Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 n.8 Pretoria Aug. 2023
http://dx.doi.org/10.7196/samj.2023.v113i8.649
IN PRACTICE
CASE REPORT
Cavernous sinus thrombosis: A rare and potentially lethal complication of herpes zoster ophthalmicus that can easily be missed
N Narainswami
FC Ophth (SA); Grey's Hospital Eye Clinic, Pietermaritzburg, South Africa
ABSTRACT
Cavernous sinus thrombosis is a rare life-threatening complication of herpes zoster ophthalmicus (HZO). This case highlights the importance of at least considering the diagnosis in all cases of HZO, as the consequences of missing it can be disastrous.
Herpes zoster ophthalmicus (HZO) is a well-recognised opportunistic infection representing reactivation of latent varicella-zoster along the ophthalmic division (V1) of the trigeminal nerve.[1] More commonly known as shingles, it can affect both immunocompetent and immunocompromised individuals, although the disease runs a more severe course in those who are immunocompromised[1,2]It is frequently a blinding condition in South Africa (SA) owing to late presentation, often coupled with a delay in initiation of appropriate treatment. The disfiguring facial scarring and chronic pain of post-herpetic neuralgia (PHN) that affect many patients add to the burden of psychosocial morbidity associated with this devastating disease.
Approximately 20% of patients with herpes zoster may present with HZO, and of these ~50% will have ocular involvement.[3-5] The presence of Hutchinson's sign (lesions on the lateral aspect and/or the tip of the nose) indicates nasociliary nerve involvement and has a strong positive predictive value for ocular involvement.[6] Causes of acute vision loss include necrotising retinitis, kerato-uveitis, scleritis, and rarely optic neuritis. Neuro-ophthalmic manifestations such as encephalitis, aseptic meningitis and cranial nerve palsies, although uncommon, have been described. Cavernous sinus thrombosis is a very rare but potentially lethal complication of HZO, with just a few isolated case reports in the literature.[7] However, it is critical that the diagnosis is considered and not missed when dealing with a patient with HZO.
Case report
A 49-year-old HIV-positive woman, who had been on highly active antiretroviral therapy (HAART) for over a year, presented with a 4-week history of progressive painful visual loss affecting the right eye. She had attended her local clinic twice during the preceding month with no improvement in symptoms. Of note, she complained of recent-onset double vision, worse on left gaze, and a worsening headache over the past few days.
Clinical examination revealed a vesicular rash along the V1 distribution, with cicatrising lesions in various stages of healing along the lateral aspect of the right nostril. Her right lid was ptotic, with an injected eye deviated outwards on primary gaze (Fig. 1). She had hypoaesthesia of the right cornea and along the V1 dermatomal distribution. Anterior segment examination was remarkable for an active mild uveitis of the right eye. Ocular motility testing revealed an incomitant squint on versions and markedly severe limited adduction and elevation of the right globe by at least 80% on ductions. Abduction of the right eye was comparatively less reduced by ~40%. Both pupils were equal and reactive to light, and both optic discs were pink with no disc swelling seen on direct fundoscopy. Flourescein dye staining highlighted a dendritic lesion of the inferior left cornea, with tapered ends and absence of terminal bulbs. Otherwise, left ocular examination was unremarkable. The rest of the neurological assessment was grossly normal, and the patient was haemodynamically stable and afebrile. Her baseline blood panel was normal.

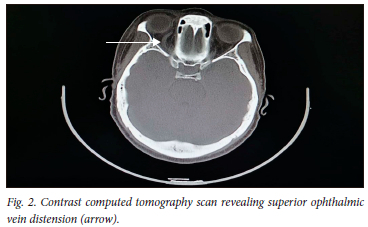
At this point our working diagnosis was HZO with ocular involvement complicated by probable intracranial extension. The pattern of combined oculomotor (CN 3), trigeminal (CN 5) and abducens (CN 6) cranial nerve palsies localised the lesion to the right cavernous sinus. There was no proptosis or chemosis. The neurology department was consulted, and an emergency contrast computed tomography scan was ordered. The scan (Fig. 2) revealed an obvious dilation of the superior ophthalmic vein of the right orbit and a filling defect of the right cavernous and transverse sinus in keeping with thrombosis.
The patient was commenced on intravenous acyclovir, broad-spectrum intravenous antibiotics, low-molecular-weight heparin and warfarin anticoagulation, and co-managed with neurology as an inpatient. She responded well to treatment during her hospital stay. A follow-up magnetic resonance venogram (MRV) revealed patency of all intracranial venous sinuses. Subsequent follow-ups at 3 and 6 months showed progressive improvement in the patient's ptosis and resolution of her ophthalmoplegia, and she no longer complained of horizontal diplopia.
Discussion
Herpes zoster occurs commonly in SA, and most clinicians will encounter a patient with HZO at some point in their career. Most patients making up this demographic in SA are young immunocompromised adults. The rest are elderly and immunocompetent, with a less severe and somewhat self-limiting disease course. HZO more commonly affects HIV-positive patients with relatively modest decreases in CD4 counts as opposed to patients with profound immunosuppression. It is therefore thought to be a disease of immune dysregulation rather than severe immunosuppression. While studies show that PHN and ocular inflammatory disease are the most common complications, there have been a few isolated case reports of cavernous sinus thrombosis as a potentially fatal complication.[7] Both CT venograms and MRVs were used in these cases to diagnose cavernous sinus venous thrombosis early in management. While an MRV was not readily available after hours for our patient, an emergency contrast CT scan of the brain and orbits by an experienced senior radiologist confirmed the diagnosis. However, MRV was performed during her hospital stay while she was on antithrombotic therapy to assess whether thrombi detected on the contrast CT scan at diagnosis had resolved. At follow-up after 1 month her vision had improved in both eyes, and her right ptosis improved further. She was discharged within a month and given a follow-up appointment at the combined neuro-ophthalmic clinic on discharge.
The important points to highlight in this case are the clues in the history and subsequent clinical examination that suggested a rare life-threatening complication presenting in a relatively common clinical scenario. Diplopia is usually uncommon in the setting of acute HZO, because inflammatory oedema of the affected eyelid often results in a severe mechanical ptosis that nullifies the visual input for binocular diplopia. Our patient presented a few weeks after onset of the rash, when some of that eyelid oedema had possibly begun to subside, allowing her eye to partially open. It was at this point that she became aware of the double vision. The recent worsening headache was also not in keeping with the natural pattern of PHN, which typically announces itself early in the disease process. The vital clue in the clinical examination was eliciting an ophthalmoplegia, which is not in keeping with a straightforward uncomplicated case of HZO. Lifting a ptotic lid and grossly examining extraocular movements (easily done in less than a minute) can elicit reduced ocular movements. The cranial nerve palsies identified in this way would alert the clinician to the possibility of a life-threatening complication such as intracranial venous sinus thrombosis. The consequences of missing such an important clinical sign and delaying urgent neuro-imaging and definitive treatment under multidisciplinary care could potentially be disastrous.
Despite the advent of HAART, HZO remains relatively common in HIV-infected patients. Zostervax and Shingrix are two current herpes zoster vaccines available in SA. While Zostervax is readily available for elderly patients (>70 years old), because it is a live attenuated vaccine concerns have been raised regarding its use in a younger immunocompromised group. Shingrix, on the other hand, is considered comparatively safe and effective in the immunocompromised group, but requires Section 21 motivation and is therefore not readily available. General practitioners, ophthalmologists and internists need to be more pro-active in recommending these vaccines to their patients to decrease the incidence of PHN, blinding ocular sequelae, and by extension rare potentially fatal complications such as cavernous sinus thrombosis. It is to be hoped that with escalation of vaccine coverage we will start to see a decline in these devastating and difficult-to-manage cases.
Teaching points
• Unusual elements of a history of diplopia should necessitate further investigation, as this is not in keeping with the natural progression of HZO.
• Lifting a ptotic upper lid to test ocular motility is the critical step in determining whether there is orbital and intracranial extension of HZO involving cranial nerves.
• Urgent neuro-imaging and a multidisciplinary approach with emergency definitive care leads to the best clinical outcomes.
• There is a need for increased herpes zoster vaccine coverage in SA to decrease the burden of this devastating disease.
Declaration. None.
Acknowledgements. None.
Author contributions. Sole author.
Funding. None.
Conflicts of interest. None.
References
1. Liesegang TJ. Herpes zoster ophthalmicus: Natural history, risk factors, clinical presentation and morbidity. Ophthalmology 2008;115(2 Suppl):S3-S12. [ Links ]
2. Gebo KA, Kolyani R, Moore RD, Polydefkis MJ. The incidence of, risk factors for, and sequelae of herpes zoster among HIV patients in the highly active antiretroviral therapy era. J Acquir Immune Defic Syndr 2005;40(2):169-174. [ Links ]
3. Adepoji FG, Olawumi HO, Adehoya BJ. HIV seropositivity and related eye disease in Utih, Ilorin. Niger Postgrad Med J 2007;14(2):163-165. [ Links ]
4. Palexas GN, Welsh NH. Herpes zoster ophthalmicus: An early pointer to HIV positivity in young African patients. Scand J Immunol Suppl 1992;11:67-68. [ Links ]
5. Vafai A, Berger M. Zoster in patients infected with HIV: A review. Am J Med Sci 2001;321(6):372-380. [ Links ]
6. Zaal MJW, Völker-Dieben HJ, D'Amaro J. Prognostic value of Hutchinson's sign in acute herpes zoster ophthalmicus. Graefes Arch Clin Exp Ophthalmol 2003;241(3):187-191. [ Links ]
7. Mehkri Y, Valisno JA, Rivas LF, et al. Management of cavernous sinus thrombosis following herpes zoster ophthalmicus. Cureus 2022;14(1):e21036. [ Links ]
 Correspondence:
Correspondence:
N Narainswami
neerannarainswami@gmail.com
Accepted 8 May 2023














