Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 no.12 Pretoria dic. 2023
http://dx.doi.org/10.7196/samj.2023.v113i12.1171
RESEARCH
Knowledge, attitudes and practices of oral HIV pre-exposure prophylaxis (PrEP) among healthcare workers in the Ekurhuleni District, South Africa
E MahlareI; E RamutshilaII; A MusekiwaIII; L KuonzaIV; T MabutoV
IMSc; School of Health Systems and Public Health, Faculty of Health Sciences, University of Pretoria, South Africa
IIMPH; South African Field Epidemiology Training Program, National Institute for Communicable Diseases, Johannesburg, South Africa
IIIPhD; School of Health Systems and Public Health, Faculty of Health Sciences, University of Pretoria, South Africa
IVMB ChB, MPH; School of Health Systems and Public Health, Faculty of Health Sciences, University of Pretoria, South Africa
VPhD; The Aurum Institute, Johannesburg, South Africa
ABSTRACT
BACKGROUND: Prevention of new HIV infections is crucial for controlling the HIV epidemic. Despite HIV pre-exposure prophylaxis (PrEP) being one of the highly effective approaches to preventing HIV, and being freely available through primary healthcare clinics (PHCs), the uptake of HIV PrEP in South Africa (SA) is low
OBJECTIVE: To understand knowledge, attitudes and practices (KAPs) of healthcare workers responsible for generating demand for HIV PrEP services, or identifying clients eligible for HIV PrEP services in PHCs in Ekurhuleni District, South Africa
METHODS: We conducted a cross-sectional interviewer-administered survey among healthcare workers from 45 randomly selected PHCs in Ekurhuleni District. We collected information on participant characteristics and their KAPs regarding HIV PrEP service delivery. KAP scores were developed using a priori cut-off points and participants were categorised into binary levels of KAPs. We performed descriptive and multivariable logistic regression analysis in line with the study objectives
RESULTS: We enrolled 160 study participants from 1 May to 30 June 2022. About two-thirds of the participants (64.4%) were highly knowledgeable about HIV PrEP, and 58.1% self-reported practices that were considered to be good. Notably, 73.1% of participants had negative attitudes toward HIV PrEP delivery. Participants who were aged >50 years had poor HIV PrEP knowledge (adjusted odds ratio (aOR) 0.1; 95% confidence interval (CI) 0.0 - 0.4; p=0.01) compared with participants <30 years old. Participants aged 30 - 40 years had poor HIV knowledge although their association is not statistically significant. Nurses had higher HIV PrEP knowledge (aOR 11.1; 95% CI 3.8 - 32.4, p<0.001) compared with health promoters. Both nurses (aOR=0.2, 95% CI 0.1 - 0.6; p<0.001) and HIV testing service counsellors (aOR 0.3; 95% CI 0.1 - 0.9; p=0.02) had negative attitudes toward HIV PrEP, compared with health promoters. Nurses had better practices in HIV PrEP delivery compared with health promoters (aOR 2.5; 95% CI 1.0 - 5.9; p=0.04
CONCLUSION: Among the healthcare workers tasked with generating demand and identifying clients eligible for HIV PrEP services, low knowledge of HIV PrEP and negative attitudes towards HIV PrEP may be barriers to the uptake of HIV PrEP. Training healthcare workers on HIV PrEP is recommended
The HIV epidemic remains a global public health threat, despite the gains that have been made over the years to reduce the number of new infections. In 2021, about 1.5 million people were newly infected with HIV worldwide.[1] This suggests that the global public health response is not on course to meet the targets set by the Joint United Nations Programme on HIV/AIDS (UNAIDS)[2] of 370 000 new infections per year by 2025. Instead, it is projected that at the current observed rates, the number of new HIV infections in 2025 will treble the anticipated target.[1]
Globally, sub-Saharan Africa (SSA) accounts for the majority of new HIV infections. In 2021, 59% of new HIV infections were from SSA.[1] Notably, about 210 000 out of the 885 000 (24%) new HIV infections in SSA were from South Africa (SA),[2] where the HIV epidemic is generalised. However, certain highly vulnerable populations, such as adolescent girls and young women (AGYW), sex workers, men who have sex with men (MSM) and people who use drugs (PWUD) have a disproportionately high number of new HIV infections.[3] Importantly, SA had a goal of reducing the number of new infections to 100 000 per year by the end of 2022.[4] However, this goal remains out of reach based on the current rates of HIV incidence decline in the country.[1]
The slow decline in HIV incidence in SA points to a need for efforts to strengthen HIV prevention. HIV pre-exposure prophylaxis (PrEP) is one of the tools in the HIV prevention toolbox that reduces the risk of HIV acquisition in HIV-negative individuals.[5] HIV PrEP works by preventing HIV from replicating in the body, and may reduce the risk of HIV acquisition from sexual intercourse by ~99% when taken as prescribed.[5] In this regard, PrEP shifts the focus of control to people who are HIV-negative. For example, the use of HIV PrEP assists vulnerable AGYW to take control of their sexual lives in a situation where negotiating for condom use is difficult.[6]
According to SA's national guidelines for HIV PrEP, the populations at substantial risk of HIV infection that are eligible for PrEP include sex workers, adolescent girls, young women, MSM, serodiscordant couples, people with multiple sexual partners, people with a recent history of sexually transmitted infection, PWUD and those who request PrEP.[5] The eligibility criteria for PrEP include willingness to take PrEP as prescribed, an HIV-negative routine antibody test, absence of symptoms of acute HIV infection (e.g. sore glands, fever or oesophageal Candida), no contraindications to antiretroviral medication (ARVs) used for PrEP and being of recommended age and body weight if <15 years of age.[5] The SA National Department
of Health (NDoH) started the routine delivery of oral HIV PrEP in 2016, and by 2020, implementation had been scaled up to all primary healthcare clinics (PHCs). In SA, HIV PrEP medications in PHCs are currently available in tablet form and taken orally (i.e. oral HIV PrEP). Although the World Health Organization recommended the use of injectable cabotegravir (CAB) for PrEP as an additional HIV prevention method in July 2022,[7] currently the CAB injection for PrEP is not used in PHCs in SA. Despite HIV PrEP being shown to be highly effective in preventing HIV, and being freely available through PHCs, the uptake of HIV PrEP in SA is low. Findings from the mid-term review of SA's National Strategic Plan on HIV, TB and STIs (NSP) 2017 - 2022 estimate uptake of 29% across all PrEP implementing sites.[4] In Ekurhuleni District, Gauteng Province, where this study was conducted, a similar picture of low uptake emerges from routine programme data. In particular, of the district's annual target of 36 953 PrEP initiations, the PHCs only managed 12 919 initiations (35% of the target).[8] Some of the reasons for the low uptake of PrEP could be the stigma that surrounds ARVs, such as beliefs that ARVs are only for HIVpositive individuals.[9]
The reach and uptake of PrEP services are highly dependent on the extent to which healthcare workers offer and deliver PrEP services. Although there may be multilevel factors influencing the observed low uptake of HIV PrEP in SA, there is little known about the knowledge, attitudes and practices (KAPs) of healthcare workers concerning HIV PrEP delivery in Ekurhuleni District PHCs. Understanding the healthcare workers' KAPs concerning oral HIV PrEP may assist in identifying barriers amenable to low-cost interventions that may significantly improve HIV PrEP uptake.
Optimal delivery of HIV PrEP services to people who are at substantial risk of acquiring HIV infection will require healthcare workers to be willing to support HIV PrEP service delivery.[10- This study explores potential barriers at the healthcare worker level (i.e. KAPs) that may be addressed to improve the offering and delivery of HIV PrEP, which may increase the uptake of PrEP.
Methods
Study design
We conducted a cross-sectional study to describe KAPs concerning HIV PrEP among healthcare workers in PHCs of Ekurhuleni District. The study was conducted between 1 May and 30 June 2022.
Study setting
This study was conducted in Ekurhuleni District, located in Gauteng Province of SA. This district is one of the five districts of Gauteng Province, with an estimated population of >3.3 million people.[8] The district has three regions, namely the Ekurhuleni East Service Delivery Region, the Ekurhuleni North Service Delivery Region and the Ekurhuleni South Service Delivery Region. The district has a total of 78 PHC facilities; of these, 26 are in Ekurhuleni East, 23 in Ekurhuleni North and 29 in Ekurhuleni South. In this study, we included 45 PHCs randomly selected from all three regions in Ekurhuleni District.
Study population
The study population comprised healthcare workers involved in HIV PrEP service delivery in all the PHCs in Ekurhuleni District. In particular, we sought to include healthcare workers responsible for generating demand for HIV PrEP services or identifying clients eligible for HIV PrEP services. The SA National PrEP guidelinesstipulates who is responsible and how demand creation must be conducted.
Inclusion criteria
We included professional nurses, HIV testing service (HTS) counsellors, and health promoters aged >18 years and working in the randomly selected 45 PHCs in Ekurhuleni District.
Exclusion criteria
We excluded sessional doctors, pharmacists, pharmacist assistants and data capturers in the selected PHC facilities. These healthcare workers were not responsible for generating demand for HIV PrEP services, nor identifying clients eligible for HIV PrEP services.
Study size and sampling
We used a sampling frame of 78 PHCs in Ekurhuleni District, and conducted simple random sampling to select 15 facilities from each of the three subdistricts (i.e. 45 facilities in total). The sample size was calculated using Epi Info (Centers for Disease Control and Prevention, USA) software. Since the level of KAPs of healthcare workers regarding the provision of PrEP was unknown, we assumed it was 50%, a proportion that also gave the maximum sample size. Therefore, assuming a population of 225 healthcare workers (15 facilities from each region, each with an average of 5 healthcare workers), a 5% level of significance and a margin of error of 5% for 95% confidence intervals (CIs), a minimum sample size of 142 was required.
We selected three healthcare workers in each PHC, and those who were available and willing to participate in the study were included.
Measurements Data collection
Data were collected using a paper-based questionnaire, which was specifically designed for this survey. The draft questionnaire was piloted at the Ekurhuleni District TB/HIV Unit among six conveniently selected respondents to assess validity and reliability. It was adjusted because of the errors that were identified during pre-testing. The questionnaire was only available in English and the meanings of medical terms were explained by the interviewer during the interview session.
The questionnaire (Appendix 1: https://www.samedical.org/file/2145) was interviewer-administered through one-on-one interviews with healthcare workers. The principal investigator, who is not related to any of the study participants, carried out all the interviews. The questionnaire included Likert-type and multiple-choice questions. A total of 30 questions were included in the questionnaire, and the questions were divided into four sections. Section A had eight questions that were used to collect the demographic information of the participants; section B had nine questions that were used to assess the knowledge; section C had four Likert-type questions that were used to assess the attitudes and section D had nine questions that were used to assess the practices of study participants regarding the HIV PrEP at their PHCs.
Variables
The demographic characteristics of healthcare workers included age, gender, type of occupation, region, PrEP training and work experience. KAP scores were given according to the responses from questionnaires. Explanatory variables were the demographic characteristics of the participants, and the outcome variables were KAP scores.
Data management and analysis
Data collected using the paper questionnaire were captured in Excel (Microsoft Corp., USA). The data were assessed for completeness, duplicates, missing data and the logic of information. The Excel spreadsheet was imported into STATA version 17 (StataCorp, USA) software for analysis.
To describe the characteristics of healthcare workers, we summarised numerical data using medians and interquartile ranges (IQRs). Categorical variables were summarised using absolute numbers and percentages.
The KAP scores were defined as good or poor based on adapted Bloom's cut-off points.[11] Each of the nine knowledge questions was scored 1 if the answer was correct or 0 if incorrect. Therefore, the knowledge score ranged from a minimum of zero to a maximum of nine. Participants who got a score of <5 (i.e. <60%) were classified as having low knowledge. Participants who got a score of >5 (i.e. >60%) were categorised as having high knowledge.
Each of the four attitude questions was scored 1 if the answer reflected a positive attitude or 0 if it reflected a negative attitude. Therefore, the attitude score ranged from a minimum of zero to a maximum of four. Participants who got a score of <2 (i.e. <50%) were categorised as having negative attitudes towards HIV PrEP service delivery. Participants who got a score of >2 (i.e. >50%) were categorised as having positive attitudes towards HIV PrEP service delivery.
Each of the nine practice questions was scored 1 if the answer reflected a good practice or 0 if it reflected a poor practice. Therefore, the practice score ranged from a minimum of zero to a maximum of nine. Participants who got a score of <5 (i.e. <60%) were categorised as having poor practices in HIV PrEP service delivery. Participants who got a score of >5 (i.e. >60%) were categorised as having good practices in HIV PrEP service delivery.
Descriptive statistics were used to summarise KAP scores. Categorical responses were summarised using bar charts and frequency tables showing counts and percentages. The median and IQR were reported for KAPs. Association between KAP and participant characteristics we assessed using the χ2 test.[12] A p-value <0.05 was considered statistically significant. We conducted univariable logistic regression and proceeded to multivariable analysis using explanatory variables with p<0.25.[13] At the multivariable stage, variables with p<0.05 were considered statistically significant.
Ethical considerations
The ethical approval for the study was received from the University of Pretoria Faculty of Health Sciences Research Ethics Committee (HSREC) (ref. no. 20/2020) and Ekurhuleni District Health Research Committee (ref. no. GP_202205_014).
The information sheet explaining the purpose and the benefits of the study was given to and discussed with the participants before administering the questionnaire. Information that participation is voluntary was given to participants, and they were requested to sign the consent form before the interview. The unique identifying record numbers on the questionnaire were used for each participant to ensure anonymity. The completed paper-based questionnaires were locked in a cupboard that is accessible to the primary investigator and the supervisory team. The data were stored on a password-protected computer to ensure confidentiality.
Results
Participant characteristics
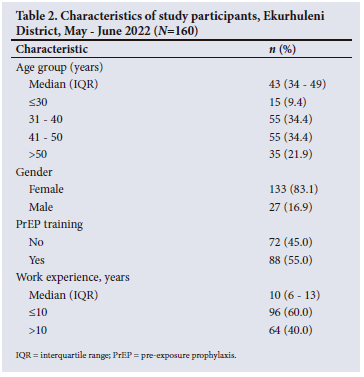
From 1 May to 30 June 2022, a total of 160 study participants were enrolled in the study. We enrolled more participants in larger PHCs that had a higher number of healthcare workers eligible to participate in the study. The participants interviewed were evenly distributed across the three regions, and by job category (Table 1).
The median (IQR) age of participants was 43 (34 - 49) years, and most (83.1%) were female. Most participants had worked for <10 years, and just over half had been trained in HIV PrEP (Table 2).
Participant responses to questions on their knowledge about HIV PrEP
Participants were most knowledgeable on how to select the correct definition of HIV PrEP as ARVs taken by HIV-negative persons before exposure to HIV, with 86% of participants providing a correct response to the question. Over half (58%) of the participants also knew the current PrEP regimen and the content for follow-up talks among people on PrEP (51%). However, for the remainder of the six other knowledge areas assessed in this study, less than half of the participants provided a correct answer. Notably, participants were least knowledgeable about the full eligibility criteria for offering PrEP, with only 18% responding to the question (Fig. 1).
Participant responses to attitude questions on HIV PrEP
One in five participants (20%) did not agree or strongly agree that the rollout of HIV PrEP was a good decision. In addition, half (50%) of the participants were neutral or agreed that the delivery of HIV PrEP was overburdening healthcare workers. Only 41% of the participants disagreed or strongly disagreed that HIV PrEP promotes risky sexual behaviour. Lastly, the majority of participants were either neutral or agreed to some extent that the use of HIV PrEP reduces condom use (Fig. 2).
Participant responses to questions on their practices in HIV PrEP delivery
Overall, most participants reported good practices in the delivery of HIV PrEP services, and as many as 91% of participants reported giving health education on HIV PrEP in their facilities. The least reported practices recommended for HIV PrEP service delivery were the follow-up of clients using PrEP (28%), the displaying of PrEP counselling job aids (31%) and displaying of the PrEP algorithm (36%) (Fig. 3).
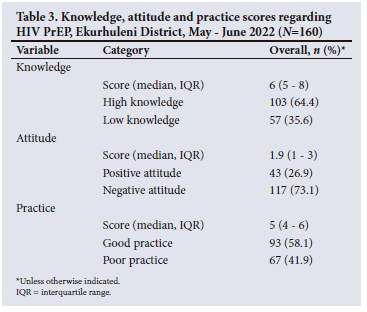
Knowledge, attitude and practice scores
Of the nine knowledge questions, the median (IQR) HIV PrEP knowledge score for the study sample was 6 (5 - 8). About two-thirds (64.4%) of the participants were highly knowledgeable about HIV PrEP. Of the four attitude questions, the median (IQR) HIV PrEP attitude score was 1.9 (1 - 3). Notably, most participants (73.1%) displayed negative attitudes towards HIV PrEP service delivery. Of the nine practice questions, the median (IQR) HIV PrEP practice score was 5 (4 - 6). Over half (58.1%) of the participants reported good practices in HIV PrEP delivery (Table 3).
Factors associated with level of knowledge about HIV PrEP
In univariable analysis, there was strong evidence that age group and occupation were associated with a high level of knowledge. Participants who were aged >50 years had lower odds of high HIV PrEP knowledge (odds ratio (OR) 0.1, 95% CI 0.0 - 0.7) compared with participants <30 years old. Nurses had higher odds of having high HIV PrEP knowledge (OR 8.4, 95% CI 3.2 - 22.0) compared with health promoters (Table 4).
In the multivariable analyses, participants in the age group 41 - 50 years (adjusted odds ratio (aOR) 0.1, 95% CI 0.0 - 0.8) and those aged >50 years (aOR 0.1, 95% CI 0.0 - 0.4) had lower odds of having high HIV PrEP knowledge compared with participants <30 years old. The association between occupation and HIV PrEP knowledge was maintained in multivariable analysis. Nurses had higher odds of having high HIV PrEP knowledge (aOR 11.1, 95% CI 3.8 - 32.4) compared with health promoters (Table 4).
Factors associated with level of attitude towards HIV PrEP
In univariable analysis, there was strong evidence of the association between occupation and high attitude scores. Compared with health promoters, HTS counsellors (OR 0.4, 95% CI 0.2 - 0.9) and nurses (OR 0.3, 95% CI 0.1 - 0.7) had negative attitudes towards HIV PrEP (Table 5).
The association between occupation and HIV PrEP attitude was maintained in multivariable analysis. Compared with health promoters, HTS counsellors (aOR 0.3, 95% CI 0.1 - 0.9) and nurses (aOR 0.2, 95% CI0.1 - 0.6) had negative attitudes toward HIV PrEP. There was no strong evidence of any association between participants' age group and level of attitude towards PrEP (Table 5).
Factors associated with level of practice in HIV PrEP delivery
In univariable analysis, there was no strong evidence of any associations between the measured participant characteristics and good PrEP delivery practices. Notably, there was some evidence, although weak, suggesting that nurses had higher odds of good practices compared with health promoters (OR 2.2, 95% CI 0.9 - 4.7) (Table 6).
In multivariable analysis (compared with univariable analysis) there was stronger evidence of nurses having higher odds of performing good practices in HIV PrEP delivery compared with health promoters (aOR 2.5, 95% CI 1.0 - 5.9) (Table 6).
Discussion
The low uptake of HIV PrEP in high HIV-burden districts, such as Ekurhuleni District, has impeded the goal of reaching <100 000 new infections per year in SA by the end of 2022.[4] Our study identified healthcare worker KAPs that may act as barriers to optimum HIV PrEP uptake. Among the healthcare workers tasked with generating demand and identifying clients eligible for HIV PrEP services, low knowledge of HIV PrEP and negative attitudes to HIV PrEP may be barriers to the offer and enrolment of eligible clients on HIV PrEP.
We found that participants had the least knowledge of issues that are critical to their roles of generating demand and identifying clients eligible for ART. While the overall HIV knowledge scores suggest that about two-thirds of participants were highly knowledgeable about HIV PrEP, participants had very low knowledge of aspects critical to increasing the uptake of HIV PrEP. Notably, just over a third of participants knew the target populations for HIV PrEP, and <2 in 10 participants knew the full PrEP eligibility criteria. These deficiencies are significant barriers to optimising the reach of HIV PrEP services to those who need them. Several studies in other programmes outside of HIV PrEP have shown how low knowledge of target populations and eligibility criteria influence the reach and uptake of services.[13-19]
Health behaviour models such as the Information Motivation Behaviour Model and the Capability Opportunity Motivation and Behavior Model (COM-B) underscore the importance of training and capacity building to achieve the required behaviours to implement health interventions.[20,21] Of concern is that only about 45% of the healthcare workers tasked with generating demand and identifying people eligible for PrEP had received formal HIV PrEP training. However, our findings showed that there were no differences in the level of HIV PrEP knowledge between those who were trained and those who were not formally trained. The similarity in the level of HIV PrEP knowledge between the trained and untrained participants may point to informal training approaches that are used in the clinics, which provide some level of knowledge to healthcare workers who are not formally trained. While we did not explore the reasons for healthcare workers not being trained, it is plausible that some of the reasons may be linked to high staff turnover or rotation of staff roles within PHCs.[20,21]
Our findings may also point to the quality of training, and gaps in post-training interventions such as mentoring. Evidence from other studies has shown increases in HIV PrEP knowledge.[22-25] A 2020 study conducted in Uganda showed improvements in HIV PrEP knowledge after training interventions.[26] In light of our findings and available evidence in the literature, we hypothesise that there may be gaps in how capacity is built and maintained to support HIV PrEP delivery in Ekurhuleni District PHCs.
Our findings showing lower odds of high HIV PrEP knowledge for participants >40 years compared with those <30 years may reflect the use of different information sources, e.g. social media as compared with mainstream sources. These findings are similar to those reported by Wood et al.[10] in a study conducted in Washington. The study found that younger healthcare workers were more knowledgeable about HIV PrEP compared with older healthcare workers.[10] These findings may reflect the ability of young healthcare workers to adapt to the constantly upgraded HIV management protocols.
We also found that nurses had higher odds of having high HIV PrEP knowledge compared with health promoters, while there were no differences in knowledge between health promoters and HTS counsellors. Similar to studies conducted by Sammons et al.[24] and Moore et al.,[23] greater technical expertise was associated with being more knowledgeable about HIV PrEP. While this is encouraging to some extent, our findings may be suggestive of the need to tailor HIV PrEP training activities to health promoters and HTS counsellors who may be less technically inclined compared with nurses. In addition to adapting the training approaches, these groups of healthcare workers may also require more post-training support compared with nurses. Further, nurses can also be tasked with mentoring other healthcare workers in their facilities, or reducing knowledge gaps.
The high proportion of participants with negative attitudes towards HIV PrEP is a concerning finding for a programme that has been in operation for 3 years now and is critical to reducing the number of new infections in SA. Although most participants agreed that the PrEP rollout was a good decision, there were major concerns about the effects of encouraging riskier sexual behaviours and eroding the progress that had been made to improve consistent condom use. Our findings are similar to those of studies conducted in Rwanda, SA, Tanzania, and the USA.[22,27,28] Although there is limited evidence on the impact of HIV PrEP on risk-taking, some studies have reported increases in risk behaviour in the context of HIV 'treatment as prevention'.[29] It is plausible that people taking HIV PrEP may reduce their self-constraint when indulging in high-risk sexual behaviours, and view HIV PrEP as a substitute for exercising behavioural control (i.e. behavioural disinhibition), or may see unprotected sex as an acceptable risk when they are taking HIV PrEP (i.e. risk compensation).[31] Although these concerns may be justified, healthcare workers have additional tools to provide health communication and counselling services to minimise behavioural disinhibition and risk compensation. Root cause analyses may be required to understand the factors that drive these concerns among healthcare workers.
We identified opportunities to align knowledge of HIV PrEP and attitudes toward HIV PrEP delivery. Firstly, although nurses were highly knowledgeable about HIV PrEP, they had lower odds of possessing good attitudes towards HIV PrEP delivery. On the other hand, health promoters had lower knowledge of HIV PrEP but had higher odds of possessing good attitudes toward HIV PrEP delivery. HTS counsellors were positioned in between: they did not stand out in possessing higher knowledge, and had levels of negative attitudes similar to the nurses. Our findings point to the need for tailored approaches to the different groups of healthcare workers tasked with generating demand and identifying people eligible for HIV PrEP.
In our study, only half of the participants implemented good practices of HIV PrEP service. This might be influenced by the different roles and responsibilities among healthcare workers. In particular, nurses had higher odds of self-reporting good practices of HIV PrEP delivery compared with other healthcare workers. Similarly, a study that was conducted by Rayanakorn et al.[25] found that nurses were actively involved in HIV PrEP service delivery. Although nurses may have performed better in this regard, the delivery of HIV PrEP services fell short of optimum delivery. For example, only a quarter of participants had referred or prescribed HIV PrEP in the past 2 months, which was poor practice. This is similar to studies conducted by Moore et al.[23] and Terndrup et al.,[22] which showed that less than half of the study participants had prescribed HIV PrEP in the previous 12 months.
Our study revealed that almost a third of participants did not include HIV PrEP service in general service points. This is similar to studies that were conducted by Kenison et al.[30] and Muwonge et al.,[26] which revealed that poor practices of PrEP delivery are demonstrated by referring patients requiring HIV PrEP prescriptions to other health providers who are stationed at different service points. The results indicate the weakness in adhering to HIV PrEP guidelines that recommend the integration of HIV PrEP services into general health services and promote easy access to HIV prevention interventions.
Although a high proportion of participants reported good practices in the delivery of HIV PrEP services, we identified discrepancies between the extent of good practices reportedly performed and the level of knowledge or attitudes possessed by the participants. In particular, most participants reported conducting health education about PrEP and referring eligible clients for PrEP initiation, but a low proportion of healthcare workers had sufficient knowledge to perform the practices that they self-reported to deliver. This requires further investigation to interpret the high level of good practices reported in this study.
To our knowledge, this is the first study to assess the KAPs of oral HIV PrEP among healthcare workers in the Ekurhuleni District. Secondly, to assess KAPs towards oral HIV PrEP, we surveyed the prescribers of HIV PrEP and the non-prescribers, who are key role-players in identifying the high-risk population that may benefit from HIV PrEP.
Limitations
Our study findings may not be generalisable outside of Ekurhuleni District. Secondly, there may have been selection bias, as healthcare workers who volunteered to participate in the study might not have been interested in HIV prevention such as HIV PrEP. Self-report might have resulted in social desirability bias as healthcare workers were reporting professionally acceptable behaviors. In addition, the use of logistic regression rather than Poisson or negative binomial regression may have overestimated effect sizes since the prevalence of outcome was common.
Conclusion
Using a rapid cross-sectional survey design, we successfully identified healthcare worker KAPs that may act as barriers to optimum HIV PrEP uptake. Among the healthcare workers tasked with generating demand and identifying clients eligible for HIV PrEP services, low knowledge of HIV PrEP and negative attitudes to HIV PrEP may be barriers to the offer and enrolment of eligible clients on HIV PrEP. Our findings also showed that interpretation of self-reported practices in the delivery of HIV PrEP, without considering the level of HIV PrEP knowledge, may mask the low quality of service delivery in PHCs.
We recommend HIV PrEP training for HTS counsellors and health promoters who are the first contacts with potential HIV PrEP candidates in primary healthcare facilities. Onsite mentoring and coaching of healthcare workers such as HTS counselors and health promoters on HIV PrEP guidelines is needed to improve knowledge. Further investigations must be conducted to find the reasons for poor HIV PrEP knowledge among older healthcare workers, and the healthcare workers' concerns about HIV PrEP increasing risky sexual behaviour.
Declaration. This research article formed part of the requirements for fulfillment of an MSc in Epidemiology and Biostatistics for author EM. All procedures performed in this study were in accordance with the Faculty of Health Sciences Research Ethics Committee at the University of Pretoria (ref. no. 20/2022).
Acknowledgments. We would like to acknowledge the SA Field Epidemiology Training programme for funding the studies, and the Ekurhuleni Research Committee for providing the opportunity and permission to conduct the study. We would like to thank the healthcare workers who participated in this study.
Author contributions. Conceptualisation: EM, TM, ER. Data curation: EM. Formal analysis: EM, TM, AM. Methodology: EM, TM, ER. Project administration: EM. Supervision: TM, ER, LK. Writing of original draft: EM. Writing of review and editing: EM, AM,TM, ER.
Funding. None.
Conflicts of interest. None.
References
1. Joint United Nations Programme on HIV/AIDS. In danger: UNAIDS Global Aids Update 2022. Geneva: UNAIDS, 2022. https://www.unaids.org/en/resources/documents/2022/in-danger-global-aids-update (accessed 2 October 2022). [ Links ]
2. Joint United Nations Programme on HIV/AIDS. Global and regional data. Geneva: UNAIDS, 2021. https://www.unaids.org/en/resources/documents/2021/2021_unaids_di (accessed 3 October 2022). [ Links ]
3. National Department of Health, South Africa. Guidelines for the provision of pre-exposure prophylaxis (PrEP) to persons at substantial risk of HIV infection. Pretoria: NDoH, 2019. https://www.prepwatch.org/wp-content/uploads/2019/07/South-Africa-PrEP-Guidelines_Jan2019.pdf (accessed 10 October 2022). [ Links ]
4. National Department of Health, South Africa. South Africa's National Strategic Plan for HIV, TB and STIs 2017-2022. Pretoria: NDoH, 2017. https://www.gov.za/sites/default/files/gcis_document/201705/nsp-hiv-tb-stia.pdf (accessed 4 October 2022). [ Links ]
5. National Department of Health, South Africa. Updated guidelines for the provision of oral pre-exposure prophylaxis to persons at substantial risk of HIV infection. Pretoria: NDoH, 2021. https://www.prepwatch.org/wp-content/uploads/2020/07/South-Africa-PrEP-Guidelines_Jan2020.pdf (accessed 10 October 2022). [ Links ]
6. Joseph Davey DL, Daniels J, Beard C, et al. Healthcare provider knowledge and attitudes about pre-exposure prophylaxis (PrEP) in pregnancy in Cape Town, South Africa. AIDS Care 2020;32(10):1290-1294. https://doi.org/10.1080/09504121.1782328 [ Links ]
7. World Health Organization. Guidelines on long-acting injectable cabotegravir for HIV prevention. Geneva: WHO, 2022. [ Links ]
8. Aisha Khoele AB, Smith A, Grey A, et al. District Health Barometer In National Department of Health. Pretoria: Health Systems Trust, 2019/2020. https://www.hst.org.za/publications/Pages/DHB2019-20.aspx (accessed 11 October 2022). [ Links ]
9. Shamu S, Shamu P, Khupakonke S, et al. Pre-exposure prophylaxis (PrEP) awareness, attitudes and uptake willingness among young people: Gender differences and associated factors in two South African districts. Glob Health Action 2021;14:1886455. https://doi.org/10.1080/16549716.2021.1886455 [ Links ]
10. Wood BR, McMahan VM, Naismith K, Stockton JB, Delaney LA, Stekler JD. Knowledge, practices, and barriers to HIV preexposure prophylaxis prescribing among Washington State medical providers. Sex Transm Dis 2018;45(7):452-458. https://doi.org/10.1177/2150132719878526 [ Links ]
11. Manar Mohammed Alzahrani AAA, Alghamdi SA, Alotaibi RK. Knowledge and attitude of dentists towards obstructive sleep apnea. Int Dental J 2022;72(3):315-321. https://doi.org/10.1016/j.identj.2021.05.004 [ Links ]
12. Suresh A. What is the chi-square test and how does it work? An intuitive explanation with R Code. Analytics Vidhya, 2019. https://www.analyticsvidhya.com/blog/2021/06/decoding-the-chi-square-test%E2%80%8A-%E2%80%8Ause-along-with-implementation-and-visualisation (accessed 13 October 2022). [ Links ]
13. Alexopoulos EC. Introduction to multivariate regression analysis. Hippokratia 2010;14(1):23-28. [ Links ]
14. Amro FM, Rayan AH, Eshah NF, MS AL. Knowledge, attitude, and practices concerning Covid-19 preventive measures among healthcare providers in Jordan. SAGE Open Nurs 2022;8:23779608221106422. https://doi.org/10.1177/23779608221106422 [ Links ]
15. Panta G, Richardson AK, Shaw IC, Coope PA. Healthcare workers' knowledge and attitudes towards sterilisation and reuse of medical devices in primary and secondary care public hospitals in Nepal: A multi-center cross-sectional survey. PLoS One 2022;17(8):e0272248. https://doi.org/10.1371/journal.pone.0272248 [ Links ]
16. Mutaru AM, Balegha AN, Kunsu R, Gbeti C. Knowledge and determinants of infection prevention and control compliance among nurses in Yendi municipality, Ghana. PLoS One 2022;17(7):e0270508. https://doi.org/10.1371/journal.pone.0270508 [ Links ]
17. Nordin NN, Vaithilingam RD, Saub R, et al. Awareness, knowledge, attitudes and practices on the management of diabetes mellitus patients with periodontitis amongst Malaysian primary care practitioners. Malays Fam Physician 2021;16(3):44-55. https://doi.org/10.51866/oa1131 [ Links ]
18. Alvarado A, Mader EM, Buttke D, Harrington LC. Southwestern national park service employee risk, knowledge, and concern for triatomine exposure: A qualitative analysis using a novel knowledge, attitudes, and practices survey. PLoS Negl Trop Dis 2022;16(9):e0010744. https://doi.org/10.1371/journal.pntd.0010744 [ Links ]
19. Tantipoj C, Sirichanyaphong T, Nuntachurat J, et al. Dentists' attitudes toward diabetes mellitus screening in Thai dental clinics. Int J Environ Res Public Health 2022;19(6):e0010744. https://doi.org/10.1371/journal.pntd.0010744 [ Links ]
20. Odusanya OO, Adeniran A, Bakare OQ, et al Building capacity of primary health care workers and clients on COVID-19: Results from a web-based training. PLoS One 2022;17(10):e0274750. https://doi.org/10.1371/journal.pone.0274750 [ Links ]
21. Abore KW, Debiso AT, Birhanu BE, Bua BZ, Negeri KG. Health professionals' readiness to implement electronic medical recording system and associated factors in public general hospitals of Sidama region, Ethiopia. PLoS One 2022;17(10):e0276371. https://doi.org/10.1371/journal.pone.0276371 [ Links ]
22. Terndrup C, Streed CG Jr., Tiberio P, et al. A cross-sectional survey of internal medicine resident knowledge, attitudes, behaviors, and experiences regarding pre-exposure prophylaxis for HIV infection. J Gen Intern Med 2019;34(7):1258-1278. https://doi.org/10.1007/s11606-019-04947-2 [ Links ]
23. Moore E, Kelly SG, Alexander L, et al. Tennessee healthcare provider practices, attitudes, and knowledge around HIV pre-exposure prophylaxis. J Prim Care Comm Health 2020;11:2150132720984416. https://doi.org/10.1177/2150132720984416 [ Links ]
24. Sammons MK, Gaskins M, Kutscha F, Nast A, Werner RN. HIV pre-exposure prophylaxis (PrEP): Knowledge, attitudes and counseling practices among physicians in Germany - a cross-sectional survey. PLoS One 2021;16(4):e0250895. https://doi.org/10.1371/journal.pone.0250895 [ Links ]
25. Rayanakorn A, Chautrakarn S, Intawong K, et al. A comparison of attitudes and knowledge of pre-exposure prophylaxis (PrEP) between hospital and key population led health service providers: Lessons for Thailand's universal health coverage implementation. PLoS One 2022;17(5):e0268407. https://doi.org/10.1371/journal.pone.0268407 [ Links ]
26. Muwonge TR, Nsubuga R, Brown C, et al. Knowledge and barriers of PrEP delivery among diverse groups of potential PrEP users in Central Uganda. PLoS One 2020; 15(10):e0241399. https://doi.org/10.1371/journal.pone.0241399 [ Links ]
27. Kambutse I, Igiraneza G, Ogbuagu O. Perceptions of HIV transmission and pre-exposure prophylaxis among health care workers and community members in Rwanda. PLoS One 2018;13(11):e0207650. https://doi.org/10.1371/journal.pone.0207650 [ Links ]
28. Pilgrim N, Jani N, Mathur S, et al. Provider perspectives on PrEP for adolescent girls and young women in Tanzania: The role ofprovider biases and quality of care. PLoS One 2018;13(4):e0196280. https://doi.org/10.1371/journal.pone.0196280 [ Links ]
29. Asabor EN, Lett E, Moll A, Shenoi SV "We've got our own beliefs, attitudes, myths': A mixed methods assessment of rural South African health care workers' knowledge of and attitudes towards PrEP implementation. AIDS Behav 2021;25(8):2517-2532. https://doi.org/10.1007/s10461-021-03213-z [ Links ]
30. Kenison TC, Badenhop B, Safo S. Unlocking HIV pre-exposure prophylaxis delivery: Examining the role of HIV providers in pre-exposure prophylaxis care. AIDS Patient Care STDS 2020;34(6):251-258. https://doi.org/10.1089/apc.2019.0288 [ Links ]
31. Mutabazi JC, Gray C, Muhwava L, et al. Integrating the prevention of mother-to-child transmission of HIV into primary healthcare services after AIDS denialism in South Africa: Perspectives of experts and health care workers - a qualitative study. BMC Health Serv Res 2020;20(1):582. https://doi.org/10.1186/s12913-020-05381-5 [ Links ]
32. Iwu CJ, Ngcobo N, Cooper S, et al. Mobile reporting ofvaccine stock-levels in primary health care facilities in the Eastern Cape Province of South Africa: Perceptions and experiences of health care workers. Hum Vaccin Immunother 2020;16(8):1911-1917. https://doi.org/10.1080/21645515.2019.1700713 [ Links ]
33. Pillay D, Stankevitz K, Lanham M, et al Factors influencing uptake, continuation, and discontinuation of oral PrEP among clients at sex worker and MSM facilities in South Africa. PLoS One 2020;15(4):e0228620. https://doi.org/10.1371/journal.pone.0228620 [ Links ]
34. Felsher M, Szep Z, Krakower D, Martinez-Donate A, Tran N, Roth AM. 'I don't need PrEP right now': A qualitative exploration of the barriers to PrEP care engagement through the application of the health belief model. AIDS Educ Prev 2018;30(5):369-381. https://doi.org/10.1521/aeap.2018.30.5.369 [ Links ]
35. Vega-Ramirez H, Torres TS, Guillen-Diaz C, et al. Awareness, knowledge, and attitudes related to HIV pre-exposure prophylaxis and other prevention strategies among physicians from Brazil and Mexico: A cross-sectional web-based survey. BMC Health Serv Res 2022;22(1):532. https://doi.org/10.1186/s12913-022-07900-y [ Links ]
36. Kundu I, Martinez-Donate A, Karkada N, et al. Attitudes and referral practices for pre-exposure prophylaxis (PrEP) among HIV rapid testers and case managers in Philadelphia: A mixed methods study. PLoS One 2019;14(10):e0223486. https://doi.org/10.1371/journal.pone.0223486 [ Links ]
 Correspondence:
Correspondence:
E Mahlare
gugulakhemnisi@gmail.com
Accepted 19 October 2023














