Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 no.9 Pretoria sep. 2023
http://dx.doi.org/10.7196/samj.2023.v113i9.668
RESEARCH
Prevalence of comorbid disease and associated risk factors among homeless people living in temporary shelters during the COVID-19 lockdown in Tshwane, South Africa
T V PhiriI; N GloeckII, III; A MusekiwaIV
IBCMP, MPH; School of Health Systems and Public Health, Faculty of Health Sciences, University of Pretoria, South Africa
IIMB ChB, MSc (Clin Epidemiol); Department of Family Medicine, Faculty of Health Sciences, University of Pretoria, South Africa
IIIMB ChB, MSc (Clin Epidemiol); Health Systems Research Unit, South African Medical Research Council, Cape Town, South Africa
IVMSc, PhD; School of Health Systems and Public Health, Faculty of Health Sciences, University of Pretoria, South Africa
ABSTRACT
BACKGROUND: People experiencing homelessness are among the most socially and medically vulnerable populations
OBJECTIVES: To assess the prevalence of comorbid disease and associated risk factors among homeless people admitted to temporary shelters
in the City of Tshwane during levels 4 and 5 of the COVID-19 national lockdown in South Africa.
METHODS: A descriptive cross-sectional study design was used. The sample was drawn from secondary data on all individuals placed in temporary shelters constructed by Tshwane during levels 4 and 5 of the COVID-19 lockdown (26 March - 31 May 2020). Descriptive statistics were used to summarise data, and a multivariable logistic regression model was applied to determine factors associated with comorbid disease
RESULTS: The overall prevalence of comorbid disease among homeless people in temporary shelters in Tshwane was 28.8% (95% confidence interval (CI) 26.9 - 30.8). There was no significant difference in the prevalence of comorbid disease by illicit substance use (29.9% for users v. 29.5% for non-users; p=0.871). In adjusted analyses, being South African (adjusted odds ratio (aOR) 2.06; 95% CI 1.10 - 3.88; p=0.024), being female (aOR 3.73; 95% CI 1.85 - 7.53; p<0.001), being black (aOR 3.43; 95% CI 1.12 - 10.54; p=0.031) or white (aOR 6.11; 95% CI 1.55 - 24.0; p=0.01), and injecting substances (aOR 1.68; 95% CI 1.19 - 2.37; p=0.003) were significantly associated with having comorbid disease
CONCLUSION: The study found a 28.8% prevalence of comorbid disease among homeless people placed in temporary shelters in Tshwane. In adjusted analysis, being South African, being female, black and white race, and injecting substances were associated with having comorbid disease. Strengthening of public health interventions such as needle and syringe exchange programmes, family planning and access to primary care with health education could improve the healthcare of people experiencing homelessness
Methods
Study design
A descriptive cross-sectional study design was used. Secondary data were analysed using data collected during levels 4 and 5 of the COVID-19 national lockdown between 26 March and 31 May 2020.
Study setting
The study was conducted in temporary shelters provided by the City of Tshwane during the national lockdown. These shelters were placed in open fields in suburbs of Tshwane: Mabopane, Pretoria Central (Struben Street and Caledonian Stadium), Heuweloord, Akasia, Lyttleton and Danville.
Study population and sampling
The study population comprised homeless people aged >18 years, living in Tshwane and admitted to a temporary shelter during levels 4 and 5 of the national lockdown (26 March - 31 May 2020). Secondary data on 2 066 participants were collected for the study.
Measurements
The data were collected using the Phulukisa app (Phulukisa Health Solutions, SA) and the Qualtrics XM database (Qualtrics International Inc., UK). The questionnaire comprised questions on demographic characteristics, medical history and substance use history.
Data collection and analysis
The secondary data were collated into an Excel 2016 spreadsheet (Microsoft Corp., USA). Duplicate entries were removed using probabilistic matching. The variables used for probabilistic matching were name and surname, date of birth, date of specimen collection and physical address. The data were secured with a password for restricted access, and the data collected from participants were de-identified before analysis was performed. Data were analysed using Stata 17 software (StataCorp, USA), and the statistical analysis included determining the prevalence of comorbid disease, together with its 95% confidence intervals (CIs). Descriptive statistics in the form of counts and percentages were used to summarise categorical data, which were also displayed using bar charts. The x2 test was used to determine the association between two categorical variables. The multivariable logistic regression model was applied to determine the risk factors associated with comorbid disease. The potential risk factors were age in years, sex, race, nationality, education level, route of substance administration, type of substance used, daily number of bags of heroin used, and medical history. All variables with a p-value <0.2 in the univariate analyses were entered into the multivariable model using automatic backward elimination stepwise selection. Multi-collinearity tests were performed before entering variables in the multivariable model to ensure that only non-collinear variables were included. The final multivariable model was tested using the Hosmer-Lemeshow x2 goodness-of-fit test. A p-value <0.05 was considered statistically significant.
Ethics approval
The study received ethics approval from the University of Pretoria Faculty of Health Sciences Research Ethics Committee before it was conducted (ref. no. 625/2021). Ethical approval for Community Oriented Substance Use Programme (COSUP) (ref. no. 176/2019) and related COVID-19 research (ref. no. 310/2020) was obtained from the University of Pretoria Faculty of Health Sciences Research Ethics Committee. A letter of permission for use of the secondary data collected by COSUP staff was obtained from Prof. Jannie Hugo, Head of Family Medicine, University of Pretoria. The purpose and benefits of the study, the confidentiality of information, and the voluntary nature of participation in the study were explained to potential participants, and informed consent was obtained from them.
Consent to participate
Every participant's right to privacy was ensured, and the confidentiality of their medical information was ensured in accordance with the applicable laws and regulations. Every participant gave informed consent in form of a digital image agreement via the Phulukisa app and the University of Pretoria Qualtrics platform. Individuals who chose not to give an image were considered as declining to consent to participate. Participants did not incur any costs based on participation in the study, and no incentives to take part were given to them.
Results
Demographic characteristics
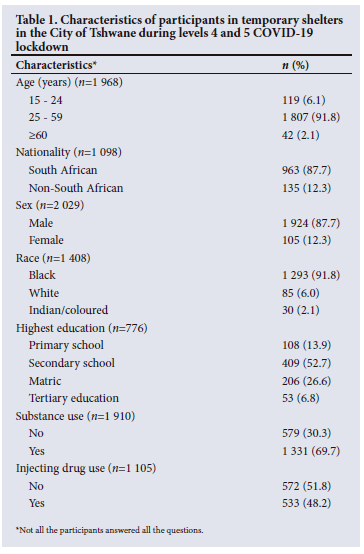
The study assessed the demographic characteristics of 2 066 homeless people who had been placed in temporary shelters in Tshwane. The majority were 25 - 59 years old (91.8%; n=1 807/1 968), with the number aged >60 years (2.1%; n=42) being the lowest. The majority were male (87.7%; n=1 924/2 029) and South African (87.7%; n=963/1 098). In terms of race, most were black (91.8%; n=1 293/1 408), followed by white (6.0%; n=85) and coloured/Indian (2.1%; n=30). In terms of highest education attained, most had secondary school education (52.7%; n=409/776). Approximately 70% of the participants were using illicit substances (69.7%; n=1 331/1 910), and 48.2% were injecting substances (48.2%; n=533/1 105) (Table 1).
Prevalence of comorbid disease and substance use
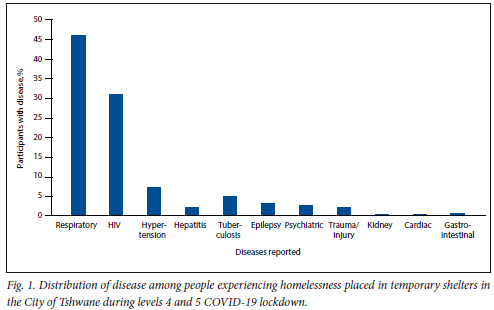
The overall prevalence of comorbid disease among homeless people placed in temporary shelters was 28.8% (95% CI 26.9 - 30.8). Nearly half of the participants (45.9%) were diagnosed with respiratory conditions such as asthma and bronchitis. Other conditions included HIV (31.0%), hypertension (7.3%), tuberculosis (4.8%), epilepsy (3.0%), psychiatric illness (2.9%), trauma/injury (2.1%), hepatitis (2.0%), kidney conditions (0.2%), cardiac conditions (0.2%) and gastrointestinal conditions (0.6%) (Fig. 1).
Prevalence of comorbid disease by substance use
The prevalence of substance use was found to be 69.7% (95% CI 67.6 - 71.4). There was no significant difference in the prevalence of comorbid disease in homeless people who used illicit drugs compared with those who did not (29.9%; n=398/1 331 v. 29.5%; n=171/579) (p=0.871).
Risk factors associated with comorbid disease
Table 2 summarises the results of the univariate and multivariate logistic regression analysis identifying factors associated with the prevalence of comorbid disease. In univariate analysis, being aged >60 years (odds ratio (OR) 2.97; 95% CI 1.43 - 6.17; p=0.004), being female (OR 2.52; 95% CI 1.70 - 3.74; p<0.001) and injecting drugs (OR 1.34; 95% CI 1.05 - 1.70; p=0.017) were significantly associated with having comorbid disease. In adjusted analyses, being South African (adjusted OR (aOR) 2.06; 95% CI 1.10 - 3.88; p=0.024), being female (aOR 3.73; 95% CI 1.85 - 7.53; p<0.001), being black (aOR 3.43; 95% CI 1.12 - 10.54; p=0.031) or white (aOR 6.11; 95% CI 1.55 - 24.0; p=0.01), and injecting substances (aOR 1.68; 95% CI 1.19 - 2.37; p=0.003) were significantly associated with comorbid disease. In multivariate analysis, age, highest education, substance use and bags of heroin used were not significantly associated with having comorbid disease among people experiencing homelessness.
Discussion
The objective of this study was to assess the prevalence of comorbid disease, the difference in the prevalence of comorbid disease according to substance use, and the risk factors associated with comorbid disease among people experiencing homelessness placed in temporary shelters in the City of Tshwane during levels 4 and 5 of the national COVID-19 lockdown (26 March - 31 May 2020). The findings of this study can inform the development of health interventions for people experiencing homelessness in SA.
The findings indicated that the prevalence of comorbid disease in homeless people placed in temporary shelters in Tshwane was 28.8% and that nearly half had respiratory conditions, followed by HIV and hypertension. Findings were similar in a study in the UK comparing people experiencing homelessness and those living in formal households.[7] The authors reported that people experiencing homelessness had higher prevalences of respiratory conditions, epilepsy and cardiac conditions. It has also been reported that people who experience homelessness have an increased prevalence of mental illness,[17] but this was not observed in our study. We found no significant difference in the prevalence of comorbid disease between people who used drugs and those who did not (29.9% v. 29.5%). In a cohort study by Reif et al.,[18] similar findings were found for alcohol- and drug-dependent individuals, with no significant effect of chronic medical disease on recent addiction treatment utilisation. The prevalence of substance use in the present study was 69.7%. This finding supports the literature that states that people experiencing homelessness have a higher prevalence of substance use than the general population. Illicit drug use is an important area of focus when dealing with healthcare for people experiencing homelessness.
The demographic findings of the present study are consistent with other estimates of the homeless population. We found that the majority of people who experienced homelessness in Tshwane were black South Africans, and that most were male (87.7%). The predominant age group was 25 - 59 years (91.8%). A study by Kok et al.[19] also showed that the homeless population living on the street comprised young working-age adults, who were mainly males. Olufemi et al.[20] reported similar results, noting that there were comparatively few females on the streets because these living conditions were very difficult for women. Our analysis showed that female sex, black and white race, South African nationality and injecting substances were associated with having comorbid disease. Females were more likely than males to exhibit these health risks, suggesting that service delivery needs should respond appropriately. There was a greater association between being white and having comorbid disease compared with being black, Indian or Coloured. We found that people experiencing homelessness who were South African had increased odds of having comorbid disease compared with non-South Africans. We also found that using illicit substances did not influence whether homeless people would have comorbid disease, but there was a significant correlation between having comorbid disease and injecting substances. The study by Scheibe et al.[16] illustrated that people who injected drugs had a high prevalence of infectious diseases (HIV and HCV), which agrees with the correlation observed in the present study. Furthermore, a study in Delhi by Saraswati et al.[21] reported a high prevalence of HIV infection, HCV infection and, more significantly, HIV-HCV co-infection among males who injected drugs. These factors should therefore be considered when planning interventions aimed at improving the healthcare of people experiencing homelessness.
Study limitations
This study analysed secondary data, which has its limitations. These include having no control over data collection, and certain variables having missing information. Secondly, we included a specific subsample of individuals ever experiencing homelessness, namely those placed in temporary shelters by the City of Tshwane. The findings in the study are based on self-reported responses and are therefore prone to recall bias and reporting of culturally or socially acceptable behaviours. Our study was cross-sectional, and we are unable to assign causal direction to the associations we observed.
Our study attempted to determine the prevalence of comorbid disease, to aid in health intervention for people experiencing homelessness in SA. However, the study did not address the underlying social exclusion that is key to improving the healthcare of people experiencing homelessness. There is no information regarding use of certain specific healthcare services that are significant to the homeless population. A research study focusing on the effects that homelessness has on people accessing and using various health services, especially women, could be a future focus in research.
Conclusion
This study assessed the prevalence of comorbid disease and factors associated with it in people experiencing homelessness placed in temporary shelters, to assist in the development of health interventions that are specifically targeted for them. The study found a high prevalence of comorbid disease among these people, showing that they have an increased risk of being affected by more than one condition that can worsen their health and prolong their state of being homeless. There was no difference in the prevalence of comorbid disease between participants who did and did not use illicit drugs. In multivariate analysis, the study found that nationality, being female, race and injecting substances were significantly associated with having comorbid disease. These factors should therefore be addressed when planning interventions that target people experiencing homelessness.
Declaration. None.
Acknowledgements. We thank the University of Pretoria Department of Family Medicine's Community Oriented Primary Care Research Unit, under which the COSUP falls, for allowing us access to the data used in this analysis.
Author contributions. TVP drafted the manuscript with input from NG and AM. TVP performed data analysis with input from AM. All authors contributed to development of the manuscript, and reviewed and approved the final version.
Funding. None.
Conflicts of interest. None.
References
1. Rule-Groenewald C, Timol F, Khalema E, Desmond C. More than just a roof: Unpacking homelessness. HSRC Review. https://repository.hsrc.ac.za/bitstream/handle/20.500.11910/1997/8591.pdf?sequence=1&isAllowed=y (accessed 20 October 2022). [ Links ]
2. Tyler KA, Ray CM. Risk and protective factors for substance use among youth experiencing homelessness. Child Youth Serv Rev 2019;107:288-296. https://doi.org/10.1016/j.chÜdyouth.2019.104548 [ Links ]
3. Morrison DS. Homelessness as an independent risk factor for mortality: Results from a retrospective cohort study. Int J Epidemiol 2009;38(3):877-883. https://doi.org/10.1093/ije/dyp160 [ Links ]
4. Ayano G, Belete A, Duko B, Tsegay L, Dachew BA. Systematic review and meta-analysis of the prevalence of depressive symptoms, dysthymia and major depressive disorders among homeless people. BMJ Open 2021;11(2):e040061. https://doi.org/10.1136/bmjopen-2020-040061 [ Links ]
5. Beijer U, Wolf A, Fazel S. Prevalence of tuberculosis, hepatitis C virus, and HIV in homeless people: A systematic review and meta-analysis. Lancet Infect Dis 2012;12(11):859-870. https://doi.org/10.1016/S1473-3099(12)70177-9 [ Links ]
6. Ford PJ, Cramb S, Farah CS. Oral health impacts and quality of life in an urban homeless population. Aust Dent J 2014;59(2):234-239. https://doi.org/10.1111/adj.12167 [ Links ]
7. Lewer D, Aldridge RW, Menezes D, et al. Health-related quality of life and prevalence of six chronic diseases in homeless and housed people: A cross-sectional study in London and Birmingham, England. BMJ Open 2019;9(4):e025192. https://doi.org/10.1136/bmjopen-2018-025192 [ Links ]
8. Bowen M, Marshall T, Yahyouche A, et al. Multimorbidity and emergency department visits by a homeless population: A database study in specialist general practice. Br J Gen Pract 2019;69(685):e515-e525. https://doi.org/10.3399/bjgp19X704609 [ Links ]
9. Roy E, Boudreau JF, Leclerc P, Boivin JF, Godin G. Trends in injection drug use behaviors over 10 years among street youth. Drug Alcohol Depend 2007;89(2-3):170-175. https://doi.org/10.1016/j.drugalcdep.2006.12.025 [ Links ]
10. McNeil R, Guirguis-Younger M. Illicit drug use as a challenge to the delivery of end-of-life care services to homeless persons: Perceptions of health and social services professionals. Palliat Med 2012;26(4):350-359. https://doi.org/10.1177/0269216311402713 [ Links ]
11. Torchalla I, Strehlau V, Li K, Krausz M. Substance use and predictors of substance dependence in homeless women. Drug Alcohol Depend 2011;118(2-3):173-179. https://doi.org/10.1016/j.drugalcdep.2011.03.016 [ Links ]
12. Teesson M, Hodder T, Buhrich N. Alcohol and other drug use disorders among homeless people in Australia. Subst Use Misuse 2003;38(3-6):463-474. https://doi.org/10.1081/JA-120017382 [ Links ]
13. Glasser I, Zywiak WH. Homelessness and substance misuse: A tale of two cities. Subst Use Misuse 2003;38(3-6):551-576. https://doi.org/10.1081/JA-120017385 [ Links ]
14. United Nations Office on Drugs and Crime. World Drug Report 2021, booklet 3. https://www.unodc.org/unodc/en/data-and-analysis/wdr2021.html (accessed 23 October 2022). [ Links ]
15. United Nations Office on Drugs and Crime. World Drug Report 2019, booklet 3. https://wdr.unodc.org/wdr2019/ (accessed 9 July 2020). [ Links ]
16. Scheibe A, Young K, Moses L, et al. Understanding hepatitis B, hepatitis C and HIV among people who inject drugs in South Africa: Findings from a three-city cross-sectional survey. Harm Reduct J 2019;16(1):28. https://doi.org/10.1186/s12954-019-0298-2 [ Links ]
17. Substance Abuse and Mental Health Services Administration (SAMHSA). Current statistics on the prevalence and characteristics of people experiencing homelessness in the United States (last updated July 2011). https://www.samhsa.gov/sites/default/files/programs_campaigns/homelessness_programs_resources/hrc-factsheet-current-statistics-prevalence-characteristics-homelessness.pdf (accessed 23 October 2022). [ Links ]
18. Reif S, Larson MJ, Cheng DM, et al. Chronic disease and recent addiction treatment utilization among alcohol and drug dependent adults. Subst Abuse Treat Prev Policy 2011;6:28. https://doi.org/10.1186/1747-597X-6-28 [ Links ]
19. Kok P, Cross C, Roux N. Towards a demographic profile of the street homeless in South Africa. Dev South Afr 2010;27(1):21-37. https://doi.org/10.1080/03768350903519309 [ Links ]
20. Olufemi O. Feminisation of poverty among the street homeless women in South Africa. Dev South Afr 2000;17(2):221-234. https://doi.org/10.1080/713661399 [ Links ]
21. Saraswati LR, Sarna A, Sebastian MP, et al. HIV, hepatitis B and C among people who inject drugs: High prevalence of HIV and hepatitis C RNA positive infections observed in Delhi, India. BMC Public Health 2015;15:726. https://doi.org/10.1186/s12889-015-2003-z [ Links ]
 Correspondence:
Correspondence:
A Musekiwa
alfred.musekiwa@up.ac.za
Accepted 20 July 2023














