Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 no.8 Pretoria Ago. 2023
http://dx.doi.org/10.7196/samj.2023.v113i8.717
RESEARCH
Acute angioedema in Cape Town emergency centres and a suggested algorithm to simplify and improve management
C DayI, II; J van der WaltIII, IV; K CrombieV; C HendrikseVI; J PeterVII, VIII
IFCP (SA), MMed (Med); Division of Allergology and Clinical Immunology, Department of Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
IIFCP (SA), MMed (Med); Allergy and Immunology Unit, University of Cape Town Lung Institute, Cape Town, South Africa
IIIAllergy (Cert), MFamMED; Division of Allergology and Clinical Immunology, Department of Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
IVAllergy (Cert), MFamMED; Allergy and Immunology Unit, University of Cape Town Lung Institute, Cape Town, South Africa
VFCP (SA), MMed (Med): Division of Emergency Medicine, Department of Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
VIFCEM (SA), MMed (EM); Division of Emergency Medicine, Department of Family, Community and Emergency Care, Faculty of Health Sciences, University of Cape Town South Africa
VIIFCP (SA), PhD; Division of Allergology and Clinical Immunology, Department of Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
VIIIFCP (SA), PhD; Allergy and Immunology Unit, University of Cape Town Lung Institute, Cape Town, South Africa
ABSTRACT
BACKGROUND: Angioedema is the most common acute allergic presentation to emergency centres (EC), with hospitalisation rates increasing in high-income countries. Angioedema can complicate with life-threatening laryngeal obstruction. There are no local data; therefore, we aimed to characterise acute angioedema cases presenting to ECs and develop a simple management algorithm
OBJECTIVE: To characterise the clinical presentation, management and outcomes of acute angioedema cases presenting to ECs. Based on these findings, we developed a management algorithm for acute angioedema to improve the care of acute angioedema in South Africa (SA
METHODS: We conducted a retrospective folder review of all patients admitted to Groote Schuur Hospital (tertiary) and Mitchells Plain District Hospital (secondary) ECs from 1 June 2018 to 31 June 2020. Using ICD-10 coding, folders of adults >18 years with possible angioedema presenting to the ECs were screened. An allergist extracted demographics, medical history, management and outcome data for each angioedema event
RESULTS: A total of 142 acute angioedema episodes were included, with a median (interquartile range) age of 42 (28 - 58) years, and 62% of patients were female. The majority (124/142, 87%) of acute angioedema EC presentations involved swelling above the shoulders, with airway involvement in 20 (14%) patients, with two patients requiring intubation. Nineteen (13%) patients required admission, with five (26%) admitted to high care/intensive care. Drug-induced angioedema was the most common cause, with 64/142 (45%) linked to a known offending drug, 42/64 (65.6%) being angiotensin-converting enzyme inhibitor (ACE-I). Critical information to guide angioedema management, including past personal/family allergy history, and duration of angioedema prior to EC visit, was not recorded in 64.7% and 37.8% of EC records, respectively. Unnecessary treatment with corticosteroids or antihistamines occurred in 19/53 (36%) and 16/53 (30%) cases with bradykinin-mediated angioedema ACE-I angioedema and hereditary angioedema). Overall, only 36/142 (25%) of angioedema patients were connected to allergy care
CONCLUSION: Angioedema is the most common allergy presentation to two ECs in Cape Town, SA. Bradykinin-mediated angioedema secondary to ACE-I therapy is the single most common offender, and was not appropriately managed in more than a third of cases. Based on these findings, we have developed a management algorithm that easily stratifies patients into bradykinin or mast cell-mediated angioedema with a step-by-step management approach that is applicable to the SA context. Ongoing awareness and education on allergy emergencies are required to ensure accurate diagnosis of less common causes of angioedema (particularly bradykinin-mediated angioedema) and linkage to allergy specialist care
Angioedema is paroxysmal, localised and self-limiting swelling of the subcutaneous and/or submucosal tissue due to a temporary increase in vascular permeabilty[1] The number of acute angioedema cases in high-income countries (HICs) is increasing.[2] However, there is a paucity of data regarding the epidemiology of angioedema in Africa. This is concerning, given that persons of African ancestry are three to five times more likely to have angiotensin converting enzyme inhibitor (ACE-I) angioedema.[3]
The aetiology of angioedema is complex, but in the emergency setting attempting to distinguish bradykinin (BK)-mediated from mast cell (MC)-mediated angioedema is important, as acute management differs. MC-mediated angioedema is responsive to treatment with corticosteroids and antihistamines, while BK-mediated angioedema is not responsive to these drugs, but does improve after administration of fresh frozen plasma, bradykinin receptor antagonists and kallikrein inhibitors.[1] Delays in recognising and treating BK-mediated angioedema can result in life-threatening laryngeal oedema and potentially death, which is particularly tragic among patients with known BK-mediated angioedema diagnoses, such as type 1 hereditary angioedema (HAE). If untreated, laryngeal angioedema has a mortality rate of 25%, and up to 40% in HAE.[4] Several easily acquired clinical features can help guide emergency treatment, including a known diagnosis or family history of HAE, the prescription of an offending drug, e.g. ACE-I, angioedema without urticaria (or other features of anaphylaxis), or exposure to a known allergen in atopic individuals (Fig. 1).[2,5,6]
Africa faces a growing epidemic of hypertension, with the prevalence of hypertension in South Africa (SA) estimated to be 18.9%.[7] ACE-I are affordable drugs used globally for the treatment of cardiovascular and renal disease and are a mainstay of hypertension treatment in low- and middle-income countries (LMICs). Although there are other drugs (e.g. non-steroidal anti-inflammatory drugs (NSAIDs)) that cause angioedema, ACE-I are the most common. ACE-I angioedema is also the most common BK-mediated angioedema, occurring in up to 1% of patients prescribed an ACE-I, and accounts for -30% of acute BK-mediated angioedema in HICs.[2] Risk factors for severe ACE-I angioedema include older age, obesity, hypertension, diabetes, dyslipidaemia and smoking.[2,5,6] We decided to evaluate the burden of ACE-I angioedema, and the characteristics and management of acute angioedema presenting to SA Emergency Centres (ECs), given this increasing ACE-I use and paucity of data from LMICs and Africa in particular.
Methods
This study is a retrospective folder review of all EC admissions >18 years between June 2018 and June 2020 at Groote Schuur Hospital EC (GSH) and Mitchells Plain District Hospital EC (MPDH) (Fig. 1), and was approved by the University of Cape Town Human Research Ethics Committee as part of the Angioedema Biomarkers in Africa (ABA) study (ref. no. 057/2020). The Western Cape Government official electronic patient tracking and registration database, Hospital and Emergency Centre Tracking Information System (HECTIS), was used to identify patients that were coded T78.3 (angioneurotic oedema) and T78.4 (allergy unspecified) by the International Classification of Diseases 10 (ICD-10). Two allergists reviewed HECTIS data and patient folders. Two ECs were selected: these sites utilise HECTIS, have a high admission rate, and are respectively a secondary and tertiary care centre. MPDH is a 230-bed district level facility located 32 km from the Cape Town city centre. It serves a population of approximately 600 000, and is referral facility for all local primary care facilities. MPDH EC is one of the busiest in SA, and monthly there are 4 500 EC presentations. GSH is a 900-bed tertiary referral centre that serves the Cape Town Metro health district (population ~4 801 000)[8] and the West Coast district (population -400 000).[9] The GSH medical EC has up to 3 000 admissions per month, with a separate trauma unit that has up to 1 000 admissions per month. These centres serve a large community in which the predominant racial group is the SA coloured population (SAC), followed by black, white and other racial groups. Angioedema is more common in patients with African ancestry, hence self-reported race was assessed.
Data were extracted for each acute angioedema episode, including patient demographics, clinical presentation, documented medical and allergy history, admission details, pharmacological and non-pharmacological treatment and discharge details. Angioedema was defined as paroxysmal, localised and self-limiting swelling of the subcutaneous and/or submucosal tissue, due to a temporary increase in vascular permeability. Anaphylaxis was defined based on the recent World Allergy Organisation Guidelines[10] as the presence of urticaria or angioedema, with either cardiac, respiratory, or gastrointestinal disturbances. Intubation included any attempts at intubation, whether direct, endoscopic, or surgical.
Results
A total of 224 events were coded T78.3/T78.4 on HECTIS by ICD-10 in patients >18 years. Of these 265 events, 142 (61.5%) presented with angioedema (Fig. 1, Table 1). Using the information available, patients could be split into BK-mediated (37%, 53/142) or MC-mediated angioedema (50%, 71/142); 12.7% (18/142) patients had insufficient information or features to classify. The median (interquartile range (IQR)) age was 42 (28 - 58) years overall, with a significantly higher median age among BK-mediated angioedema (57 (43 - 67) years v. 35 (25 - 48) years, p<0.001). Overall, there was a female predominance of 62.4% (88/142), and the median age of the cohort was 42 (IQR 28 - 58) years, with a similar distribution across both facilities (Table 1). The most common self-reported racial group was SAC at 57.4% (81/142), followed by black at 35.9% (51/142), with no differences between BK and MC angioedema groups. Isolated angioedema (without urticaria or anaphylaxis) was the most common presentation at 73.9% (107/142). Overall, nine patients presented with angioedema in the context of anaphylaxis (6.3%, 9/142).
A possible allergen was identified in 71.8% of events (Table 1). Drug-induced angioedema was most common at 45% (64/142), with ACE-I being the single most common drug implicated (65.6%, 42/64), followed by NSAIDs (17.2%, 11/64) and antibiotics (9.4%, 6/64). Other triggers included foods in 18.3% (26/142), as well as bee venom (6/142 (4.2%)), and paraphenylenediamine in hair dye 4/142 (2.8%). Information regarding the time from the start of angioedema to hospital presentation was only available for 90 (63.4%) patients, with a median (IQR) time of 12 (5 - 24) hours.
Overall, 50/142 (35.2%) patients had two or more swollen body areas, with 124/142 (87.3%) presenting with swelling above the shoulders. The most common sites of angioedema were the face, at 36.6% (n=52), the tongue, at 33.8% (n=48), and the lips, at 32.4% (n=46). Four of the HAE patients presented with isolated bowel angioedema. A total of 20 (14%) patients had airway angioedema, with 2 requiring intubation. There were no deaths. Acute infective illness was the most common contributing factor (22/142, 15.5%), with 6 patients (4.2%) having a newly diagnosed chronic illness.
Allergy history was poorly documented, with information available for only 35.2% of the cohort. In the overall cohort, 33/50 patients (66%) had atopy, with a higher number of atopic patients in the MC-mediated than the BK-mediated groups, although the difference was non-significant (40% (20/50) v. 30% (9/30), respectively) (p=1.8).
The most common diagnoses were a history of previous allergies 15/50 (30%) angioedema 11/50 (22%) and HAE 11/50 (22%). More information was available for general medical history with data for 114 (80.2%) patients. The most common comorbidity was hypertension (n=55, 48.2%) followed by elevated cholesterol (n=18, 15.8%), with 11 patients having HIV (9.6%). There was a higher number of medical comorbidities in the BK-mediated angioedema group compared with the MC-mediated group.
The most used medications were oral antihistamines (59.2%, 84/142), corticosteroids (50%, 71/142; oral corticosteroids 25.3% (36/142); intravenous corticosteroids 24.6% (35/142)) (Table 2). Adrenaline was administered to 19% of patients, but only one patient received adrenaline on discharge. A total of 19 (13.4%) patients were admitted, with 5 (26.3%) admitted to a high care unit or intensive care unit (ICU), 11 (57.9%) admitted to the EC short-stay ward and 3 (15.8%) admitted to general medical wards. Only 25.4% of patients were referred to the Allergy Clinic, with only 3/11 of the patients with recurrent angioedema referred. Importantly, no patients with suspected anaphylaxis had a mast-cell tryptase measurement performed.
Description of ACE-I angioedema patients
Overall, 42 patients had ACE-I angioedema. In keeping with the overall cohort, the majority of these were female (n=27, 64.3%). However, this group was older than the overall cohort, with a median (IQR) age of 61 (50 - 68) years. The most commonly self-reported race was SAC (n=22, 53.7%), but there was a larger proportion of black African patients in this group compared with the overall cohort (18/42, 41.5% and n=51, 31.9%, respectively). This group had the most comorbidities, including hypertension (87.8%, 37/42), hypercholesterolaemia (29.3%, 12/42) and diabetes (26.2%, 11/42). One patient was known to the allergy clinic, and only two patients had a history of allergic disease (asthma, 4.8%), but six patients (14.6%) had previously had angioedema while on an ACE-I and the drug was not discontinued. Information regarding contributing factors for acute angioedema was available for 23/42 patients (56.1%), with four patients having an acute illness (congestive cardiac failure, acute COVID-19 infection, bacterial pharyngitis and gastroenteritis), and another four having a newly diagnosed chronic illness (hypertension, HIV, HIV-associated nephropathy and lung cancer), with one patient using additional over-the-counter medication, namely aspirin). The time since starting an ACE-I was poorly documented and information was only available for 12 patients. The median time in days from initiation of an ACE-I to onset of angioedema was 14 days, with a wide IQR of 5 - 758. The time from symptom onset to presentation at a healthcare facility was prolonged at 12 (IQR 5 - 25) hours, which is similar to the overall cohort. Overall, 17/42 (41.46%) of these patients had more than one area of angioedema, with 38/42 (92.7%) having above-the-shoulder swelling, and 9/42 (22%) having airway angioedema (one patient required intubation, and there were no deaths). Seven patients (16.7%) required adrenaline for airway-threatening angioedema. Six patients (14.6%) received fresh frozen plasma, and no patients received bradykinin receptor antagonists. Inappropriately, 17 (40.5%) patients received corticosteroids, with 15 (36.5%) also inappropriately receiving oral antihistamines. Information regarding change in antihypertensive treatment was available for 33 (80.5%) patients: 20/33 (60.6%) were switched from ACE-I to alternative treatment (calcium channel blocker n=12, angiotensin receptor blocker n=10, thiazide n=2, spironolactone «=1, >1 agent ?i=3). Of concern, two patients were continued on an ACE-I despite documented ACE-I angioedema. A total of six (14.6%) patients were admitted: ICU n=1 (2.4%), EC short-stay ward n=2 (4.9%), general ward n=3 (7.3%). The median duration of admission was 2 days (IQR 1 - 5.75). Only eight (19.5%) patients were referred to the allergy clinic, with 31/42(75.6%) patients having no follow-up plan.
Description of HAE patients
There were 11 patients in the cohort with HAE, and all presented to GSH. The majority were female (90.9%,10/11) and all were SAC. Eight attacks were spontaneous, with three patients having triggers (minor trauma, missed androgen treatment, and consumption of monosodium glutamate in patient with known allergy). Four patients (36.4%) had isolated bowel angioedema, and six (54.5%) had swelling above the shoulder. None of the patients had airway compromise and none required intubation. The time in hours from onset of angioedema to presentation was longer in the HAE group than in the other groups, with a median (IQR) of 24 (15 - 48) hours. Overall, seven patients (63.6%) were on danogen prophylaxis. Three patients (27.2%) were treated erroneously - two received corticosteroids, and another oral antihistamine. Only three patients received recombinant CI inhibitor concentrate, and none received a bradykinin 2 receptor antagonist despite availability at GSH. The majority were treated with fresh frozen plasma (63.6%, 7/11) and freeze-dried plasma (9%, 1/11).
Discussion
Angioedema is the most common allergy presentation to ECs in Cape Town, SA, with BK-mediated angioedema secondary to ACE-I therapy being the single most common offender. Critically past medical history and basic clinical features to allow differential treatment of BK- and MC-mediated forms of angioedema were not documented, with resultant unnecessary or incorrect treatments. Ongoing awareness and education on allergy emergencies are required to ensure accurate diagnosis of less common causes of angioedema (particularly BK-mediated angioedema) and linkage to allergy specialist care.
In North America, the burden oí acute angioedema has been increasing, and between 12% and 30% of cases are due to ACE-I.[2] Globally, the overall mortality rate due to acute angioedema is low, but hospitalisations and complications due to angioedema have been increasing,[1,2] In comparison, our ACE-I angioedema rate is 28.9%. Both SA and North American ACE-I angioedema cohorts were older, mostly female, had a high percentage of Africans, and had more comorbid illnesses.[2,12] In the present study, most admissions were to the EC short-stay ward and the EC-run high care unit, indicating that acute angioedema places a large burden on ECs and staff. Allergy history, presentation and identification of potential triggers were poorly documented in EC clerking notes, with a large amount of missing data (particularly regarding allergic comorbidities, co-factors and timing of events). In addition, there was incorrect management of BK-mediated angioedema with corticosteroids and antihistamines in 39.6% of this group (n=21/53). This highlights the need for improving allergy teaching at the undergraduate and postgraduate level, as well as improving guidelines for the acute management of angioedema in SA.
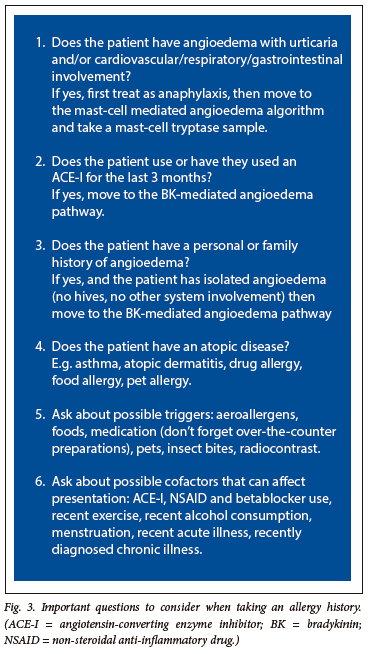
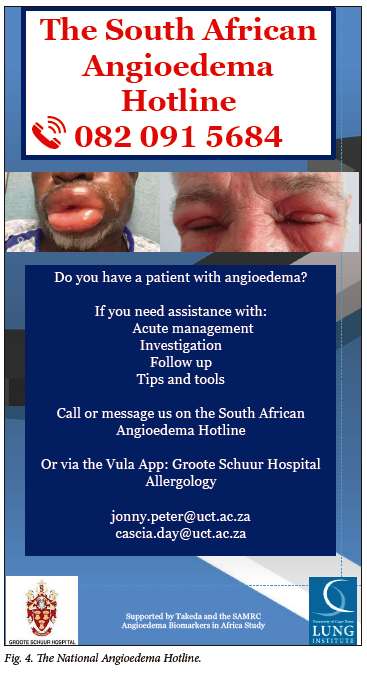
Globally, one in five individuals has an allergic disease, and this number will rise, as the incidence of allergies and autoimmune disease is increasing.[13] Allergology is a relatively new subspecialist field and a scarce resource, with few trained allergologists in SA. The World Allergy Organisation and the European Academy of Allergy and Clinical Immunology have found that training gaps exist globally at both undergraduate and postgraduate levels. These include: angioedema, insect/food allergies, diagnostic testing and indications for specialist referral.[13] Lombardi et al.[14] found that physicians have very poor awareness of the side-effects of ACE-I, with only 31.9 - 40% of clinicians correctly answering survey questions. These training gaps can be seen in this cohort in the sparsely completed allergy history, and incorrect treatment of BK-mediated angioedema. SA ECs are staffed by a variety of specialists from internal medicine, family medicine and emergency medicine, as well as trainee registrars, medical officers and interns. The variety of clinical experience, and the distribution across different specialties makes targeting teaching gaps challenging. Hence we have created an algorithm for the management of acute angioedema in the SA setting (Fig. 2) that can be utilised at any clinical skill level. This algorithm distinguishes BK- from MC-mediated angioedema, and highlights the differences in management and the treatment options available in our setting. We have also highlighted important questions to ask in an allergy assessment (Fig. 3). In addition, we have started the National Angioedema Hotline to provide advice and assistance to clinicians managing these cases, particularly for junior clinicians in rural areas (Fig. 4). It is critical that SA universities update their undergraduate and postgraduate programmes to teach the management of allergic conditions, management of allergic emergencies, and when to refer for specialist opinion.
This is the first study to review the epidemiology and outcomes of acute angioedema in SA. However, the study was limited to two ECs in the Cape Town Metro and may not be a clear representation of acute angioedema in SA. A larger, multicentre, national review is needed to gain a deeper understanding of the epidemiology of angioedema in our context. Globally, there is little information on angioedema in LMICs, and future studies are advised. We relied on the correct ICD-10 coding of events by clinicians and administration staff to identify acute events, which is open to error. We also relied on the completeness of clerking notes by clinicians for each event and, as has already been highlighted there were missing data regarding allergy history and presentation.
Angioedema is the most common allergy presentation to ECs in Cape Town, with one to three cases per facility per week. BK-mediated angioedema secondary to ACE-I therapy is the single most common cause. Ongoing awareness and education on allergy emergencies are required to ensure accurate diagnosis and management of angioedema (particularly BK-mediated angioedema). Re-evaluation of allergy teaching is needed, as well as improved linkage to allergy specialist services.
Declaration. This manuscript is part of CD's PhD thesis. Acknowledgements. Thank you to the Angioedema Biomarkers in Africa team and the SA Medical Research Council.
Author contributions. JR CD, and JvdW designed the study. CD and fvdW conducted the folder review, and analysis. CD and JP wrote the first draft, all authors edited and reviewed the manuscript.
Funding. None.
Conflicts of interest. None.
References
1. Cicardi M, Suffritti C, Perego F, Caccia S. Novelties in the diagnosis and treatment of angioedema J Investig Allergol Clin Immunol 2016;26(4):212-221. https://doi.org/10.18176/jiaci.0087 [ Links ]
2. Smith A, Ray M, Jain N, Zhang H, Sebelik M. The burden of angioedema on United States emergency departments'. 2006-2010. Laryngoscope 2017;127(4):828-834. https://doi.org/10.1002/lary.26336 [ Links ]
3. Brown NJ, Ray WA, Snowden M, Griffin MR. Black Americans have an increased rate of angiotensin converting enzyme inhibitor-associated angioedema. Clin Pharmacol Ther 1996;60(1):8-13. https://doi.org/10.1016/s0009-9236(96)90161-7 [ Links ]
4. Javaud N, Karami A, Stirnemann J, et al. Bradykinin-mediated angioedema. Factors prompting ED visits. Am J Emerg Med 2013;31(1):124-129. https://doi.org/10.1016/j.ajem.2012.06.021 [ Links ]
5. Stauber T, Confino-Cohen R, Goldberg A. Life-threatening angioedema induced by angiotensin-converting enzyme inhibitors. Characteristics and risk factors. Am J Rhinol Allergy 2014;28(1):54-58. https://doi.org/10.2500/ajra.2014.28.3989 [ Links ]
6. Sandefur BJ, Silva LOJE, Lohse CM, et al. Clinical features and outcomes associated with angioedema in the emergency department. W J Emerg Med 2019;20(5):760-769. https://doi.org/10.5811/westjem.2019.6.42852 [ Links ]
7. Kamerman P. Underdiagnosis of hypertension and diabetes mellitus in South Africa. S Afr Med J 2022;112(1):53-50. https://doi.org/10.7196/SAMJ.2022.v112i1.15968 [ Links ]
8. Macrotrends. Cape Town, South Africa Metro Area Population 1950-2022. Macrotrends, 2022. https://www.macrotrends.net/cities/22481/cape-town/population (accessed 30 September 2022). [ Links ]
9. Department of Cooperative Government and Traditional Affairs, South Africa. West Coast District Municipality Western Cape, profile and analysis district development model. Pretoria. COGTA, 2020. https://www.cogta.gov.za/ddm/wp-content/uploads/2020/ll/Westcoast-DM-September-2020.pdf (accessed 30 September 2022). [ Links ]
10. Cardona V, Ansotegui IJ, Ebisawa M, et al. World Allergy Organization anaphylaxis guidance 2020. World Allergy Org J 2020;13(10):100472. https://doi.org/10.1016/j.waojou.2020.100472 [ Links ]
11. Kim SJ, Brooks JC, Sheikh J, Kaplan MS, Goldberg BJ. Angioedema deaths in the United States, 1979-2010. Ann Allergy Asthma Immunol 2014;113(6):630-634. https://doi.Org/10.1016/j.anai.2014.09.003 [ Links ]
12. Depetri F, Tedeschi A, Cugno M. Angioedema and emergency medicine. From pathophysiology to diagnosis and treatment. Eur J Int Med 2019;59:8-13. https://doi.org/10.1016/j.ejim.2018.09.004 [ Links ]
13. Barker S, Daniels L, Chang Y-S, et al. Allergy education and training for physicians. World Allergy Org J 2021;14(10):100589. https://doi.org/10.1016%2Fj.waojou.2021.100589 [ Links ]
14. Lombardi C, Crivellaro M, Dama A, Senna G, Gargioni S, Passalacqua G. Are physicians aware of the side effects of angiotensin-converting enzyme inhibitors?. A questionnaire survey in different medical categories. Chest 2005;128(2):976-979. https://doi.org/10.1378/chest.128.2.976 [ Links ]
 Correspondence:
Correspondence:
C Day
cascia.day@uct.ac.za
Accepted 12 June 2023














