Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.114 n.2 Pretoria Feb. 2024
http://dx.doi.org/10.7196/SAMJ.2024.v114i2.1306
RESEARCH
The development of a nurse-led preoperative anaesthesia screening tool by Delphi consensus
M B NejthardtI, II; P AlexandrisIII; S BechanIV; M F A BijliV; S ChettyVI; J M DippenaarVII; M W GibbsVIII, IX; M JohnsonX; H KluytsXI; R LlewellynXII, XIII; M MotiangXIV; P MoganeXV, XVI; P MotshabiXVII, XVIII; B MraraXIX; F RoodtXX, XXI; U SinghXXII; S SpijkermanXXIII; E TurtonXXIV; J van der WesthuizenXXV; B M BiccardXXVI, XXVII
IMB BCh, FCA (SA); Department of Anaesthesia and Perioperative Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
IIMB BCh, FCA (SA); Department of Anaesthesia and Perioperative Medicine, Groote Schuur Hospital, Cape Town, South Africa
IIIMB ChB, FCA (SA); Department of Anaesthesia, Faculty of Health Sciences, Nelson Mandela University, Gqeberha, South Africa
IVMB ChB, Cert Crit Care (SA); Discipline of Anaesthesiology and Critical Care, Nelson R Mandela School of Medicine, University of Kwa-Zulu Natal, Albert Luthuli Academic Hospital, Durban, South Africa
VMB ChB; Department of Anaesthesia and Perioperative Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
VIMB ChB, PhD; Department of Anaesthesia and Critical Care, Stellenbosch University and Tygerberg Hospital, Cape Town, South Africa
VIIMB ChB, MMed (Anaes); Department of Anaesthesiology, Steve Biko Academic Hospital, University of Pretoria, South Africa
VIIIMB ChB, FCA (SA); Department of Anaesthesia and Perioperative Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
IXMB ChB, FCA (SA); Department of Anaesthesia and Perioperative Medicine, Groote Schuur Hospital, Cape Town, South Africa
XMB ChB, FCA(SA); Department of Anaesthesia and Critical Care, Stellenbosch University and Tygerberg Hospital, Cape Town, South Africa
XIMB ChB, FCA (SA); Department of Anaesthesiology and Critical Care, Sefako Makgatho Health Sciences University, Pretoria, South Africa
XIIMB ChB, FCA (CMSA); Department of Anaesthesia and Perioperative Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
XIIIMB ChB, FCA (CMSA); Department of Anaesthesia and Perioperative Medicine, Groote Schuur Hospital, Cape Town, South Africa
XIVMB ChB, MMed; Department of Anaesthesiology and Critical Care, Sefako Makgatho Health Sciences University, Pretoria, South Africa
XVMB BCh, FCA (SA); Department of Anaesthesiology, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
XVIMB BCh, FCA (SA); Department of Anaesthesia, Chris Hani Baragwanath Hospital, Soweto, South Africa
XVIIMB ChB, PhD; Department of Anaesthesiology, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
XVIIIMB ChB, PhD; Department of Anaesthesia, Charlotte Maxeke Hospital, Johannesburg, South Africa
XIXMB BCh, Cert Crit Care (SA); Department of Anaesthesia and Critical Care, Nelson Mandela Academic Hospital, Walter Sisulu University, Mthatha, South Africa
XXMB ChB, FCA (SA); Department of Anaesthesia and Perioperative Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
XXIMB ChB, FCA (SA); George Provincial Hospital, George, South Africa
XXIIMB ChB, FCA (SA); Discipline of Anaesthesiology and Critical Care, Nelson R Mandela School of Medicine, University of Kwa-Zulu Natal, Albert Luthuli Academic Hospital, Durban, South Africa
XXIIIMB ChB, FCA (SA); Department of Anaesthesiology, Steve Biko Academic Hospital, University of Pretoria, South Africa
XXIVMB ChB, FCA (SA); Department of Anaesthesia, University of the Free State, Universitas Hospital, Bloemfontein, South Africa
XXVMB ChB, Mmed (Anaes); Department of Anaesthesia, University of the Free State, Universitas Hospital, Bloemfontein, South Africa
XXVIMB ChB, PhD; Department of Anaesthesia and Perioperative Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
XXVIIMB ChB, PhD; Department of Anaesthesia and Perioperative Medicine, Groote Schuur Hospital, Cape Town, South Africa
ABSTRACT
BACKGROUND: Low- and middle-income countries have a critical shortage of specialist anaesthetists. Most patients arriving for surgery are of low perioperative risk. Without immediate access to preoperative specialist care, an appropriate interim strategy may be to ensure that only high-risk patients are seen preoperatively by a specialist. Matching human resources to the burden of disease with a nurse-administered pre-operative screening tool to identify high-risk patients who might benefit from specialist review prior to the day of surgery may be an effective strategy
OBJECTIVE: To develop a nurse-administered preoperative anaesthesia screening tool to identify patients who would most likely benefit from a specialist review before the day of surgery, and those patients who could safely be seen by the anaesthetist on the day of surgery. This would ensure adequate time for optimisation of high-risk patients preoperatively and limit avoidable day-of-surgery cancellations
METHODS: A systematic review was conducted to identify preoperative screening questions for use in a three-round Delphi consensus process. A panel of 16 experienced full-time clinical anaesthetists representing all university-affiliated anaesthesia departments in South Africa participated to define a nurses' screening tool for preoperative assessment
RESULTS: Ninety-eight studies were identified, which generated 79 questions. An additional 14 items identified by the facilitators were added to create a list of 93 questions for the first round. The final screening tool consisted of 81 questions, of which 37 were deemed critical to identify patients who should be seen by a specialist prior to the day of surgery
CONCLUSION: A structured nurse-administered preoperative screening tool is proposed to identify high-risk patients who are likely to benefit from a timely preoperative specialist anaesthetist review to avoid cancellation on the day of surgery
Low- and middle-income countries perform too few surgeries.[1] Access to theatre is partly limited by human resource constraints, which include a critical shortage of specialists.[2] Despite the limited number of surgeries in low-resource environments, not all high-risk patients are seen timeously prior to surgery to modify risk. This is partly due to the limited number of anaesthetists. Nearly 80% of patients presenting for surgery in low- and middle-income countries are of a low perioperative risk, yet not all of the remaining high-risk patients are seen by a specialist anaesthetist.[3]
Hypothesis
Low-risk patients are unlikely to be cancelled on the day of surgery because of health-related issues, and thus do not require assessment by an anaesthetist until the day of surgery. Patients with an elevated risk, and those with modifiable risk factors, are more likely to benefit from a specialist anaesthesia review and preoperative optimisation. A critical shortage of specialist anaesthetists leads to a significant proportion of high-risk patients not being timeously and appropriately assessed preoperatively. Additionally, a lack of a simple triage/screening system to differentiate the low- and high-risk patients leads to an inappropriate review of low-risk patients by specialists.
Without immediate preoperative access to specialist anaesthesia care for all patients, an appropriate interim strategy may be to ensure that only high-risk patients are seen by a specialist. Task-sharing of the preoperative assessment process by nurses and anaesthetists could increase the effectiveness of the available human resources.
By matching human resources to the patient's burden of disease with a nurse-administered preoperative anaesthesia screening tool, we may be able to identify all high-risk patients who might benefit from specialist review prior to the day of surgery. This may be an effective strategy to ensure appropriate allocation of human resources.
Objectives
The primary objective of the study was to develop a nurse-administered preoperative anaesthaesia screening tool to identify patients who would most likely benefit from a specialist review before the day of surgery, and those patients who could safely be seen by the anaesthetist on the day of surgery. This would ensure adequate time for optimisation of high-risk patients preoperatively, and limit avoidable day-of-surgery cancellations.
Methods
Question generation for Delphi consensus process
A systematic review of published preoperative screening tools was conducted on 5 August 2017. The search is shown in the appendix (http://samedical.org/file/2160).
The search of PubMed, Scopus and EBSCOhost generated 899 references. These were screened to include only human studies, patients in the preoperative setting undergoing non-cardiac or non-obstetric surgery and studies involving a risk stratification tool or questionnaire. Review and duplicate articles were excluded. Ninety-eight studies were identified (appendix S2) and used to generate a list of 79 screening items which were then categorised into 10 domains (appendix S3).
The Delphi study was approved by the Human Research Ethics Committee of the Faculty of Health Sciences, University of Cape Town (ref. no. HREC 841/2019). All participants consented to participation in the process and were invited to be co-authors of the manuscript. The Conducting and REporting of DElphi Studies (CREDES) was used as a reporting guideline[4] (appendix S4).
Panel selection
Heads of anaesthesia departments (HODs) at all eight of the universities in South Africa (SA) were asked to nominate two members of their department to participate in the study who fulfilled the following criteria: (i) clinical experience of at least 5 years post specialist examinations; (ii) strong general clinical ability coupled with up-to-date academic knowledge; and (iii) a willingness to participate and communicate their point of view.
Delphi process
Stage 1: Establishing a preliminary list of questions to be included for round 1: A further 14 items were added by the facilitators (MN and BB) to the 79 items identified in the systematic review (Supplementary material S5,6).
Stage 2: Delphi round 1: The list of questions was recorded on an Excel for Mac (version 16.53; Microsoft, USA) spreadsheet and emailed to the participating anaesthetists for formal rating of the components. They were asked to rate the importance of a particular component on a 9-point Likert scale, where 1 was considered as least important and 9 most important. Guidance on categorising the items was given to the panel (Table 1).
The panel was instructed to provide comments related to any of the components, as well as propose any additional questions that they thought were important and not included.
Stage 3: Processing of round 1: The questions and responses were transcribed onto Google Sheets and categorised into one of three categories (unimportant, important or critical) based on the median response score calculated for each question. Consensus criteria for categorisation was set at 75%, 95% confidence interval 53.8 - 96.2 (12/16 panel members needed to agree on the categorisation). Items where consensus was reached for 'low importance' were removed from subsequent rounds and not included in the proposed tool. Items with consensus for 'important' and 'critical' would be included in the screening tool.
Stage 4: Delphi round 2: Each panel member received individual Google Sheets with the list of questions and their median scores. The panel were asked to consider re-ranking those items that did not reach the 75% majority, and also to score the newly suggested items.
Stage 5: Processing of round 2: Questions considered similar or duplicates by the panel were amalgamated. Questions achieving consensus for 'low importance' were removed. Following round 2, the facilitators prepared the remaining set of questions for round 3 panel discussion.
Stage 6: Delphi round 3 and final consensus: The list of 'important' and 'critical' questions where consensus was reached was circulated to the panel 3 days prior to the scheduled online Zoom meeting. The recorded meeting was chaired and facilitated by MN and BB, during which all the questions and their median score were presented for discussion. The facilitators' role was to move the group to a consensus position and categorise each item into one of the three categories. Panel members were able to raise their views verbally as well as via the chat forum. Categorisation of each question was concluded by majority decision (75%). If consensus was not reached, the default position was to adopt a more conservative strategy and include questions at the higher category. Thus, if a small cohort of panel members believed that the item was 'critical', but the view was not shared by 75% of the group, it would still have been included as a 'critical' item. The results of the final Delphi round were circulated by email to the panel for final approval to ensure that it reflected the views of all the panel members.
Results
Ninety-eight studies identified in the systematic review generated 79 questions. An additional 14 questions were added by the facilitators to create a list of 93 items (appendix S6) for round 1 of the Delphi process. New panel-proposed items from rounds 1 and 2 are included in appendix S7. The results of the individual questions for rounds 1 and 2 are listed in appendix S8.
The selected panel for the Delphi process included 16 anaesthetists with a mean (standard deviation) specialist work experience of 14.9 (6.5) years. Five of the eight university HODs were part of the panel.
The summary of the Delphi rounds is shown in Fig. 1.
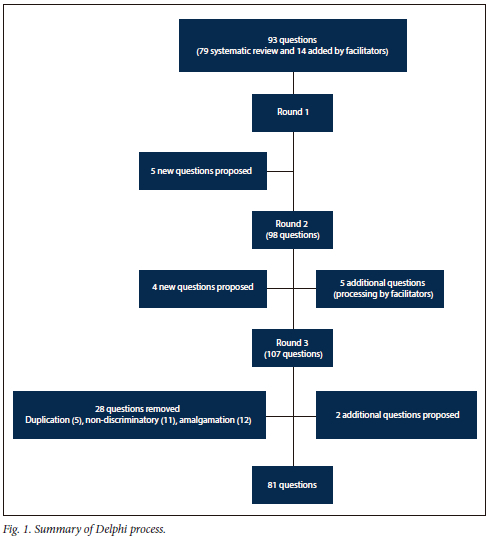
Fourteen of the 16 panel members attended the round 3 online meeting. The other two members subsequently made comments, reviewed the final questions and agreed with the consensus reached.
The facilitators' role during round 3 was to move the panel towards consensus on items not reached during round 2. Importantly, the aim of the final round was to create a questionnaire that would identify only the high-risk patients needing review before the day of surgery. To avoid inclusion of low-risk patients needing review before the day of surgery, the facilitators also proposed that certain questions despite consensus categorisation as 'critical' during round 2 be discussed and be possibly recategorised as 'important' (appendix S9).
At the conclusion of the Delphi process, the Nurses' Preoperative Screening Tool included 81 items, of which 37 were critical, which identified patients who should be seen by a specialist prior to the day of surgery, and 44 important questions were also identified. The final Nurses' Preoperative Screening Tool is shown in Table 2.
Discussion
The principal outcome of the study is an agreed-upon structured preoperative screening tool that can be administered by a nurse to identify high-risk patients who may benefit from a specialist review prior to the day of surgery. The tool also identifies clinically important information that may affect perioperative care but would be unlikely to result in a cancellation on the day of surgery.
The study had several strengths. The proposed questions for inclusion in the Delphi consensus process were derived from a systematic review. The Delphi panel was experienced, with an individual average of 15 years as a specialist anaesthetist. Importantly, there was strong national support for the study, with five HODs on the panel and all eight academic anaesthesia departments in SA represented. The specialists on the panel care for patients across SA, which includes a population spectrum of diverse health literacy and economic status. It is therefore likely that the tool may have utility across all levels of healthcare. Its use in remote rural settings where access to healthcare resources is often limited would need to be tested.
The following limitations of the study were identified. Nurses for whom the tool is intended were not included in the Delphi process. Testing the clinical applicability and nurse acceptability will be explored in subsequent studies, but nurse-led pre-operative assessment clinics are not novel.[5,6] Another limitation was the absence of specialist anaesthetists from private practice on the Delphi panel. Although the motivation behind the study was the extreme shortage of anaesthetists in the state sector, and identifying strategies to optimise specialist time through task-sharing of screening by nurses, and even though the majority of the panel has some degree of private practice experience, the authors acknowledge that colleagues in private practice could have contributed intellectual and sector-specific information. This may well have enhanced the validity and possible uptake of the questionnaire. Future work with the private sector through the SA Society of Anaesthesiologists may attract participation in the testing, refinement and validation of the tool for a broader SA context.
The risk of a bandwagon effect with Delphi participants going along with the majority opinion was not assessed. Pursuing group consensus through the display of median scores and group categorisation increases the tradeoff between accuracy and consensus.[7] The study mitigated the risk through: (i) anonymity in the first two rounds; (ii) intermediate cohesiveness of the group (panel of expert with some degree of heterogeneity influenced by their local factors); (iii) online meeting, which may be associated with less social pressure than a face-to-face meeting (speculative); and (iv) filtered feedback by facilitators in exploring minority/divergent points of view in the final round. Amalgamation of questions, directing of discussions and drive toward consensus with the aim of finding a practical and appropriate tool may have been subject to facilitator bias. However, to limit facilitator bias, we used two facilitators, who were sensitive in exploring every individual opinion and searching for a group consensus during the online meeting. The online meeting was recorded and reviewed, and results of the final round were circulated to all members, with unanimous approval of the final document. This may support the view that the facilitators did not have undue influence on the process, although this was not objectively assessed.
The tool has many questions, which may detract from its use. Some questions may not be easily and consistently interpretable. One such question, about the level of surgical risk, may be difficult to quantify for doctors as well as nurses for whom the tool was intended. Adding a list of surgeries that accompanies the questionnaire where the risk of major adverse cardiac events (MACE) is low (<1%), intermediate (1 - 5%) and high (>5%) could assist in answering the question.
The study does not offer any new paradigm shifts or novel screening strategies. Its intention was to identify and formalise a set of screening items, through a process of consensus, to identify high-risk patients who may likely benefit from a specialist review prior to the day of surgery.
The study has several potential positive consequences that need to be tested. These include the appropriate referral of high-risk patients and subsequent decrease in cancellation rates, better resource allocation of specialist services by avoiding unnecessary review of low-risk patients, and nurse empowerment and upskilling to improve the level of peri-operative care. Finally, the screening tool may become an adaptable foundation for use in a preoperative assessment clinic and a bridge to education and treatment strategies in targeting chronic conditions such as diabetes, hypertension and anaemia.
Future work will focus on prospective validation of the tool and contextual adaptation into different health systems. Poorly performing questions with low predictive value for cancellation can be identified and removed to streamline the screening process.
Declaration. This is a substudy of a PhD protocol: Preoperative evaluation and optimisation in a resource-limited environment. PhD candidate: MB Nejthardt.
Acknowledgements. The corresponding author wishes to thank Mr Pierre de Villiers (Boston, USA) for his assistance with Excel spreadsheet and Google Sheet form development.
Author contributions. Study concept: BB. Protocol development: MN, BB. Systematic review: MN, FR, FB, BB. Participation in the Delphi survey: all authors except FR and FB. Analysis of the responses: MN, BB. First draft and revision of manuscript: MN, BB. Critical review and revisions of the manuscript: all authors.
Funding. None.
Conflicts of interest. None.
References
1. Meara JG, Leather AJ, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet 2015;386(9993):569-624. https://doi.org/10.1016/S0140-6736(15)60160-X [ Links ]
2. Kempthorne P, Morriss WW, Mellin-Olsen J, Gore-Booth J. The WFSA Global Anesthesia Workforce Survey. Anesth Analg 2017;125(3):981-990. https://doi.org/10.1213/ane.0000000000002258 [ Links ]
3. Biccard BM, Madiba TE, Kluyts HL, et al. Perioperative patient outcomes in the African Surgical Outcomes Study: A 7-day prospective observational cohort study. Lancet 2018;391(10130):1589-1598. https://doi.org/10.1016/s0140-6736(18)30001-1 [ Links ]
4. Junger S, Payne SA, Brine J, Radbruch L, Brearley SG. Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care: Recommendations based on a methodological systematic review. Palliat Med 2017;31(8):684-706. https://doi.org/10.1177/0269216317690685 [ Links ]
5. Arun N, Al-Jaham KMA, Alhebail SA, et al. Nurse-run preanaesthesia assessment clinics: An initiative towards improving the quality of perioperative care at the ambulatory care centre. BMJ Open Qual 2021;10:e001066. https://doi.org/10.1136/bmjoq-2020-001066 [ Links ]
6. Nicholson A, Coldwell CH, Lewis SR, Smith AF. Nurse-led versus doctor-led pre-operative assessment for elective surgical patients requiring regional or general anaesthesia. Cochrane Database Syst Rev 2013(11):Cd010160. https://doi.org/10.1002/14651858.cd010160.pub2 [ Links ]
7. Winkler J, Moser R. Biases in future-orientated Delphi studies: A cognitive perspective. Technol Forecasting Soc Change 2016;105:63-76. https://doi.org/10.1016/j.techfore.2016.01.021 [ Links ]
 Correspondence:
Correspondence:
M B Nejthardt
mb.nejthardt@uct.ac.za
Accepted 5 November 2023














