Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 n.9 Pretoria Sep. 2023
http://dx.doi.org/10.7196/samj.2023.v113i9.724
RESEARCH
Perinatal outcome of maternal deaths at Chris Hani Baragwanath Academic Hospital, Johannesburg, South Africa, January 2014 - June 2019
N Msibi-AfolayanI; M NchinyaniI; F L NakwaII; Y AdamI
IMB BCh, FCOG (SA); Department of Obstetrics and Gynaecology, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIMB BCh, FC Paed (SA); Department of Paediatrics and Child Health, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND: Maternal death is a tragic event. Of maternal deaths worldwide, 99% occur in low- and middle-income countries. Perinatal outcome is related to maternal wellbeing. Maternal death has a negative impact on fetal and neonatal outcome in the short and long term
OBJECTIVES: To determine the perinatal outcomes of pregnancies that ended in a maternal death at Chris Hani Baragwanath Academic Hospital (CHBAH), Johannesburg, South Africa, over a 5-year period, to describe the causes of maternal death, and to determine the stillbirth rate (SBR) and early neonatal death (ENND) rate in this population
METHODS: This was a retrospective cross-sectional study of maternal deaths in women with a viable pregnancy from January 2014 to June 2019 at CHBAH. All maternal deaths with gestation >26 weeks or fetal weight >500 g were included in the study. Information on demographics, booking status, antenatal care, pregnancy outcome, and fetal and neonatal outcome was extracted from maternal and neonatal files
RESULTS: Of a total of 183 maternal deaths during the study period, 147 were included in the study. The institutional maternal mortality ratio was 135 deaths per 100 000 live births. Hypertension was the main direct cause of death (36.5%; n=27/74), followed by pregnancy-related sepsis (27.4%; n=21/74) and obstetric haemorrhage (20.6%; n=15/74). Non-pregnancy-related infections, of which 91.4% were HIV and HIV-related complications, comprised 47.9% (n=35/73) of indirect causes of death, followed by medical and surgical disorders. Of a total of 151 babies, including two sets of twins and one set of triplets, 137 were delivered and 14 were undelivered at the time of maternal death. Ninety-one babies (61.9%) were born alive and 51 (34.6%) were stillbirths. Of the 91 liveborn infants, 6 (6.5%) had an ENND. Of the 51 stillbirths, 14 (27.5%) were undelivered and 11 (21.6%) were delivered by perimortem caesarean section. The SBR was 347 per 1 000 maternal deaths and the ENND rate 66 per 1 000 live births. The perinatal mortality rate (PMR) was 388 per 1 000 maternal deaths, which is 12 times higher than the PMR per 1 000 live births for the general population
CONCLUSION: Women who experience maternal death have babies with very poor perinatal outcomes, with a very high SBR, ENND rate and PMR. The health of the mother has a direct and significant effect on fetal and neonatal outcomes
Maternal mortality is still a global challenge, with the maternal mortality ratio (MMR) in low- and middle-income countries (LMICs) at least 14 times greater than in high-income countries (HICs).[1] The full impact of maternal deaths on families and communities has yet to be fully understood, with minimal research in this field.[2] The global MMR came down from 342 to 211 deaths per 100 000 live births between 2000 and 2017.[1] This represents a 38% reduction in the global MMR, with an estimated 2.9% annual decrease.[1] Data collected by the World Health Organization (WHO) show that 99% of maternal deaths occur in LMICs, especially in Africa.[3] In the 2017 - 2019 Saving Mothers and Babies report, the MMR in South Africa (SA) was 154 per 100 000 live births in the 2014 - 2016 triennium and 113.8 per 100 000 in the 2017 - 2019 triennium.[4]
The causes of maternal mortality are grouped as direct, indirect and incidental.[5] Direct causes of maternal death are a consequence of complications or management of the pregnancy and delivery, e.g. hypertension, haemorrhage and puerperal sepsis.[5] Indirect causes of maternal mortality are described as death of a pregnant woman with a pre-existing or newly developed health problem unrelated to pregnancy, for example cardiac disease and non-pregnancy-related infections (NPRIs) such as HIV/AIDS.[5] Incidental or non-obstetric maternal deaths are deaths with causes not linked to pregnancy, such as trauma and violence.[5] Reducing maternal deaths remains a global priority.[5] According to the WHO, the perinatal mortality rate (PMR) is the number of deaths of fetuses weighing at least 500 g (or, when birthweight is unavailable, after 22 completed weeks of gestation) plus the number of early neonatal deaths (ENNDs) per 1 000 total births.[6] The definition of stillbirth in SA is any fetus that has died after 28 weeks or 1 000 g.[7] Perinatal mortality is a measure of maternal healthcare, wellbeing and nutritional status along with fetal wellbeing. It also indicates the quality of care offered antenatally, intrapartum, postpartum and during the neonatal period.[8]
Millennium Development Goals 4 and 5 are aimed at improving child and maternal health and mortality, respectively.[9] Maternal wellbeing directly affects the fetal and neonatal outcome, as the fetus is directly dependent on the mother for survival. Maternal deaths are indicative of maternal health and functional adequacy of the healthcare system. Also, fetal health is directly related to maternal health.[10] To improve perinatal wellbeing, it is therefore of paramount importance to assess maternal health and healthcare during the antenatal and intrapartum periods, as well to optimise postpartum care of the baby. Not enough work has been done to assess perinatal outcomes in relation to maternal death.
Maternal and perinatal outcomes are intrinsically related, and initiatives focused on optimising one often have an impact on the other.[8] In sub-Saharan Africa, obstructed labour, abnormal fetal presentation and hypertensive diseases of pregnancy have been shown to increase the risk of perinatal mortality by more than fivefold and result in more than a third of all perinatal deaths.[7] Preterm birth, infection, hypertensive disease and intrapartum asphyxia are major contributors to perinatal deaths in LMICs.[1] A study in Tanzania showed that infants orphaned within 42 days of birth had a probability of surviving to 1 year of only 52.0%.[11]
Under-5 child mortality in SA fell from 56 to 36 deaths per 1 000 live births between 2009 and 2014, and infant mortality from 39 to 28 per 1 000 during the same period.[12] However, there has been minimal change in neonatal deaths in SA, with the neonatal mortality rate remaining at 11 - 12 per 1 000 live births between 2012 and 2015.[13] The PMR was highest at 24.3 per 1 000 in 2009, and lowest at 21 per 1 000 in 2016.[7] According to Statistics South Africa, national stillbirths fell from 15.6 to 13.5 deaths per 1 000 total births between 2003 and 2016.[7]
Chris Hani Baragwanath Academic Hospital (CHBAH) is a referral centre for seven midwife obstetric units, a district hospital and two regional hospitals in Gauteng Province and two regional hospitals in North West Province. The perinatal outcomes of pregnancies that end in maternal death at CHBAH are unknown. This study aimed to analyse the perinatal outcomes of these pregnancies at CHBAH to improve infant and child survival at the institution.
Methods
Setting and study design
This was a retrospective cross-sectional study conducted at CHBAH, a tertiary hospital in Soweto, an urban area of mixed informal settlements and formal housing in Johannesburg.[14] The Department of Obstetrics and Gynaecology has high volumes of patients, with 111 551 deliveries and 108 920 live births between January 2014 and June 2019. The study included all women with a pregnancy of at least 26 weeks' duration or who delivered a baby weighing >500 g, who died at CHBAH from January 2014 to June 2019. At CHBAH, fetal viability is defined as estimated gestational age of >26 weeks or a birthweight of >800 g. The study population included the neonates and stillbirths born to these women. All maternal deaths are discussed at the weekly departmental maternal mortality and morbidity meetings, where the cause of death is evaluated and the death notification form completed.
Data collection
The following information was taken from the maternal records: demographic information (age, parity, employment), and pregnancy-related factors (history, booking status, antenatal care, blood results, comorbidities, mode of delivery). The following information was extracted from the neonatal files: weight, sex, Apgar scores, admission status, and outcomes related to that admission.
Statistical analysis
Data were entered in the REDCap (Research Electronic Data Capture) online database manager, then exported to Excel version 16.3 (Microsoft Corp., USA) for data cleaning and data quality checks. Data were transferred to Stata version 14 (StataCorp, USA) for statistical analysis. Categorical variables were described with frequencies and percentages, and continuous variables with means and standard deviations (SDs) or medians and interquartile ranges (IQRs).
The stillbirth rate (SBR) was calculated by dividing the number of stillbirths by the total number of maternal deaths during the study period and expressing this per 1 000. Undelivered fetuses were also documented as stillbirths for statistical purposes. The ENND rate was estimated by dividing the number of deaths during the first 7 completed days of life by the total number of live births among the maternal deaths during the study period and expressing this per 1 000.
Means were compared with a f-test (if two groups) or analysis of variance (if more than two groups). Medians were compared with a rank-sum test (if two groups) and the Kruskal-Wallis test (if more than two groups). Frequencies were compared with a x2 test, and with Fisher's exact test if the cell size was <5. A p-value <0.05 was considered statistically significant.
Ethical considerations
Ethical approval was obtained from the University ofthe Witwatersrand Human Research Ethics Committee (ref. no. M1911143). Approval was also obtained from the chief executive officers at CHBAH and from the Department of Obstetrics and Gynaecology. Patient confidentiality was always ensured, and anonymity was secured by use of study numbers.
Results
Baseline characteristics of the study population
Of a total of 183 maternal deaths at CHBAH during the study period, 147 were included in this study; 34 were excluded because the gestational age was <26 weeks and 2 due to missing information. The institutional MMR was 135 deaths per 100 000 live births. Most of the women (n=85; 57.8%) were unemployed, 26 (17.7%) were employed, and in 36 (24.5%) the employment status was unknown.
Table 1 shows the general characteristics of the study population. The median (IQR) parity was 1 (0 - 2; range 0 - 7), and the median (IQR) gravidity was 3 (2 - 4; range 1 - 7). The mean (SD) gestational age at booking was 20.2 (7.7) weeks, and the mean (SD) gestational age at the time of death was 33.8 (4.6) weeks.
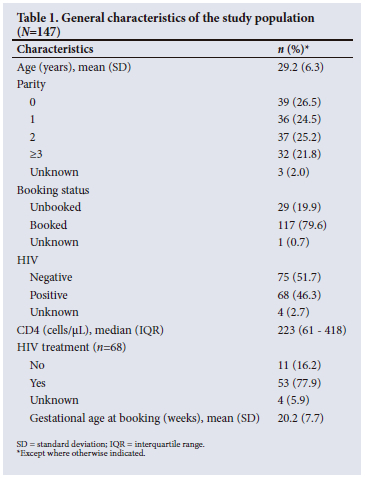
Antenatal and past obstetric history
Of the women, 22 (15.0%) had had a previous miscarriage, 3 (2.0%) a previous ectopic pregnancy and 1 (0.7%) a termination of pregnancy. The median (IQR) gestational age at booking was 20 (16 - 24; range 3 - 39) weeks, and the mean (SD) haemoglobin concentration at booking was 11.2 (2.3) g/dL. Two women (1.4%) were Rh negative. Most women (94.6%; n=139) had negative rapid plasma reagin (RPR) test results and 5 (3.5%) had unknown RPR status. A total of 68 women (46.3%) were HIV positive and 53 (77.9%) were on treatment. The median (IQR) duration of antiretroviral treatment was 5 (3 - 12; range 1 - 106) months. The median (IQR) CD4 count was 223 (61 - 418; range 3 - 2 467) cells/ uL. Of the 41 patients who had viral load results, 11 (26.8%) had a lower than detectable viral load. The median (IQR) viral load for those with a detectable viral load was 17 583 (420 - 462 000) copies/mL.
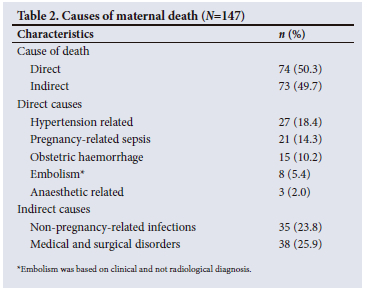
Causes of maternal death
Of the maternal deaths, ~80% were in the postpartum period. Table 2 shows the causes of maternal death. Hypertension was the leading direct cause of maternal death, followed by pregnancy-related sepsis, obstetric haemorrhage and embolism. Of the deaths indirectly caused by NPRIs (n=35), 32 (91.4%) were a result of HIV and related complications. Of the deaths indirectly caused by medical and surgical disorders (n=38), 34.3% were due to cardiac disease and 14.8% to respiratory disease.
Delivery outcomes
Over two-thirds of the women (69.4%; n=102) delivered by caesarean section, 30 (20.4%) had a normal vaginal delivery (NVD), 14 (9.5%) were undelivered, and 1 (0.7%) had a laparotomy for extrauterine pregnancy. Of the total caesarean section deliveries in the study, 80 (78.4%) were emergencies, 3 (2.9%) elective and 19 (18.6%) perimortem caesarean sections. Of the 30 NVDs, 26 (86.7%) were spontaneous and 4 (13.3%) were induced. There were 90 preterm deliveries in the study, of which 42 (46.7%) ended as stillbirths.
Perinatal outcomes
There was a total of 151 babies, as there were two sets of twins and one set of triplets. One hundred and thirty-seven babies were delivered and 14 were undelivered at the time of maternal death. There were 51 stillbirths, including the 14 undelivered fetuses. The SBR was 347 per 1 000 births. Table 3 shows the perinatal outcomes with the relevant rates. In 18 cases (11.0%) the neonatal outcome data were incomplete owing to missing data and poor record keeping. The PMR was 388 per 1 000 births. Among 38 paediatric admissions with reasons for admission, the most common reason was prematurity (39.5%; n=15), followed by respiratory distress (23.7%; n=9) and low Apgar scores (15.8%; n=7).
Table 4 compares perinatal outcomes for direct v. indirect causes of maternal death. The mean GA at time of birth or death was significantly lower in the group with indirect causes of death compared with the group with direct causes. The group with direct causes of maternal death had significantly more live births. Indirect causes of maternal deaths were associated with a significantly higher rate of undelivered infants and a significantly higher rate of preterm births.
Table 5 compares fetal outcomes according to when in the perinatal period the mother died. The median GA at delivery did not differ significantly between the antenatal, intrapartum and postpartum maternal death groups (p=0.21). Mothers who died during the postpartum stage had a significantly higher rate of live births (72.7%), and the antenatal death group had a significantly higher rate of undelivered fetuses (77.8%) (p<0.001). Birthweight did not differ significantly between the three maternal death groups.
With regard to causes of maternal death, gestational age at the time of delivery was highest for obstetric haemorrhage (median (IQR) 38 (34 - 39) weeks) and lowest for NPRIs (30 (28.5 - 33.0) weeks) (p<0.01) (Table 6). There was no significant difference in neonatal outcomes according to specific causes of death (p=0.243). The NPRI group had a significantly higher rate of preterm births compared with the other causes of maternal death (p=0.002).
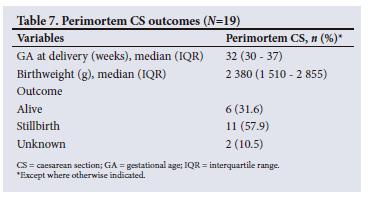
Perimortem caesarean section
Table 7 shows perimortem caesarean section outcomes. Documents were missing for 2 of the fetuses delivered by perimortem caesarean section, and their outcome is unknown. The deaths of women who had a perimortem caesarean section were mostly from NPRIs (36.8%; n=7) with tuberculosis (TB) and Pneumocystis pneumonia (PCP) as the cause of death, followed by thromboembolic disease (21.0%; n=4) with pulmonary embolus and amniotic fluid embolus as the cause, hypertension (15.7%; n=3), diabetic ketoacidosis (10.5%; n=2), and abruptio placentae, asthma and peripartum cardiomyopathy at 5.3% (n=1) each. Perimortem caesarean deliveries had similar outcomes to total maternal deaths in terms of a predisposition towards preterm deliveries and low birthweight, but the SBR was higher.
Discussion
This study determined the causes of maternal death and perinatal outcomes over a 5-year period. It is the first study to use routinely collected data to report perinatal outcomes in association with maternal deaths in SA.
The institutional MMR was 135 per 100 000 live births. This MMR is much higher than the national MMR of 113.8 per 100 000 live births in the 2017 - 2019 triennium,[4] probably because CHBAH receives many critical and high-risk patients. The PMR at CHBAH during the study period specific to women who had a maternal death was higher than the rate in the general SA population (388 per 1 000 maternal deaths v. 30.9 per 1 000 live births, respectively).[4] The PMR for CHBAH during the study period was 36 per 1 000 births, showing that the maternal death population has more catastrophic perinatal outcomes even compared with the high-risk population at CHBAH. Our study highlights the dire perinatal outcomes associated with maternal death, as the PMR in this group is 12 times higher than that of the general population. Perinatal mortality is a comprehensive indicator for estimating the true level of mortality around the time of delivery, as it analyses both live births and stillbirths in the target population studied.[15] The study also revealed extremely high stillbirth and ENND rates. The SBR was 347 per 1 000 births with maternal death, which is 17 times higher than the national SBR and 14 times higher than the SBR at CHBAH during the study period. The maternal death population has these much higher rates because it is a high-risk population, and a sick mother is more likely than a healthy one to have a sick fetus or one that dies. The ENND rate of 66 per 1 000 live births with maternal death was equally troubling, at 6 times higher than the national rate and 5 times higher than the rate for the CHBAH population during the study period, as babies born to mothers who die are already compromised and therefore have a predisposition to neonatal death. Furthermore, many of the babies in this study were preterm and vulnerable to the associated complications, which can lead to death. Prematurity is the driver of neonatal deaths in SA.[13] We have been able to find no studies that looked at the SBR, ENND rate and PMR specific to the maternal death population in SA.
A WHO systematic analysis showed that globally almost 75% of maternal deaths were due to direct causes, mainly haemorrhage (27.1%, nearly as high as all indirect causes at 27.5%), hypertensive disorders and sepsis.[16] These causes are similar to those reported in SA, where NPRIs, hypertension, obstetric haemorrhage and pregnancy-related sepsis, as well as medical and surgical diseases, predominated in a 2012 report.[17] However, this profile differs from that in HICs, for example the UK, where the leading causes of direct and indirect maternal deaths were reported as thromboembolism and cardiac disease, respectively.[18] HIV infection has been recognised as having a major effect on maternal deaths in SA,[17] and it continues to be the leading cause of maternal death, as our study shows. HIV and its complications were the most common cause of death, even with improved HIV testing and an almost 80% treatment rate. More work needs to be done in terms of early detection and treatment of opportunistic infections, as many of our patients died from TB and PCP, which are preventable and treatable diseases.
Most of the mothers who died delivered via caesarean section. Of the caesarean sections, almost 80% were emergency procedures and almost 19% perimortem procedures. Almost two thirds of the deliveries were preterm, which is associated with an increased risk of neonatal death,[19] as is also seen in the general obstetric population at CHBAH.
The present study shows that indirect causes of maternal death were significantly associated with lower gestation at birth and lower birthweight compared with direct causes of death. Indirect causes of maternal death are health problems that do not provide an optimal environment for fetal growth and survival. The survival of a fetus in utero is dependent on several factors. These can be broken down into the wellbeing of the fetus in its environment, the function of the uteroplacental unit, and the condition of the environment in which the fetus lives. A single insult or a combination of factors may lead to stillbirth.[20] A study conducted in SA, Tanzania and Malawi suggested that pregnancy accelerates HIV disease progression owing to the immunosuppression associated with pregnancy.[21] An HIV-positive woman experiences a double hit from the pregnancy and the disease, which increases her likelihood of opportunistic infections and their complications. Because the fetus is dependent on the mother for its growth and survival, its risk of morbidity and mortality is significantly raised. The authors of that study further posited that NPRIs and HIV-related conditions such as pulmonary TB, pneumonia and hypertension increase mortality in pregnant and postpartum women.[21]
In the present study, antenatal maternal death was associated with a higher rate of stillbirths (total and undelivered) compared with intrapartum or postnatal deaths. Most antenatal maternal deaths occurred in the preterm period, and most of the causes of death were comorbid conditions that have a direct effect on maternal health and therefore fetal health. Most of the antenatal maternal deaths were due to NPRIs. The hypertension group had the most live births and the NPRI group the most undelivered stillbirths and preterm births and the lowest birth weights. The reason for this observation is not clear, but it could be related to the fact that the fetus is affected by comorbid conditions, which may be associated with an increased rate of placental insufficiency and poor fetal growth and survival.[22]
Perimortem caesarean delivery is a means of saving the fetus if the mother dies. The literature suggests that the procedure should be performed within 4 minutes to minimise neurological damage to the fetus. If the mother has a resuscitable cause of death, perimortem caesarean section may make it possible to revive her.[23] In the present study, approximately one-fifth of the caesarean sections were perimortem procedures. More than half of the infants were of low birthweight, and almost two-thirds were stillborn. These cases have a high maternal and perinatal mortality rate.[23]
Study limitations
The study took place at a tertiary hospital that deals with a high-risk population, so the study findings may not be generalisable to the SA population as a whole. The study was based on routine clinical data, and some information was missing. The maternal data collected are not routinely linked to the perinatal outcomes data. The study also focused on early neonatal outcomes and not late neonatal (7 - 30 days of life) outcomes.
A strength of the study is that the causes of maternal death were determined by a multidisciplinary team.
Conclusion
Maternal deaths are associated with poor perinatal outcomes. The causes of the deaths in the present study were similar to maternal deaths in the 2017 - 2019 Saving Mothers and Babies report.[4] The worst perinatal outcomes were associated with maternal death in the antenatal period, and these deaths were mainly due to indirect causes. Mothers who died of NPRIs had infants with poor perinatal outcomes. Of the poor fetal and neonatal outcomes, stillbirth was the most common. Maternal death was associated with very high stillbirth and ENND rates.
While strides have been made in initiation of antiretroviral therapy for HIV, we need to focus on opportunistic infections and adherence to treatment. We suggest that routinely collected data on maternal deaths include perinatal outcomes as a standard. Prenatal care may assist in optimising the health of women with comorbidities, and future research needs to evaluate prenatal care and its effects on preventing maternal deaths and thus improving perinatal outcomes. More work also needs to be done to improve HIV programmes and prevent HIV-related opportunistic infections, as these are still a leading cause of maternal death and poor perinatal outcomes.
Declaration. The research for this study was done in partial fulfilment of the requirements for NM-A's MMed (Obstet Gynaecol) degree at the University of the Witwatersrand.
Acknowledgements. NM-A thanks her family and friends for their love and support.
Author contributions. NM-A and YA: conceptualisation and design of the study. NM-A: data collection and interpretation and drafting of the manuscript. FLN: revised the neonatal data. NM-A, MN and YA: revised and approved the final manuscript.
Funding. None.
Conflicts of interest. None.
References
1. World Health Organization. Trends in maternal mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Geneva: WHO, 2019. https://www.unfpa.org/featured-publication/trends-maternal-mortality-2000-2017 (accessed May 2020). [ Links ]
2. Moodley J, Fawcus F, Pattinson R. Improvements in maternal mortality in South Africa. S Afr Med J 2018;108(3a):s4-s8. https://doi.org/10.7196/SAMJ.2018.v108i3.12770 [ Links ]
3. Mmusi-Phetoe RMM. Social factors determining maternal and neonatal mortality in South Africa: A qualitative study. Curationis 2016;39(1):1571. https://doi.org/10.4102/curationis.v39i1.1571 [ Links ]
4. National Department of Health, South Africa. Saving Mothers and Babies 2017 - 2019: Executive Summary. Pretoria: NDoH, 2020. https://www.health.gov.za/wp-content/uploads/2023/05/SAVING-MOTHERS-SAVING-BARIES-REPORT-2017-2019.pdf (accessed June 2020). [ Links ]
5. Lumbiganon P, Laopaiboon M, Intarut N, et al. Indirect causes of severe adverse maternal outcomes: A secondary analysis of the WHO Multicountry Survey on Maternal and Newborn Health. BJOG 2014;121(Suppl 1):32-39. https://doi.org/10.1111/1471-0528.12647 [ Links ]
6. World Health Organization. Neonatal and perinatal mortality: Country, regional and global estimates. Geneva: WHO, 2006. https://apps.who.int/iris/bitstream/handle/10665/43444/9241563206_eng.pdf?sequence=1&isAllowed=y (accessed May 2020). [ Links ]
7. Statistics South Africa. Perinatal deaths in South Africa 2014. Statistical release P0309.4. Pretoria: Stats SA, 27 October 2016. http://www.statssa.gov.za/publications/P03094/P030942014.pdf (accessed May 2020). [ Links ]
8. Allanson ER, Muller M, Pattinson RC. Causes of perinatal mortality and associated maternal complications in a South African province: Challenges in predicting poor outcomes. BMC Pregnancy Childbirth 2015;15:37. https://doi.org/10.1186/s12884-015-0472-9 [ Links ]
9. Hug L, Alexander M, You D, Alkema L; UN Inter-agency Group for Child Mortality Estimation. National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: A systematic analysis. Lancet Glob Health 2019;7(6):e710-e720. https://doiorg/10.1016/S2214-109X(19)30163-9 [ Links ]
10. Lassi ZS, Majeed A, Rashid S, Yakoob MY, Bhutta ZA. The interconnections between maternal and newborn health - evidence and implications for policy. J Matern Fetal Neonatal Med 2013;26(Supp1 1):3-53. https://doi.org/10.3109/14767058.2013.784737 [ Links ]
11. Finlay JE, Moucheraud C, Goshev S, et al The effects of maternal mortality on infant and child survival in rural Tanzania: A cohort study. Matern Child Health J 2015;19(11):2393-2402. https://doi.org/10.1007/s10995-015-1758-2 [ Links ]
12. Nkonki LL, Chola LL, Tugendhaft AA, Hofman KK. Modelling the cost of community interventions to reduce child mortality in South Africa using the Lives Saved Tool (LiST). BMJ Open 2017;7(8):e011425. https://doi.org/10.1136/bmjopen-2016-011425 [ Links ]
13. Rhoda N, Velaphi S, Gebhardt GS, Kauchali S, Barron P. Reducing neonatal deaths in South Africa: Progress and challenges. S Afr Med J 2018;108(3a):s9-s16. https://doi.org/10.7196/SAMJ.2017.v108i3b.12804 [ Links ]
14. Uzabakiriho B, Maswime S. Causes of maternal death at Natalspruit Hospital, Johannesburg, South Africa. S Afr Med J 2019;109(6):412-414. https://doi.org/10.7196/SAMJ.2019.v109i6.13215 [ Links ]
15. Akombi BJ, Renzaho AM. Perinatal mortality in sub-Saharan Africa: A meta-analysis of demographic and health surveys. Ann Glob Health 2019;85(1):106. https://doi.org/10.5334/aogh.2348 [ Links ]
16. Say L, Chou D, Gemmill A, et al Global causes of maternal death: A WHO systematic analysis. Lancet Glob Health 2014;2(6):e323-e333. https://doi.org/10.1016/S2214-109X(14)70227-X [ Links ]
17. Chweneyagae D, Delis-Jarrosay N, Farina Z, et al The impact of HIV infection on maternal deaths in South Africa. S Afr J Obstet Gynaecol 2012;18(3):70-76. [ Links ]
18. Knight M, Nair M, Tuffnell D, et al, eds; MBRRACE-UK. Saving lives, improving mothers' care: Surveillance of maternal deaths in the UK 2012 - 14 and lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2009 - 14. Oxford: National Perinatal Epidemiology Unit, University of Oxford, 2016 https://www.npeu.ox.ac.uk/assets/downloads/mbrrace-uk/reports/MBRRACE-UK%20Maternal%20Report%202016%20-%20website.pdf (accessed July 2020). [ Links ]
19. MacDorman MF, Thoma M, Declercq E, Howell EA. The relationship between obstetrical interventions and the increase in U.S. preterm births, 2014 - 2019. PLoS ONE 2022;17(3):e0265146. https://doi.org/10.1371/journal.pone.0265146 [ Links ]
20. Maslovich MM, Burke LM. Intrauterine fetal demise (updated 31 October 2022). Treasure Island, Fla.: StatPearls Publishing, 2023. https://www.ncbi.nlm.nih.gov/books/NBK557533/ (accessed February 2023). [ Links ]
21. Calvert C, Marston M, Slaymaker E, et al Direct maternal deaths attributable to HIV in the era of antiretroviral therapy: Evidence from three population-based HIV cohorts with verbal autopsy. AIDS 2020;34(9):1397-1405. https://doi.org/10.1097/QAD.0000000000002552 [ Links ]
22. Wardinger JE, Ambati S. Placental insufficiency (updated 3 October 2022). Treasure Island, Fla.: StatPearls Publishing, 2023. https://www.ncbi.nlm.nih.gov/books/NBK563171/ (accessed February 2023). [ Links ]
23. Katz VL. Perimortem cesarean delivery: Its role in maternal mortality. Semin Perinatol 2012;36(1):68-72. https://doi.org/10.1053/j.semperi.2011.09.013 [ Links ]
 Correspondence:
Correspondence:
N Msibi-Afolayan
nomshado.msibi@gmail.com
Accepted 29 June 2023














