Limitations
The firearm wound location data for patients at HEC were incomplete, and this accounts for the 595 patients included in the wound location data. There was no determination made as to entrance and exit, as this is determined incorrectly ~50% of the time.[45] There is also possibly an undercount of firearm wounds, as unless the notes specified the number of retained bullets, two entrance wounds may have been documented as a single wound. Where the notes were unclear, an even number of wounds were taken as entrance and exit and so documented as a single wound, so as not to double-count bullets, with location documented in order of the following: head/neck, chest, abdomen and extremity. There is also significant missing information with regard to the wound location of patients who died, as their folders were with forensic services and unavailable. This may have impacted the accuracy of the wound location data, especially when compared with those who survived. The RTS also excluded HEC patients for the same reason, and also those where a Glasgow Coma Scale or blood pressure was not documented. Although RTS predicts mortality, including an Injury Severity Score and the Trauma Injury Severity Score would have better documented severity and probability of death. The study under-reports the burden on theatre services, as only MPH theatre data were recorded. With 105 MPH patients and 114 HEC patients transferred to the tertiary institution, the theatre burden at tertiary level is likely significant.
Suggestions for future research
Future studies should consider multicentre epidemiological assessment of the burden of firearm injuries on the health system, and should include all levels of care. This information would allow for a more accurate economic assessment of the healthcare costs,[46,47] including years lived with disability, years of life lost,[2,48] and potentially add to a list of all deficits framework, which would measure the full burden of injury and violence across individual, family, and societal domains.[49]
Conclusion
Firearm injuries represent a substantial proportion of the trauma burden at district emergency centres in the Western Cape. Managing patients with firearm injuries is resource intensive, as evident by their high acuity, the need for operative care, the long length of stay, the burden on EMS with interfacility transfers and the high demand for tertiary care. In addition, the quicker process times with regard to their care pathways within the facilities suggest that firearm victims are prioritised over other patients - potentially contributing to longer waits and limiting access to emergency care for other patients, especially during weekends. This study examines a large cohort of firearm injuries and provides some understanding of prevalence and burden. An impact and economic analysis from this cohort would develop a costing analysis for this injury profile.
Declaration. This study was submitted by the first author for an MMed degree from the University of Cape Town.
Acknowledgements. The authors would like to acknowledge Dr Moosa Parak (HECTIS) for his assistance in accessing the data for this research, and Dr Adam Khan for assistance with data collection and Thomas Slingsby for generating the heat map.
Author contributions. All authors contributed to the research conception and design. LB performed the data collection and CH the data analysis, with the first draft written by LB and CH. The other authors commented on subsequent versions, and all authors have read and approved of the final manuscript.
Funding. The data collection was supported by a ZAR5 000 research grant awarded to KE by Mitchells Plain Hospital Academic Fund.
Conflicts of interest. None.
References
1. Naghavi M, Abajobir AA, Abbafati C, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980 - 2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390(10100):1151-1210. https://doi.org/10.1016/S0140-6736(17)32152-9 [ Links ]
2. Haagsma JA, Graetz N, Bolliger I, et al. The global burden of injury: Incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013. Inj Prev 2015;22(1):3-18. http://doi.org/10.1136/injuryprev-2015-041616 [ Links ]
3. Norman R, Matzopoulos R, Groenewald P, Bradshaw D. The high burden of injuries in South Africa. Bull World Health Organ 2007;85(February):695-702. https://doi.org/10.2471/blt.06.037184 [ Links ]
4. Matzopoulos R, Prinsloo M, Pillay-van Wyk V, et al. Injury-related mortality in South Africa: A retrospective descriptive study of postmortem investigations. Bull World Health Org 2015;93(5):303-313. https://doi.org/10.2471/blt.14.145771 [ Links ]
5. Nand D, Naghavi M, Marczak LB, et al Global mortality from firearms, 1990 - 2016. JAMA 2018;320(8):792-814. https://doi.org/10.1001/jama.2018.10060 [ Links ]
6. Matzopoulos R, Groenewald P, Abrahams N, Bradshaw D. Where have all the gun deaths gone? S Afr Med J 2016;106(6):589-591. https://doi.org/10.7196/samj.2016.v106i6.10379 [ Links ]
7. Western Cape Government, South Africa. Provincial Crime Report 2016/17. https://www.westerncape.gov.za/assets/crime_analysis_western_cape_2016-17.pdf (accessed 7 June 2023). [ Links ]
8. United Nations Office on Drugs and Crime VI. Global Study on Homicide 2019, Booklet 2. Geneva: UN, 2019. https://www.unodc.org/unodc/en/data-and-analysis/global-study-on-homicide.html (accessed 7 June 2023). [ Links ]
9. Republic of South Africa National Assembly. Question No. 3408 (internal question paper no. 37, 4 September 2015). https://pmg.org.za/files/RNW3408-151026.docx (accessed 7 June 2023). [ Links ]
10. Western Cape Crime Report 2018/19. Cape Town: Department of Community Safety, 2018. https://www.westerncape.gov.za/sites/www.westerncape.gov.za/files/wccs_crime_report_2020-03-25_medres.pdf (accessed 7 June 2023). [ Links ]
11. Fahimi J, Larimer E, Hamud-Ahmed W, et al. Long-term mortality of patients surviving firearm violence. Inj Prev 2015;22(2):129-134. https://doi.org/10.1136/injuryprev-2015-041710 [ Links ]
12. Shaahinfar A, Yen IH, Alter HJ, et al. Long-term mortality in pediatric firearm assault survivors: A multicenter, retrospective, comparative cohort study. Acad Emerg Med 2018;25(12):1447-1457. https://doi.org/10.1111/acem.13631 [ Links ]
13. Ward CL, Artz L, Berg J, et al. Violence, violence prevention, and safety: A research agenda for South Africa. S Afr Med J 2012;102(4):215-218. http://samj.org.za/index.php/samj/article/view/5544/4001 (accessed 8 June 2023). [ Links ]
14. Matzopoulos R, Zavala D, Mtonga R, et al Implementation challenges facing hospital-based surveillance systems in Africa: Lessons learned from IPPNWs Multinational Injury Surveillance System (MISSPP) and South Africa's National Non-fatal Injury Surveillance System (NANFISS) pilot projects. Inj Prev 2010;16:A144. https://doi.org/10.1136/ip.2010.029215.517 [ Links ]
15. Hardcastle TC, Finlayson M, van Heerden M, Johnson B, Samuel C, Muckart DJJ. The prehospital burden of disease due to trauma in KwaZulu-Natal: The need for Afrocentric trauma systems. World J Surg 2012;37(7):1513-1525. https://doi.org/10.1007/s00268-012-1852-1 [ Links ]
16. Hanewinckel R, Jongman HP, Wallis LA, et al. Emergency medicine in Paarl, South Africa: A cross-sectional descriptive study. Int J Emerg Med 2010;3:143-150. https://doi.org/10.1007/s12245-010-0185-9 [ Links ]
17. Hunter LD, Lahri S, van Hoving DJ. Case mix of patients managed in the resuscitation area of a district-level public hospital in Cape Town. African J Emerg Med 2017;7(1):19-23. https://doi.org/10.1016/j.afjem.2017.01.001 [ Links ]
18. Hodkinson PW, Wallis LA. Cross-sectional survey of patients presenting to a South African urban emergency centre. Emerg Med J 2009;26(9):635-640. https://doi.org/10.1136/emj.2008.063362 [ Links ]
19. Wallis LA, Twomey M. Workload and casemix in Cape Town emergency departments. S Afr Med J 2007;97(12):1276-1280. http://www.ncbi.nlm.nih.gov/pubmed/18264609 (accessed 8 June 2023). [ Links ]
20. Zaidi AA, Dixon J, Lupez K, et al. The burden of trauma at a district hospital in the Western Cape Province of South Africa. Afr J Emerg Med 2019;9(January):S14-S20. https://doi.org/10.1016/j.afjem.2019.01.007 [ Links ]
21. Aspelund AL, Patel MQ, Kurland L, McCaul M, van Hoving DJ. Evaluating trauma scoring systems for patients presenting with gunshot injuries to a district-level urban public hospital in Cape Town, South Africa. Afr J Emerg Med 2019;August:0-1. https://doi.org/10.1016/j.afjem.2019.07.004 [ Links ]
22. Schuurman N, Cinnamon J, Walker BB, et al. Intentional injury and violence in Cape Town, South Africa: An epidemiological analysis of trauma admissions data. Glob Health Action 2015;8(1):27016. https://doi.org/10.3402/gha.v8.27016 [ Links ]
23. Norberg J, Nilsson T, Eriksson A, Hardcastle T. The costs of a bullet - inpatient costs of firearm injuries in South Africa. S Afr Med J 2009;99(6):442-444. http://www.ncbi.nlm.nih.gov/pubmed/19736845 (accessed 8 June 2023). [ Links ]
24. Van Heukelum M, le Roux N, Jakoet S, Ferreira N. Financial burden of orthopaedic gunshot-related injury management at a major trauma centre. S Afr Med J 2020;110(9):882. https://doi.org/10.7196/samj.2020.v110i9.14638 [ Links ]
25. Jakoet MS, Burger M, van Heukelum M, et al The epidemiology and orthopaedic burden of civilian gunshot injuries over a four-year period at a level one trauma unit in Cape Town, South Africa. Int Orthop 2020;44(10):1897-1904. https://doi.org/10.1007/s00264-020-04723-6 [ Links ]
26. Martin C, Thiart G, McCollum G, Roche S, Maqungo S. The burden of gunshot injuries on orthopaedic healthcare resources in South Africa. S Afr Med J 2017;107(7):626-630. https://doi.org/10.7196/samj.2017.v107i7.12257 [ Links ]
27. Kao AM, Schlosser KA, Arnold MR, et al Trauma recidivism and mortality following violent injuries in young adults. J Surg Res 2019;237:140-147. https://doi.org/10.1016/j.jss.2018.09.006 [ Links ]
28. Western Cape Government, South Africa. Mitchells Plain nodal economic development profile. Western Cape Government, 2005. http://www.btrust.org.za/repository/5_CIPPN_Mitchells%20Plain%20narrative.pdf (accessed 7 June 2023). [ Links ]
29. UCT News. Measuring the success of the Cape Flats army deployment. Cape Town: UCT New, 2020. https://www.news.uct.ac.za/article/-2020-01-16-measuring-the-success-of-the-cape-flats-army-deployment (accessed 7 June 2023). [ Links ]
30. South African Triage Group. The South African Triage Scale Training Manual 2012. SATG, 2012;1-34. https://emssa.org.za/wp-content/uploads/2017/10/SATS-Manual.pdf (accessed 7 June 2023). [ Links ]
31. Hendrikse C, Parak M, van Hoving DJ. A descriptive analysis of the effect of the national COVID-19 lockdown on the workload and case mix of patients presenting to a district-level emergency centre in Cape Town, South Africa. S Afr Med J 2020;110(11):1113-1118. https://doi.org/10.7196/samj.2020.v110i11.15028 [ Links ]
32. Newgard CD, Sanchez BJ, Bulger EM, et al A geospatial analysis of severe firearm injuries compared to other injury mechanisms: Event characteristics, location, timing, and outcomes. Acad Emerg Med 2016;23(5):554-565. https://doi.org/10.1111/acem.12930 [ Links ]
33. Kironji A, Hodkinson P, de Ramirez SS, et al Identifying barriers for out of hospital emergency care in low and low-middle income countries: A systematic review. BMC Health Serv Res 2018;18:291. https://doi.org/10.1186/s12913-018-3091-0 [ Links ]
34. Kobusingye OC, Hyder AA, Bishai D, Hicks ER, Mock C, Joshipura M. Emergency medical systems in low- and middle-income countries: Recommendations for action. Bull World Health Org 2005;83(8):626-631. [ Links ]
35. Renson A, Schubert FD, Gabbe LJ, Bjurlin MA. Interfacility transfer is associated with lower mortality in undertriaged gunshot wound patients. J Surg Res 2019;236:74-82. https://doi.org/10.1016/j.jss.2018.11.011 [ Links ]
36. Feldman KA, Tashiro J, Allen C, et al. Predictors of mortality in pediatric urban firearm injuries. Pediatr Surg Int 2017;33:53-58. https://doi.org/10.1007/s00383-016-3984-0 [ Links ]
37. Olaussen A, Blackburn T, Mitra B, Fitzgerald, M. Shock Index for Critical Bleeding. Emerg Med Australas 2014;26:223-228. https://doi.org/10.1111/1742-6723.12232 [ Links ]
38. Campos-Serra A, Montmany-Vioque S, Rebasa-Cladera P, et al. The use of the shock index as a predictor of active bleeding in trauma patients. Cirugía Espanola (English ed) 2018;96(8):494-500. https://doi.org/10.1016/j.cireng.2018.09.007 [ Links ]
39. Hoffe ME, McCaul M, Hendrikse C. Emergency clinician output in a district hospital emergency centre: A cross-sectional analysis. Afr J Emerg Med 2022;12(3):264-269. https://doi.org/10.1016/j.afjem.2022.05.008 [ Links ]
40. Prinsloo M, Mhlongo S, Dekel B, et al. The 2nd Injury Mortality Survey: A national study of injury mortality levels and causes in South Africa in 2017. Cape Town: South African Medical Research Council, 2021. [ Links ]
41. Patel J, Leach-Kemon K, Curry G, Naghavi M, Sridhar D. Firearm injury - a preventable public health issue. Lancet Pub Health 2022;7(11):e976-982. https://doi.org/10.1016/s2468-2667(22)00233-x [ Links ]
42. Van Hoving DJ, van Koningsbruggen C, de Man M, Hendrikse C. Temporal changes in trauma according to alcohol sale restrictions during the South African national COVID-19 lockdown. Afr J Emerg Med 2021;11(4):477-482. https://doi.org/10.1016/j.afjem.2021.08.001 [ Links ]
43. Matzopoulos R, Prinsloo M, Bradshaw D, Abrahams N. Reducing homicide through policy interventions: The case of gun control. S Afr Med J 2019;109(11b):63-68. https://doi.org/10.7196/samj.2019.v109i11b.14256 [ Links ]
44. Navsaria P, Maqungo S, Marineau L, Prinsloo M, Molefe IJ, Hodkinson P. Firearm pandemic: Time to act and flatten the curve. S Afr Med J 2023;113(3):113-114. https://doi.org/10.7196/samj.2023.v113i3.316 [ Links ]
45. Collins KA, Lantz PE. Interpretation of fatal, multiple, and exiting gunshot wounds by trauma specialists. J Forensic Sc 1994;39(1):13574J. https://doi.org/10.1520/jfs13574j [ Links ]
46. Bowman B. Towards a South African injury costing model: A review of the literature for the development of a process path. Afr Saf Promot 2002;1(1):55-64. https://wiredspace.wits.ac.za/bitstreams/1d03889b-a8cb-45cc-b336-d4b34335d96b/download (accessed 12 June 2023). [ Links ]
47. Bowman B, Stevens G, Seedat M, Snyman R. Costing injuries in South Africa: Preliminary results and challenges from a pilot study. Afr J Health Sci 2010;17:57-63 https://www.ajol.info/index.php/ajhs/article/view/99567/88852 (accessed 12 June 2023). [ Links ]
48. Norman R. Estimates of injury mortality and disability based on the Cape Metropole study. Estimates of injury mortality and disability based on the Cape Metropole study. 2002. https://www.samrc.ac.za/sites/default/files/attachments/2022-08/cmsreport.pdf (accessed 7 June 2023). [ Links ]
49. Lyons RA, Finch CF, McClure R, van Beeck E, Macey S. The injury List Of All Deficits (LOAD) framework - conceptualising the full range of deficits and adverse outcomes following injury and violence. Int J Injury Control Safety Promotion 2010;17(3):145-159. https://doi.org/10.1080/17457300903453104 [ Links ]
 Correspondence:
Correspondence:
L Bush
luke.bush@westerncape.gov.za
Accepted 21 November 2023














