Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 no.9 Pretoria Set. 2023
http://dx.doi.org/10.7196/samj.2023.v113i9.500
RESEARCH
Time to thrombolysis and factors contributing to delays in patients presenting with ST-elevation myocardial infarction at Chris Hani Baragwanath Academic Hospital, Johannesburg, South Africa
I TickleyI; S A van BlydensteinII; R MeelIII
IMB ChB; Department of Internal Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IICert Pulmonology (SA), MMed (Int Med); Department of Internal Medicine and Division of Pulmonology, Faculty of Health Sciences, University of the Witwatersrand and Chris Hani Baragwanath Academic Hospital, Johannesburg, South Africa
IIICert Cardiology (SA), PhD; Department of Internal Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND: Acute coronary syndrome is a public health burden both worldwide and in South Africa (SA). Guidelines recommend thrombolysis within 1 hour of symptom onset and 30 minutes of hospital arrival for patients with ST-elevation myocardial infarction (STEMI) in order to prevent morbidity and mortality. There is a paucity of data pertaining to the time between onset of chest pain and thrombolysis in STEMI patients in SA
OBJECTIVES: To elucidate the time to thrombolytic therapy, establish the reasons for treatment delays, and calculate the loss of benefit of thrombolysis associated with delays in treatment of patients presenting with STEMI at Chris Hani Baragwanath Academic Hospital (CHBAH), Johannesburg, SA
METHOD: A prospective observational study of 100 consecutive patients with STEMI was conducted at CHBAH (2021 - 2022
RESULTS: The mean (standard deviation) age was 55.6 (11.6) years, with a male predominance (78%). Thrombolytic therapy was administered to 51 patients, with a median (interquartile range (IQR)) time to thrombolysis of 360 (258 - 768) minutes; 10 of the patients who received a thrombolytic (19.6%) did so within 30 minutes of arrival at the hospital. The median (IQR) time from symptom onset to calling for help was 60 (30 - 240) minutes, the median time from arrival of help to hospital arrival was 114 (48 - 468) minutes, and the median in-hospital delay to thrombolysis after arrival was 105 (45 - 240) minutes. Numerous reasons that led to delay in treatment were identified, but the most frequent was prehospital delays related to patient factors. Late presentation resulted in 26/49 patients (53.1%) not receiving thrombolytic therapy. Five patients died and 43 suffered from heart failure. Thirty per 1 000 participants could have been saved had they received thrombolytic therapy within 1 hour from the onset of chest pain
CONCLUSION: Prehospital and hospital-related factors played a significant role in delays to thrombolysis that led to increased morbidity and mortality of patients with STEMI
Acute coronary syndrome (ACS) is a public health burden that is on the rise owing to epidemiological transition and urbanisation that have led to an increased prevalence of non-communicable diseases[1] such as hypertension, dyslipidaemia and obesity. Cardiovascular disease is now the second most common cause of death in most African countries,[2] with mortality rates of 165.3 per 100 000 for white and 5.3 per 100 000 for black South Africans. Ischaemic heart disease ranked 8th for natural causes of death among adults, 5th for the age group >65 years and 7th in Gauteng Province, according to figures for South Africa (SA) for 2018.[3]
There are two approaches to the acute management of ST-elevation myocardial infarction (STEMI), thrombolysis and primary percutaneous coronary intervention (PCI), with guidelines recommending primary PCI as the preferred strategy if conducted timeously.[4] There is a paucity of data on the efficiency of management of patients with STEMI in the SA healthcare system. High-income countries (HICs) have adopted STEMI networks and protocols[5] to improve their treatment of patients, which has resulted in a 93% primary PCI rate at PCI-capable facilities.[5] At community facilities, 70% received primary PCI and 20% a thrombolytic agent.[5] India, which is considered a low- to middle-income country (LMIC), has also begun initiatives to improve management of STEMI through a non-profit organisation, STEMI India,[6] and the results from a pilot study have been promising.
The SA STEMI network[7] conducted an observational study at private health facilities that showed significant delays for patients requiring interfacility transfer, with 70% receiving reperfusion therapy at PCI-capable facilities and only 34% when interfacility transfer was required. In comparison, in SA public health facilities, Maharaj et al.[8] found that 67% of patients received thrombolysis in a retrospective multicentre study in Cape Town, and Meel and Gonçalves[9] noted a 37% thrombolysis rate in a prospective single-centre study in Pretoria.
In SA, thrombolytic therapy remains the primary method of treatment for STEMI owing to limited availability of PCI in public health facilities, as well as for those presenting to private health facilities without the funds to pay for PCI. There are very few data on primary PCI in public health facilities in SA. Gauteng, the country's most densely populated province, has 28 PCI-capable facilities[10] with an estimated 471 439 people per PCI facility. SA has 14 public PCI facilities in total, 6 of which are in Gauteng, and three provinces, namely North West, Northern Cape and Limpopo, do not have any PCI facilities in the public sector.
Thrombolysis, although an effective treatment option, is unfortunately time sensitive, with maximum benefit within the first hour after symptom onset.[11] Guidelines from the European Society of Cardiology (ESC)[4] and the American College of Cardiology (ACC)[12] recommend thrombolysis within 10 minutes of diagnosis and 30 minutes of hospital arrival.
There is, however, an observed disparity between guideline-recommended time frames and actual times patients encounter at Chris Hani Baragwanath Academic Hospital (CHBAH), Johannesburg. In order to assess the efficiency of the health system in providing treatment within these specified time frames, regular audits on the total ischaemic time (i.e. time of chest pain onset to thrombolysis), which includes the prehospital, transport and in-hospital time periods, and reasons for delays need to be conducted. These audits will provide feedback on the strengths and weaknesses of the system that can be utilised to make improvements and ultimately provide better care for patients with STEMI.
The primary objective of this study was to elucidate the time to thrombolysis and reasons for delays in administration or non-administration of thrombolytic agents to patients with STEMI presenting to CHBAH. Secondary objectives were to determine the demographics of patients presenting with STEMI, and their echocardiogram and coronary angiogram findings.
We hypothesised that patients presenting to CHBAH were not being thrombolysed within 30 minutes of arrival or within 1 hour of symptom onset.
Methods
This single-centre prospective observational study conducted at CHBAH in Soweto, Johannesburg, in 2001 and 2002 included 100 consecutive participants. The decision to have 100 participants was based on studies by Meel and Gonçalves[9] and Boersma et al.,[11] both of which included 100 patients in their analysis.
The CHBAH Cardiology Division provides services to the southern part of Gauteng as well as to North West Province, a total population of ~4 million people. Patients with a diagnosis of STEMI were identified through the medical admissions ward and the Coronary Care Unit at CHBAH, and were interviewed by the first author (IT) during their hospital admission. Inclusion criteria were patients aged >18 years with a diagnosis of STEMI based on the Fourth Universal Definition of Myocardial Infarction,[13] presenting to CHBAH directly or indirectly from surrounding referral hospitals with no absolute contraindication to thrombolysis. Exclusion criteria were an ACS other than STEMI and patient refusal to participate in the study.
Potential participants were given an information sheet, and informed consent was obtained. Those who were too ill were interviewed once they had stabilised. The medical records of those who died before they could be interviewed were used with ethics approval. A verbally administered survey was conducted by the first author to determine a timeline from onset of chest pain to thrombolysis and identify factors that contributed to delays. Factors contributing to delays were then divided into prehospital and in-hospital groups. Prehospital factors such as delays in seeking medical attention and transport to hospital were provided by the participants. In-hospital factors, from the time of arrival to thrombolysis, were provided by the participants and obtained from their medical records. Subgroup analysis was performed for in-hospital time to thrombolysis, comparing presentation to a public or a private health facility. In the interview, participants were asked about their time to obtaining an electrocardiogram (ECG), medical review and thrombolysis. These times were then compared between those who had initially presented to private or public health facilities to identify differences in how long it took to obtain an ECG, medical review and thrombolysis.
Further information, including echocardiogram findings, angiography findings, medications, complications and outcome were obtained from the participants' medical records.
Based on the benefits of early thrombolysis,[11] a delay in total time to thrombolysis was defined as a time >60 minutes from onset of chest pain to thrombolysis. In-hospital delays were defined according to the ESC and ACC guidelines[4,12] as a time >10 minutes from arrival at the hospital to obtaining an ECG, >10 minutes from the ECG to diagnosis, and >10 minutes from diagnosis to receiving a thrombolytic agent.
The information was captured on an Excel spreadsheet, version 2307 (Microsoft Corp., USA). Data were analysed using Stata 15 software (StataCorp, USA) and Excel version 2307.
The following equation from Boersma et al.[11] and also used by Meel and Gonçalves[9] was used to calculate the loss of benefit relative to the first hour based on time delay: f(x) = 19.4 - 0.6x + 29.3x - 1, where x is the treatment delay in hours and f(x) is the absolute benefit per 1 000 patients treated, expressed as a percentage (L(x) = 100(1 - f(x)/f (1)).
The study was approved by the Human Research Ethics Committee (Medical) of the University of the Witwatersrand (ref. no. M210 217).
Results
The demographic and clinical characteristics of the study participants are summarised in Table 1.
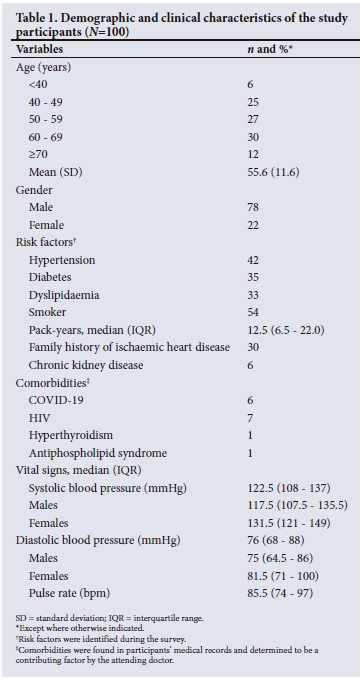
Participants' medications are summarised in Table 2. The majority of the patients were started on medical treatment during their hospitalisation. More than 90% were on antiplatelet, anticoagulant and lipid-lowering therapy. Eighty were on a beta-blocker and 50 were on an angiotensin-converting enzyme inhibitor.
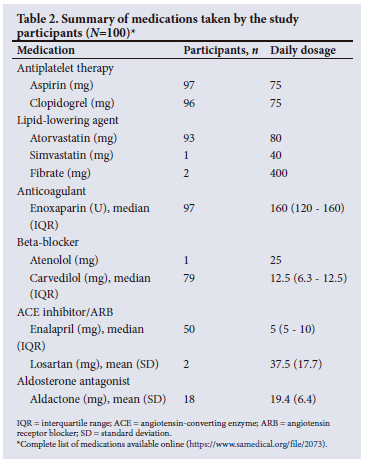
Fig. 1 illustrates the thrombolysis pattern of the study participants.
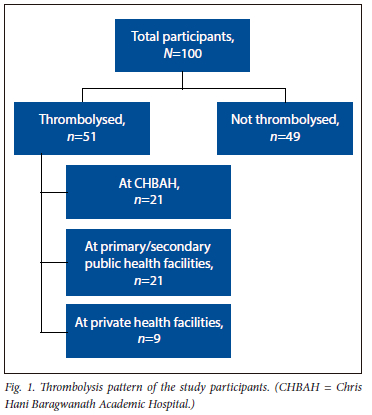
Sixty-five participants presented to hospital within 12 hours of symptom onset. Fifty-one were thrombolysed, 2 (3.9%) within 1 hour of symptom onset, 35 (68.6%) between 1 and 12 hours and 14 (27.5%) after 12 hours. Once participants arrived at the hospital, 10 (19.6%) received thrombolysis within 30 minutes of hospital arrival and 41 (80.4%) after 30 minutes. Forty-nine did not receive a thrombolytic agent, with late presentation being the most common reason for non-administration.
Prehospital delays
Participants' delays in seeking medical help resulted in a median (interquartile range (IQR)) delay of 60 (30 - 240) minutes in calling for help (Table 3). Reasons for the delays in seeking help included not being aware of the implications of the symptoms and/ or misinterpreting them as non-cardiac (gastritis, reflux) (28%), self-medicating (34%), and not wanting to disturb family members because the symptoms were mild, combined with the time of onset being during the night or in the early hours of the morning when family members were asleep (13%).
Arrival of help was defined as the arrival of a person capable of assisting the patient and arranging their transfer to the nearest health facility. The median (IQR) time from help arrival to first health facility arrival was 114 (48 - 468) minutes, with a median transport time from the place of chest pain onset to first health facility of 15 (10 - 20) minutes. Eighty-five participants called a family member or friend initially.
Of the participants, 73% used their private vehicle for transport to the health facility and 23% opted to use emergency medical services (EMS). Participants frequently (26%) cited ambulance delays from previous experiences or word of mouth as the reason for not calling an ambulance. Six called an ambulance, but the ambulance was delayed and they were forced to use their own vehicle. Two used public transport after a delayed response from EMS. One walked to their nearby health facility, and one was in CHBAH at the time of symptom onset. Four noted that there were health facilities close to their homes, so they did not consider calling an ambulance.
In-hospital delays
Sixteen participants first presented to a private health facility, 60 to a primary or secondary public health facility, and 24 directly to CHBAH. The median times from hospital arrival to ECG and review by a medical doctor are shown in Table 3.
A delay in obtaining an ECG was defined as >20 minutes from arrival at the health facility. Fifty-two participants had a delay in obtaining an ECG, for which the main reasons were the health facility being busy (n=38; 73.1%) and inappropriate triage (n=23; 44.2%). Some participants had more than one reason for delay. Despite complaints of chest pain, these patients were not immediately seen by a medical doctor. The median (IQR) time from the ECG to thrombolysis was 84 (18 - 222) minutes, with a busy health facility again being cited as the most common reason for delay (n=15/51; 29.4%). Other factors included awaiting transfer (n=12/51; 23.5%), either to another health facility because no thrombolytic agent was available, or to a high-care area prior to thrombolysis. Three (18.8%) of the 16 participants who initially presented to a private health facility had a delay in thrombolysis because the health facility requested payment before administration of a thrombolytic agent. The agents used for thrombolysis were alteplase (n=36; 70.6%), tenecteplase (n=5; 9.8%, only administered in private health facilities), and streptokinase (n=3; 5.9%); 7 participants (13.7%) were referred without documentation of the agent used.
Of the 49 participants who did not receive thrombolysis, 26 presented to hospital after 12 hours and were not eligible for thrombolysis, 16 were misdiagnosed, and in 8 cases there was no stock of a thrombolytic agent. Four participants arrived at CHBAH on the same day but were not thrombolysed owing to delays in transfer. Two had a cardiac arrest on arrival and were not thrombolysed because of fears of complications, and 5 did not have an ECG done at the primary or secondary health facilities, and were subsequently diagnosed on arrival at CHBAH so were out of the thrombolytic time window. Some participants had more than one reason for non-administration of thrombolysis.
Electrocardiogram and echocardiogram features
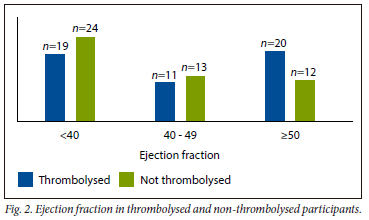
STEMI territories involved on the ECG (all participants) were 39 anterior, 34 inferior, 16 anteroseptal, 10 inferolateral and 1 in the anterolateral region. Echocardiograms were obtained for 99 articipants (one patient died before an echocardiogram could be done). Forty-three (43.5%) had an ejection fraction (EF) <40%, 24 (24.2%) had an EF of 40 - 49%, and 32 (32.3%) had an EF >50% (Fig. 2).
Regional wall motion abnormality was noted to be present in 97 reports (98.0%). The most frequent area involved was the anterior wall (56.7%), followed by the septal wall (51.1%), the inferior wall (41.1%) and the lateral and apical walls (21.1% each); 3.1% had global hypokinesia of the left ventricle.
Eighty-two participants had coronary angiograms. Two (2.4%) had a normal angiogram, and 18 (22.0%), 25 (30.5%), 30 (36.6%), and 7 (8.5%) had single-, dual-, triple- and quadruple-vessel disease, respectively. The vessel most commonly involved was the left anterior descending artery: 62 participants (75.6%) had stenosis, 10 12.2%) had a normal vessel, 9 (11.0%) had a total occlusion, and 1 (1.2%) had an ectatic vessel. Fifty-six participants (68.3%) had PCI, 15 (18.3%) were referred for a coronary artery bypass graft, and 11 (13.4%) had no intervention.
Complications
In the thrombolysis group, 4 patients had bleeding complications after thrombolysis, 2 had a cardiac arrest prior to thrombolysis, 5 were in cardiogenic shock requiring inotropic support, and 1 had a cerebrovascular accident during angiography. Three participants in this group died during their hospital admission.
In the non-thrombolysis group, 1 participant had cardiogenic shock and 2 died during their hospital admission. None had bleeding complications.
The benefit of fibrinolytic therapy was 42.1, 30.6 and 22.3 lives saved per 1 000 patients treated in the 1 - 2, 2 - 3 and 3 - 6 hours periods, respectively (Fig. 3).
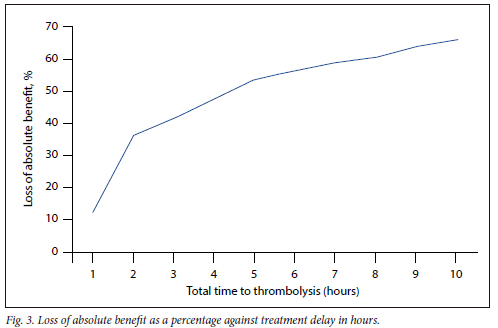
The mean loss of benefit expressed as a percentage relative to the first hour in the study sample was 47.5%. This translated into potentially saving an additional 30 per 1 000 patients had all been treated in the first hour in this study (i.e. 47.5%*65, where 65 = the number of people treated in the first hour in the reference dataset[11] from which the formula is derived).
Discussion
It has been established since the 1980s that early thrombolysis reduces morbidity and mortality in STEMI patients.[11,14-16] Forty years later, the present study has shown that only 51% of patients presenting to CHBAH received this intervention, and only 2 received it within 1 hour of symptom onset. How can this situation be improved, and is it a problem unique to Gauteng or SA? It is certainly not a problem unique to this study population, and the concept of a STEMI network and systems of care has been promoted for many years in STEMI guidelines set out by the ESC and ACC to improve care of STEMI patients. STEMI networks and systems of care are built around identifying the issues facing the population of a geographical area so that reperfusion through PCI or thrombolysis can be administered timeously through a multidisciplinary team of EMS, doctors and health facilities. In the study area, there is currently no STEMI network in place to improve the management of these patients. We hope that our study will bring this issue to light and that gaps in STEMI management in public health facilities will be addressed through upcoming networks such as STEMI SA.
Thirty-five patients presented to hospital 12 hours after onset of symptoms, with an overall median symptom-to-door time of 174 minutes. Delays were often due to misinterpretation of symptoms and self-medication, and many participants were not aware of the benefits of early thrombolysis. Participants frequently said that they took aspirin, thinking that it would cure their symptoms and not being aware that it is just an adjunct, with emergency thrombolysis or PCI being definitive care. Differentiating between heartburn and myocardial infarction is a dilemma frequently faced by people with chest pain. Patients with any risk factors for STEMI need to be counselled that obtaining an ECG would enable differentiation between these conditions, and that it should be done immediately so that appropriate treatment can be instituted.
Prehospital delays are not a problem unique to the SA setting, with both HICs and LMICs experiencing delays in symptom-to-door times,[17] e.g. 110 - 140 minutes in Beijing, China, 162 minutes in the USA, 130.5 minutes in Malaysia, and 250 - 290 minutes in India.[17] In Africa, times have been reported to range from 2.3 hours to 4.3 days.[18] SA studies had a mean symptom-to-door time of 90 minutes[9] and a median of 192.5 minutes,[8] with the present study showing a similar time. It is hoped that increasing awareness of early thrombolysis and addressing social and cultural barriers to seeking medical treatment through community education programmes will help reduce these times.
Underutilisation of EMS was notable in the present study. Most participants (73%) used private transport to get to their nearest health facility, which led to triage and in-hospital delays. The choice to use private transport was mainly due to mistrust in EMS due to time delays, as well as poor understanding of the role of the EMS, which goes beyond just being a means of transport. EMS play an important role in STEMI management: call centre staff can recognise a complaint as an emergency, and dispatch appropriately trained staff, who will assist in prehospital diagnosis, stabilisation and thrombolysis. EMS staff can provide emergency care, which includes obtaining an ECG, detecting fatal arrythmias, administering thrombolysis and pain management, and other lifesaving interventions. The Grampian Region Early Anistreplase Trial (GREAT)[19] compared mortality in patients who received prehospital thrombolysis with that in those who received thrombolysis in hospital. It was found that prehospital thrombolysis was not only as effective but was associated with decreased mortality (n=41/163; 25.2%) compared with the in-hospital group (n=53/148; 35.8%). In SA, the Durban University of Technology, which trains emergency medical staff, embarked on skills training in ECG interpretation and initiating prehospital thrombolysis by trained Advanced Life Support staff.[20] However, a subsequent follow-up study showed that this has not come to fruition, with multiple barriers to implementation including logistic issues, costs, and lack of a multidisciplinary approach.[21] A STEMI network will play a crucial role in implementing this strategy in the future.
The median arrival-to-thrombolysis time was 105 minutes, which is three and a half times the recommended 30 minutes. The reasons for the delays differed between health facilities, and there was a statistically significant shorter time for obtaining an ECG and medical review at private health facilities. At CHBAH, an ECG is done on arrival at the hospital, but ECGs are only interpreted later by a doctor. At primary public health facilities, an ECG is done on request by a doctor. At some facilities, the ECG machine was not in working order or an ECG was not done at all. Keeping in mind the guidelines recommending that an ECG be done within 10 minutes of first medical contact, measures need to be put in place to ensure that every health facility has a working ECG machine and that regular training is given to emergency staff so that the findings can be interpreted and acted upon immediately.
According to the SA primary healthcare and hospital treatment guidelines,[22,23] streptokinase is recommended in view of cost factors: 1.5 million U costs ~ZAR4 000, and alteplase 100 mg costs ZAR11 838.88.[24]
Despite its cost, streptokinase was not available at some primary and secondary public health facilities, with 12 patients receiving delayed thrombolysis because they arrived from other health facilities to CHBAH within the thrombolytic window and 4 not being thrombolysed at all because they arrived out of the thrombolytic window. There seems to be hesitancy with regard to administration of thrombolytic agents at primary care level. STEMI networks need to be put in place so that patients can access thrombolysis at all levels of care to expedite treatment. This wider access will also decrease the burden on the emergency departments at tertiary hospitals.
The SA hospital and primary healthcare guidelines must be updated to include recommendations to administer thrombolysis within 30 minutes of arrival at the health facility. The 2019 guidelines do not include a time period during which thrombolysis should be administered.[22] With regard to patients who attended a private health facility and were requested to pay before administration of thrombolysis, section 27 of the Constitution states that everyone has a right to access to healthcare services, and no one may be denied emergency medical treatment. Requesting payment prior to providing treatment is a breach of this constitutional right, and private health facilities should be held to this legal obligation.[25] Section 4 of the National Health Act 61 of 2003 states that emergency healthcare should not be limited based on nationality or immigration status, so these services must be available to all persons in SA.
None of the participants in the present study received primary PCI at CHBAH during the study period. Primary PCI use has increased in HICs, but this has not been the case in LMICs, and data on primary PCI rates in public health facilities in SA are scarce.[5,10,26] Thrombolysis is still the most-utilised treatment strategy for patients in the public health sector, and will continue to play an important role, as primary PCI requires a multidisciplinary team of skilled staff including an interventional cardiologist, radiographers, specialised nursing, a 24-hour PCI facility and an efficient EMS.
Heart failure in patients with ACS is a major complication leading to an increased risk of death, arrythmias, and re-admission with heart failure.[27-29] Systolic function is a parameter used on the echocardiogram to risk-stratify patients that has an impact on treatment and prognosis. We noted a high prevalence of heart failure post STEMI in this study, with 43 participants with an EF <40%, 55.8% of whom did not receive thrombolysis. It has been reported that ischaemic cardiomyopathy accounts for 7.7 - 9% of heart failure presentations in sub-Saharan Africa.[30] More recent studies on the prevalence and causes of heart failure in SA are scarce, and this is potentially an area for further research.
We noted that half of the participants in the present study received thrombolysis, which is an overall improvement from the 37% reported a decade ago at a similar tertiary centre in Gauteng.[9] However, the number of patients receiving thrombolysis within the first hour was dismal in both the current study (2 patients) and the previous study[91 (2 patients). In both studies, an additional 30 - 32 per 1 000 lives could have been saved had all the patients who received thrombolysis been treated within the first hour. Furthermore, the time delay before administration of thrombolysis (360 minutes in this study v. 270 minutes in the study by Meel and Gonçalves[9]) remains a major concern and calls for further resource diversion to implement and facilitate strategies to improve the care and outcome of patients with STEMI.
Study limitations
This study was conducted during the COVID-19 pandemic when SA's healthcare system was overburdened, with high patient numbers and a workforce that was experiencing physical and psychological fatigue. These factors may have influenced the study results. However, a recent observational study at CHBAH, published as an abstract[31] noted that the rates of thrombolysis just prior to and during the first peak of COVID-19 were unchanged. Patient recall bias and poor referrals from primary- and secondary-level hospitals are also factors that potentially influenced the data.
Conclusion
Thrombolysis, although a crucial management strategy, is not being adequately utilised in the public health sector. There are many factors affecting its appropriate implementation, with prehospital, EMS and in-hospital delays playing a significant role in delays to thrombolysis, which led to increased morbidity and mortality of patients with STEMI.
Declaration. The research for this study was done in partial fulfilment of the requirements for IT's MMed (Int Med) degree at the University of the Witwatersrand.
Acknowledgements. We express our gratitude to the patients for participating in this research, and to the staff in the CHBAH Coronary Care Unit, medical wards and medical records for their assistance.
Author contributions. IT: drafted the study protocol, collected and analysed data, wrote the manuscript, approved the final manuscript. SAvB: co-supervised, reviewed the drafted protocol, revised the manuscript, approved the final manuscript. RM: conceptualised the study, supervised, reviewed the drafted protocol, interpreted the results, revised the manuscript, approved the final manuscript.
Funding. None.
Conflicts of interest. None.
References
1. Tibazarwa K, Ntyintyane L, Sliwa K, et al. A time bomb of cardiovascular risk factors in South Africa: Results from the Heart of Soweto Study "Heart Awareness Days. Int J Cardiol 2009;132(2):233-239. https://doiorg/10.1016/j.ijcard.2007.1L067 [ Links ]
2. Mbewu A. The burden of cardiovascular disease in sub-Saharan Africa. SA Heart 2009;6(1):4-10. https://doi.org/10.24170/6-1-2005 [ Links ]
3. Statistics South Africa. Mortality and causes of death in South Africa: Findings from death notification: 2018. Statistical release P0309.3. Pretoria: Stats SA, 15 June 2021. https://www.statssa.gov.za/publications/P03093/P030932018.pdf (accessed 20 September 2022). [ Links ]
4. Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018;39(2):119-177. https://doi.org/10.1093/eurheartj/ehx393 [ Links ]
5. Claeys MJ, Sinnaeve PR, Convens C, et al. STEMI mortality in community hospitals versus PCI-capable hospitals: Results from a nationwide STEMI network programme. Eur Heart J 2012;1(1):40-47. https://doiorg/10.1177/2048872612441579 [ Links ]
6. Kaifoszova Z, Kala P, Alexander T, et al. Stent for Life Initiative: Leading example in building STEMI systems of care in emerging countries. EuroIntervention 2014;10(Suppl T): T87-T95. https://doi.org/10.4244/eijv10sta14 [ Links ]
7. Snyders A, Delport R. Referral pathways for reperfusion of STEMI - developing strategies for appropriate intervention: The SA Heart STEMI early intervention project. SA Heart 2015;12(2):74-80. https://doiorg/10.24170/12-2-1722 [ Links ]
8. Maharaj RC, Geduld H, Wallis LA. Door-to-needle time for administration of fibrinolytics in acute myocardial infarction in Cape Town. S Afr Med J 2012;102(4):241-244. [ Links ]
9. Meel R, Gonçalves R Time to fibrinolytics for acute myocardial infarction: Reasons for delays at Steve Biko Academic Hospital, Pretoria, South Africa. S Afr Med J 2015;106(1):92-96. https://doi.org/10.7196/SAMJ.2016.v106i1.9801 [ Links ]
10. Stassen W, Wallis L, Lambert C, Castren M, Kurland L. Percutaneous coronary intervention still not accessible for many South Africans. Afr J Emerg Med 2017;7(3):105-107. https://doi.org/10.1016/j.afjem.2017.04.009 [ Links ]
11. Boersma E, Maas AC, Deckers JW, Simoons ML. Early thrombolytic treatment in acute myocardial infarction: Reappraisal of the golden hour. Lancet 1996;348(9030):771-775. https://doi.org/10.1016/s0140-6736(96)02514-7 [ Links ]
12. O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: A report ofthe American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;61(4):e78-e140. https://doi.org/10.1016/j.jacc.2012.11.019 [ Links ]
13. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction (2018). Circulation2018;138(20):e618-e651. https://doi.org/10.1161/cir.0000000000000617 [ Links ]
14. White HD, van de Werf FJJ. Thrombolysis for acute myocardial infarction. Circulation 1998;97(16):1632-1646. https://doi.org/10.1161/01.cir.97.16.163 [ Links ]
15. Rovelli F, de Vita C, Feruglio GA, et al. GISSI trial: Early results and late follow-up. J Am Coll Cardiol 1987;10(5):33B-39B. https://doi.org/10.1016/s0735-1097(87)80426-6 [ Links ]
16. Sikri N, Bardia A. A history of streptokinase use in acute myocardial infarction. Tex Heart Inst J 2007;34(3):318-327. [ Links ]
17. Lim SC, Rahman A, Yaacob NM. Pre-hospital factors influencing time of arrival at emergency departments for patients with acute ST-elevation myocardial infarction. Malays J Med Sci 2019;26(1):87-98. https://doi.org/10.21315/mjms2019.26.1.8 [ Links ]
18. Yao H, Ekou A, Niamkey T, et al. Acute coronary syndromes in sub-Saharan Africa: A 10-year systematic review. J Am Heart Assoc 2022;11(1):e021107. https://doi.org/10.1161/jaha.120.021107 [ Links ]
19. Rawles JM. Quantification of the benefit of earlier thrombolytic therapy: Five-year results of the Grampian Region Early Anistreplase Trial (GREAT). J Am Coll Cardiol 1997;30(5):1181-1186. doi.org/10.1016/s0735-1097(97)00299-4 [ Links ]
20. Castle N, Naidoo R, Owen R Initiation of pre-hospital thrombolysis in South Africa. S Afr Med J 2006;96(1):28-31. [ Links ]
21. Lynch A, Sobuwa S, Castle N. Barriers to the implementation of prehospital thrombolysis in the treatment of ST-segment elevation myocardial infarction in South Africa: An exploratory inquiry. Afr J Emerg Med 2020;10(4):243-248. https://doi.org/10.1016/j.afjem.2020.08.001 [ Links ]
22. National Department of Health, South Africa: Essential Drugs Programme. Standard Treatment Guidelines and Essential Medicines List. 5th ed. Pretoria: NDoH, 2019: Chapter 3.2. https://knowledgehub.health.gov.za/system/files/elibdownloads/2023-04/Hospital%2520Level%2520%2528Adult%2529%25202019_v2.0.pdf (accessed 20 September 2022). [ Links ]
23. National Department of Health, South Africa: Essential Drugs Programme. Primary Healthcare Standard Treatment Guidelines and Essential Medicine List. 7th ed. Pretoria: NDoH, 2020: Chapter 4.4. https://knowledgehub.health.gov.za/system/files/elibdownjloads/2023-04/Primary%2520Healthcare%2520STGs%2520and%2520EML%25207th%2520edition%2520-%25202020-v2.0.pdf (accessed 20 September 2022). [ Links ]
24. National Department of Health, South Africa. Recommendation for alternative therapy for streptokinase. EDP022019/01. https://www.samedical.org/file/973 (accessed 20 September 2022). [ Links ]
25. Kramer E. 'No one may be refused emergency medical treatment' - ethical dilemmas in South African emergency medicine. S Afr J Bioethics Law 2008;1(2):53-56. https://hdl.handle.net/10520/EJC64473 (accessed 19 April 2023). [ Links ]
26. Kakou-Guikahue M, N'Guetta R, Anzouan-Kacou J-B, et al. Optimizing the management of acute coronary syndromes in sub-Saharan Africa: A statement from the AFRICARDIO 2015 Consensus Team. Arch Cardiovasc Dis 2016;109(6-7):376-383. https://doi.org/10.1016/j.acvd.2015.12.005 [ Links ]
27. Bahit MC, Kochar A, Granger CB. Post-myocardial infarction heart failure. J Am Coll Cardiol 2018;6(3):179-186. https://doi.org/10.1016/j.jchif.2017.09.015 [ Links ]
28. Alkhalil M, Kearney A, MacElhatton D, Fergie R, Dixon L. The prognostic role of mid-range ejection fraction in ST-segment elevation myocardial infarction. Int J Cardiol 2020;321:12-17. https://doi.org/10.1016/j.ijcard.2020.07.001 [ Links ]
29. Perelshtein Brezinov O, Klempfner R, Zekry SB, Goldenberg I, Kuperstein R. Prognostic value of ejection fraction in patients admitted with acute coronary syndrome. Medicine 2017;96(9):e6226. https://doi.org/10.1097/md.0000000000006226 [ Links ]
30. Kraus S, Ogunbanjo G, Sliwa K, Ntusi NAB. Heart failure in sub-Saharan Africa: A clinical approach. S Afr Med J 2015;106(1):23-31. https://doi.org/10.7196/SAMJ.2016.v106i1.10325 [ Links ]
31. Leon S, Meel R. Impact of the COVID-19 pandemic on acute coronary syndrome patients admitted to an urban academic hospital in Soweto, South Africa. Abstracts: SA Heart Congress 2021. SA Heart 2021;18(3):176. https://journals.co.za/doi/pdf/10.10520/ejc-saheart-v18-n3-a4 (accessed 20 August 2023). [ Links ]
 Correspondence:
Correspondence:
R Meel
ruchikameel@gmail.com
Accepted 12 June 2023














