Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 no.9 Pretoria Set. 2023
http://dx.doi.org/10.7196/samj.2023.v113i8.16706
RESEARCH
Longitudinal data resource from the Wellbeing of Older People cohort of people aged >50 years in Uganda and South Africa from 2009 to 2019
J O MugishaI; A EdwardsII; N NaidooIII; S ChatterjiIII; J SeeleyI, II; P KowalIII
IPhD; Medical Research Council/Uganda Virus Research Institute, and London School of Hygiene and Tropical Medicine Uganda Research Unit, Entebbe, Uganda
IIPhD; Africa Health Research Institute, Durban, South Africa
IIIPhD; World Health Organization Study on global AGEing and adult health (SAGE), Geneva, Switzerland
ABSTRACT
BACKGROUND: The population of people aged >60 years continues to increase globally, and has been projected by the United Nations Population Division to increase to 21% of the total population by 2050. In addition, the number of older people living with HIV has continued to increase owing to the introduction of antiretroviral therapy as a treatment for HIV-infected people. Most of the older people living with HIV are in sub-Saharan Africa, an area that faces the biggest burden of HIV globally. Despite the high burden, there are limited reliable data on how HIV directly and indirectly affects the health and wellbeing of older people within this region
OBJECTIVE: To showcase the availability of data on how HIV directly and indirectly affects the health and wellbeing of older people in Uganda and South Africa (SA
METHODS: The World Health Organization Study on global AGEing and adult health (SAGE), in collaboration with Medical Research Council/Uganda Virus Research Institute and London School of Hygiene and Tropical Medicine (MRC/UVRI and LSHTM) Uganda
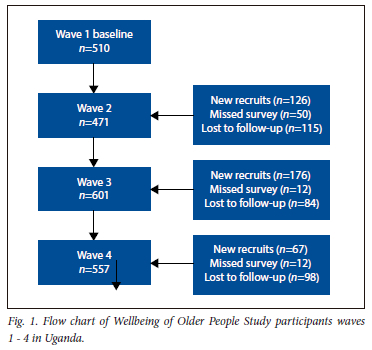
Research Unit and the Africa Health Research Institute (AHRI) in SA, started the SAGE Wellbeing of Older People Study (WOPS) in Uganda and SA in 2009. Since initiation, respondents have been surveyed every 2 years, with four waves of surveys conducted in Uganda and three waves in South Africa.
RESULTS: The available datasets consist of two cohorts of people, aged >50 years, who were surveyed every 2 years between 2009 and 2018. The prevalence of HIV positivity over this period increased from 39% to 54% in Uganda and 48% to 62% in SA. The datasets provide comparisons of variables at a household level and at an individual level. At the individual level, the following measures can be compared longitudinally for a 10-year period for the following variables: sociodemographic characteristics; work history and benefits; health states and descriptions; anthropometrics performance tests and biomarkers; risk factors and preventive health behaviours; chronic conditions and health services coverage; healthcare utilisation; social cohesion; subjective wellbeing and quality of life; and impact of caregiving
CONCLUSION: This article describes the WOPS in Uganda and SA, the population coverage of this study, and the survey frequency of WOPS, survey measures, data resources available, the data resource access and the strengths and weaknesses of the study. The article invites interested researchers to further analyse the data and answer research questions of interest to enhance the impact of these data
The number of older people living with HIV continues to increase globally. This is mainly due to the introduction of antiretroviral drugs, which have improved the survival of people living with HIV,[1-3] and due to populations of older people who are acquiring new HIV infections.[4] As of 2020, an estimated 21% of all people living with HIV, >6.5 million people, were aged >50 years.[5] Most of these older people living with HIV reside in sub-Saharan Africa. Despite the increase in the number of older people living with HIV, there are limited reliable data on HIV and ageing in the African region.[6-9] Reliable data on HIV and ageing, and how these individually and combined affect the health of older people in low- and middle-income countries, will provide knowledge about health and social needs and facilitate interventions for improved health maintenance as people age. Longitudinal research in multiple settings has provided reliable data about the health and wellbeing of older people with and without HIV within Africa, with results that can be used for effective planning for both health and social programmes for this ageing population.[10-12]
In order to fill these data gaps, the World Health Organization (WHO), in collaboration with Medical Research Council, Uganda Virus Research Institute (MRC/UVRI), and London School of Hygiene and Tropical Medicine (LSHTM) Uganda Research Unit and the Africa Centre surveillance area (presently the Africa Health Research Institute (AHRI)) in South Africa (SA) developed and implemented the Study on global AGEing and adult health (SAGE) Wellbeing of Older People Study (WOPS). In Uganda and SA, WOPS cohorts are open cohorts of people aged >50 years living with and without HIV. These cohorts were established in 2009 as part of WHO SAGE.[13]
SAGE is a longitudinal study on the health and wellbeing of adult populations as well as the ageing process.[13] The target population has been people who are >50 years, but it has also collected data from a comparison sample of younger adults aged 18 - 49 years in each wave. SAGE WOPS in both Uganda and SA has collected longitudinal data on people >50 years directly or indirectly affected by HIV/AIDS. The main aim of WOPS in both Uganda and SA
has been to study the health and wellbeing of older people living with and without HIV, with special emphasis on the effects of the introduction of antiretroviral therapy (ART) on older people living with HIV.
For the WOPS in Uganda and SA, older people were defined by the World Health Organisation as those aged >50 years. This definition was based on the fact that the life expectancy in most of the sub-Saharan African (SSA) countries was very low by 2009, owing to the HIV/AIDS epidemic and also the fact that most of the people aged >50 years in SSA were already grandfathers and mothers.[14] In addition, the WHO based this on the fact that by age 50 most of the people in Africa were already affected by extreme poverty and diseases of ageing, including non-communicable diseases. Since its inception in 2009, four waves of WOPS have been undertaken in Uganda, and the fifth wave was underway at the time of writing this article, while three waves have been completed in SA.
Objective
To add to the body of knowledge by providing reliable data on HIV and ageing, and how these individually and combined effect the health of older people in low- and middle-income countries (LIMCs). The main aim of this article is to describe the data and data resources available from multiple waves of SAGE WOPS in Uganda and SA. Specifically, we describe the study settings and population coverage, survey frequency, survey measures, the data resources available, and strengths and areas that may need improvement in future WOPS surveys. Lastly, we also describe the sociodemographic characteristics of the study respondents at each wave of WOPS. Our objective is to attract collaborating researchers to further analyse the data and publish impactful outcomes to influence future research and policy implementation that will improve the wellbeing of older people in LMICs.
Methods
Design
The research design for this study was longitudinal, multisite, prospective and cross-sectional. The survey was conducted every 2 years or as close to 2 years as possible at the two sites. Three data collection waves were completed in SA, and four in Uganda. In SA, the first wave took place between 2009 and 2010. The second wave took place between 2013 and 2015. The third wave took place between 2016 and 2017. The fourth wave took place in Uganda only in 2019. During each wave, respondents of the previous waves who were alive and still living in the survey area were traced and interviewed.
Setting and participants Study setting in Uganda
In Uganda, WOPS surveys were implemented at two sites in rural southwest Uganda (in Kalungu and Masaka districts) and one site in southern Uganda (Wakiso district) in and around Entebbe town near Kampala, the capital city of Uganda. Since 1989, the MRC/UVRI and LSHTM, Uganda Research Unit has been conducting HIV/AIDS-related epidemiological and clinical studies in these populations. Specifically, HIV/AIDS epidemiological studies have been ongoing within the general population cohort (GPC) that is located in Kalungu district.[15] Clinical studies have been ongoing at the Masaka site[16] and in and around Entebbe where the MRC/UVRI and LSHTM Uganda research site has its headquarters.[17] Within these study settings, use of antiretroviral drugs for treatment of people infected with HIV began in 2004, and presently all people living with HIV can access antiretroviral drugs at Uganda Ministry of Health-affiliated ART treatment centres within the WOPS site settings.
The Ugandan participants
For the initial recruitment of study respondents in WOPS Wave 1, a list was created of all people >50 years from existing MRC cohorts, from which a random sample of 510 study respondents were selected. The sample included the following groups of respondents:
(i) older persons who were living with HIV but not yet on ART;
(ii) older persons living with HIV and on ART for at least 1 year; (iii) three groups of older people who were not living with HIV who had a child living with HIV; (iv) people who had a child who died of AIDS-related illness; and (v) had not lost any child due to HIV infection (each group was equally represented in the study sample, with 100 participants per each group). The reason for stratification of the sample (for both Uganda and SA) into these different categories was to study the differences in health and wellbeing between these groups. However, when ART guidelines changed to start ART for everyone living with HIV (at wave 3), there were fewer people who were dying of HIV/AIDS, and therefore fewer people available to be strategised into the groups. The original rationale for adding a group of older persons who had lost their adult children as a result of HIV/AIDS was to study the indirect effects of HIV on the health and wellbeing of older people. For example, if an older person lost an adult child to HIV/ AIDS, they would take on the responsibility of caring for their grandchildren, which was likely to impact on their health and wellbeing.[18,19] However, since this was a longitudinal study over a very long period, and developments in medicine meant that the study objectives had to be adjusted slightly to be more aligned with the context, from wave 3 onwards we stratified the sample into two categories, i.e. older people living with HIV and those living without HIV. This change in sampling did not affect the study other than that there were fewer available data to evaluate the impact of losing a child to the disease.
For WOPS in Uganda, HIV testing was done following the Ministry of Health of Uganda testing algorithm. The algorithm for HIV rapid testing consisted of an initial screening with the rapid test, Determine HIV1/2 (Abott Diagnostics Medical Co, Ltd., Japan). If the test result was negative, the participant was given a diagnosis of HIV-negative with no further rapid testing. If the test result was positive, the sample was retested with the rapid test HIV 1/2 Stat-Pak (Chembio Diagnostic System, Inc., USA). If both tests gave a positive result, the participant was given a diagnosis of HIV-positive with no further rapid testing. If the tests give discordant results (i.e. one positive and the other negative), the sample was further evaluated with the rapid test SD Bioline (Standard Diagnostics Inc., Republic of Korea). For those samples assessed by all three tests, two positive test results were interpreted as a positive diagnosis. If two of the three tests gave negative results, then the participant was considered to be HIV-negative. At each study wave, follow-up participants who were HIV-negative in the previous wave were retested in order to avoid misclassification.
In waves 2, 3 and 4, we re-interviewed those respondents from wave 1 who were still living in the area at the time of the initial interviews. In addition, at each wave, we replaced all the study respondents who were known to have died to maintain the study cohort sample size, taking into account the additional risk of death in cohorts involving older people. All sample replacements were randomly selected from among older people in the same study populations, stratified for gender, HIV status and age. In wave 2, 437 respondents were interviewed, in wave 3, 600 study respondents and wave 4, 557 study respondents.
Participant characteristics in the Uganda cohort are outlined in Tables 1 - 3 by data collection waves.
Study setting in South Africa
In SA, WOPS was implemented at the AHRI, previously the Africa Centre for Population and Health. AHRI is located in the Mpukunyoni tribal area, Hlabisa subdistrict, northern rural KwaZulu-Natal, SA.
South African participants
The SAGE-WOPS cohort at AHRI gathered data on persons aged >50 years, which included people living with HIV during three survey waves (2010, 2013 and 2017). The WOPS cohort enrolled individuals purposively selected from the AHRI Demographic Surveillance Area (DSA).[20] In waves 1 and 2, respondents were enrolled to represent four groups: (i) HIV-positive on ART for >1 year; (ii) HIV-positive not on ART or on ART for <3 months; (iii) HIV-negative having an adult child aged 18 - 49 on ART for >1 year; and (iv) HIV-negative having an adult child aged 18 - 49 who died of HIV-related causes. However, there was considerable overlap between these groups in wave 2, mainly owing to the changes in availability of ART over time, and therefore in wave 3 the sample was only stratified by gender, age and HIV status.
In SA, it was decided not to select a comparison group because of the extensive nature of the HIV epidemic in this setting, where the majority of families had experience of someone being affected or infected. The SA cohort is embedded in the larger health surveillance dataset where this information is kept. To avoid research fatigue, the same questions were not asked in both the surveillance and the WOPS study, but further analysis is required to link the identifiers for the participants. The purpose of the present article is to highlight the availability of these data in the hope that students and collaborators interested in the data would agree to work with us to put them to further use.
In SA, the final numbers of recruited respondents were 422 in wave 1, 512 in wave 2 and 726 in wave 3. We re-interviewed wave 1 WOPS respondents who were still living in the area in subsequent waves, and, as in Uganda, we replaced all respondents who were known to have died or moved away. An oversampling rate of 20% was used in wave 3 to allow for refusals (n=4) and/or individuals who could not be located (n=24 died, n=3 moved away). The number of respondents who took part in all three waves in SA was 338.
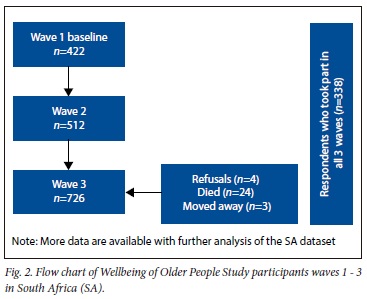
Participant characteristics in the SA cohort are outlined in Table 2 by data collection waves.
WOPS survey measures
For both Uganda and SA, a standardised questionnaire adapted from WHO SAGE[21] was used in the WOPS surveys. In addition, standardised methods, interviewer training and translation protocols of the questionnaire to the local language were used in both countries. The SAGE household and individual questionnaires (see Table 3 included the following six sections: (i) respondent and household characteristics, the number of adult members of the household >18 years and those <18 years, living conditions, assets and household income, household and family support networks and social networks, transfers to family, friends, community and governments; (ii) descriptions of health (with self-reported information about mobility, self-care, pain and discomfort, cognition, interpersonal activities, sleep and energy, affect, vision and wellbeing; (iii) self-reported chronic diseases including arthritis, stroke, hypertension, chronic lung disease (including tuberculosis and asthma), angina, depression, diabetes, cataracts/eye health, oral health, hearing (from wave 3) and injuries and physical disability; (iv) healthcare utilisation and risk factors and behaviours (including healthcare use, health are/clinic/hospital stays, HIV tests and results, tobacco use, alcohol use and diet; (v) care-giving and care-receiving (with information about caregiving roles and responsibilities, characteristics of any deceased child(ren) of respondent, residence history of deceased child(ren) of respondent, sickness and treatment knowledge, personal care, health/nursing care, physical assistance, financial assistance, health impact, overall health and financial expenses and implications and assessment of satisfaction with caregiver's role; (vi) objective health measurements including anthropometrics, performance tests and biomarkers (such as blood pressure, weight, height, waist circumference, normal and rapid timed walking speeds, vision tests (both distant and near vision), hand grip strength and cognitive processing as measured through verbal recall and verbal fluency.
Dried blood spots (DBS) were collected from consenting respondents. The DBS were collected for studying the relationship between biomarkers and a number of outcomes. These biomarkers included C-reactive protein, D-dimer, IL6, human apolipoproten and HbA1c. Biomarker data have been related to a frailty phenotype.[22] In wave 3, saliva samples were obtained for storage and later genetic testing (via Oragene OG-500 kits). The samples are stored in the AHRI biorepository and available to collaborators for further investigation. Saliva contains a wide range of genetic data that can be used for genetic research and clinical diagnostic purposes. Analysis of these samples for the many biomarkers that can be identified in saliva may lead to description of comorbidities of conditions and disease that appear in this cohort.
A summary of the main measures for waves 1 - 4 is shown in Table 3.
In Uganda, in addition to administering the study questionnaire, a verbal autopsy (VA) questionnaire was administered to the next of kin of any WOPS respondents who died between the WOPS rounds. The VA questionnaire was administered to determine the probable cause of death of the deceased WOPS respondent. The VA autopsy questionnaire used was adapted from the WHO 2007 VA questionnaire.[23-25] Data generated from the VA have not been analysed.
Research ethics committee approval
We obtained ethical clearance from the Uganda Virus Research Institute Research and Ethics Committee (ref. no. GC/127/19/04704), the Uganda National Council for Science and Technology (ref. no. SS4982) and the London School of Hygiene and Tropical Medicine (ref. no. 17640). Approval was also obtained from the WHO Ethical Review Committee (ref. no. RPC-149). In SA, ethical clearance was approved by the Biomedical Research Ethics Committee of the University of KwaZulu-Natal (ref. no. BF 136/09).
Discussion
The WOPS longitudinal dataset from two rural environments provides a platform and rich data to describe and interrogate the health and wellbeing of older people living with and without HIV in the SSA region. Since the study was conducted in both Uganda and SA, comparisons on the health and wellbeing of older people can be done from within the eastern and southern Africa regions.
A number of peer-reviewed publications have been published from the WOPS study in both Uganda and SA (appendix https://www.samedical.org/file/2057), in addition to a number of presentations at national and international conferences. Further analysis of this dataset has the potential to provide researchers from multiple disciplines with new insights in the changing landscape of the HIV epidemic.
Based on the data available, potential disciplines that could use the data include, but are not limited to, gerontologists, social scientists, social workers, policy makers, psychologists, public health clinicians, epidemiologists, statisticians, healthcare workers, chronic disease clinicians, pulmonologists, language therapists, audiologists, physiotherapists, occupational therapists, dieticians, HIV clinicians and disability practitioners, to name the main disciplines. The longitudinal data will allow these disciplines to explore and describe aspects of health and wellbeing of older people, directly and indirectly, affected by the HIV epidemic.
Conclusion
Some of the research questions that could be explored from this data and comparisons made between the regions are:
• How has caregiving for family members living with HIV changed over the period when HIV treatment regimens have changed?
• What is the impact of community involvement and social networks on the quality of life of older people in rural LMICS settings? How do these factors impact the older persons' wellbeing? Does HIV infection influence the phenomenon of wellbeing in older people and quality of life? Does social cohesion play a role in quality of life and health and wellbeing of older people living with HIV?
• How do older people access healthcare in different African regions, and how have healthcare utilisation practices changed as the epidemic has evolved? Does HIV infection influence patterns of healthcare utilisation for older people, and what do the findings indicate to policy makers who plan healthcare utilisation services?
• How do we characterise the prevalence of multimorbidity of conditions such as diabetes, hypertension, cataracts, edentulism, cervical and breast cancer, and these conditions' comorbidity with HIV?
• How do lifestyle factors such as tobacco and alcohol use interact with HIV, and how do they impact health and wellbeing among older people in rural settings?
• How can measures of disability inform the development of interventions to support older people in rural settings?
Many other research questions could be answered from this database considering the wide range of measures listed in Table 3 and recorded at both sites. Describing the data in this data set through the data profile article aims to raise awareness of the opportunity for researchers and students to utilise and collaborate with other researchers interested in factors that affect the health and wellbeing of older people living with and without HIV infection.
The SAGE website (www.who.int/healthinfo/systems/sage) and specifically the SAGE WOPS HIV studies (https://www.who.int/healthinfo/sage/hiv_studies/en/) provide details of the studies and links to the data archive for all waves and materials, which are in the public domain and available free of charge. Prospective users of the study instruments, protocols and meta- and micro-data will need to agree to the online user agreement before access is granted.
Declaration. None.
Acknowledgements. We thank all the study respondents in both sites. We acknowledge the work done by the various team members. We appreciate the leadership from the principal investigators in both Uganda and SA over the years. We have received tremendous support from MRC/UVRI and LSHTM Uganda Research Unit, AHRI and WHO-SAGE since the initiation of this cohort. Statisticians, research data managers and laboratory staff who have worked with the teams over the past decade are also gratefully acknowledged.
Author contributions. JS conceptualised the manuscript. JM and AE drafted the manuscript. All authors reviewed and edited the final manuscript.
Funding. Financial support was provided by National Institutes of Ageing through the WHO SAGE.
Conflicts of interest. None.
References
1. Bakanda C, Birungi J, Mwesigwa R, et al. Association of aging and survival in a large HIV-infected cohort on antiretroviral therapy. AIDS 201135(5):701-705. https://doi.org/10.1097/QAD.0b013e3283437ed7 [ Links ]
2. Semeere AS, Lwanga I, Sempa J, et al. Mortality and immunological recovery among older adults on antiretroviral therapy at a large urban HIV clinic in Kampala, Uganda. J Acquired Immune Defic Synd 2014;67(4):382. https://doi.org/10.1097/qai.0000000000000330 [ Links ]
3. Perez JL, Moore RD. Greater effect of highly active antiretroviral therapy on survival in people aged >50 years compared with younger people in an urban observational cohort. Clin Infect Dis 2003;36(2):212-218. https://doi.org/10.1086/345669 [ Links ]
4. Tavoschi L, Dias JG, Pharris A, et al. New HIV diagnoses among adults aged 50 years or older in 31 European countries, 2004 - 15: An analysis of surveillance data. Lancet HIV 2017;4(11):e514-e521. https://doi.org/10.1016/S2352-3018(17)30155-8 [ Links ]
5. Autenrieth CA, Beck EJ, Stelzle D, et al. Global and regional trends of people living with HIV aged 50 and over: Estimates and projections for 2000 - 2020. PLOS One 2018;13(11):e0207005. https://doi.org/10.1371/journal.pone.0207005 [ Links ]
6. Pillay NK, Maharaj P. Population ageing in Africa. In: Maharaj P (ed.) Aging and Health in Africa. New York: Springer, 2013:11-51. [ Links ]
7. Kalasa B. Population and Ageing in Africa: A policy dilemma. Addis Ababa: UNFPA, 2001. [ Links ]
8. Lloyd-Sherlock P. Population ageing in developed and developing regions: Implications for health policy. Soc Sci Med 2000;51(6):887-895. https://doi.org/10.1016/S0277-9536(00)00068-X [ Links ]
9. Mba CJ. Population ageing and survival challenges in rural Ghana. J Soc Dev Afr 2004;19(2):90-112. https://doi.org/10.4314/jsda.v19i2.23889 [ Links ]
10. Negin J, Cumming RG. HIV infection in older adults in sub-Saharan Africa: Extrapolating prevalence from existing data. Bull World Health Org 2010;88(11):847-853. https://doi.org/10.2471/blt.10.076349 [ Links ]
11. Negin J, Martiniuk A, Cumming RG, et al. Prevalence of HIV and chronic comorbidities among older adults. AIDS 2012;26(01):S55. https://doi.org/10.1097/QAD.0b013e3283558459 [ Links ]
12. Gómez-Olivé FX, Angotti N, Houle B, et al. Prevalence of HIV among those 15 and older in rural South Africa. AIDS Care 2013;25(9):1122-1128. https://doi.org/10.1080/09540121.2012.750710 [ Links ]
13. Kowal P, Chatterji S, Naidoo N, et al. Data resource profile: The World Health Organization Study on global AGEing and adult health (SAGE). Int J Epidem 2012;41(6):1639-1649. https://doi.org/10.1093/ije/dys210 [ Links ]
14. Kowal P, Dowd JE. Definition of an older person. Proposed working definition of an older person in Africa for the MDS Project. Geneva: World Health Organisation, 2001. https://doi.org/10.1314012.1.5188.9286 [ Links ]
15. Asiki G, Murphy G, Nakiyingi-Miiro J, et al. The general population cohort in rural south-western Uganda: A platform for communicable and non-communicable disease studies. Int J Epidem 2013;42(1):129-141. https://doi.org/10.1093/ije/dys234 [ Links ]
16. Terris-Prestholt F, Kumaranayake L, Foster S, et al. The role of community acceptance over time for costs of HIV and STI prevention interventions: Analysis of the Masaka Intervention Trial, Uganda, 1996 -1999. Sexually Trans Dis 2006;33(10):S111-S116. https://doi.org/10.1097/01.olq.0000175389.10289.ba [ Links ]
17. French N, Gray K, Watera C, et al. Cryptococcal infection in a cohort of HIV-1-infected Ugandan adults. AIDS 2002;16(7):1031-1038. [ Links ]
18. Knodel J, Im-em W. The economic consequences for parents oflosing an adult child to AIDS: Evidence from Thailand. Soc Sci Med 2004;59(5):987-1001. https://doi.org/10.1016/j.socscimed.2003.11.042 [ Links ]
19. Seeley J, Wolff B, Kabunga E, et al. 'This is where we buried our sons': People of advanced old age coping with the impact of the AIDS epidemic in a resource-poor setting in rural Uganda. Ageing Soc 2009;29(1):115-134. https://doi.org/10.1017/S0144686X08007605 [ Links ]
20. Nyirenda M, Chatterji S, Falkingham J, et al. An investigation of factors associated with the health and well-being of HIV-infected or HIV-affected older people in rural South Africa. BMC Pub Health 2012;12(1):259. https://doi.org/10.1186/1471-2458-12-259 [ Links ]
21. Kowa P, Kahn K, Ng N, et al. Ageing and adult health status in eight lower-income countries: The INDEPTH WHO-SAGE collaboration. Glob Health Action 2010;3(1):5302. https://doi.org/10.3402/gha.v3i0.5302 [ Links ]
22. Edwards A, Siedner MJ, Nash S, Neuman M, Danaviah S, Smit T, Gareta D, Kowal P, Seeley J. HIVserostatus, inflammatory biomarkers and the frailty phenotype among older people in rural KwaZulu-Natal, South Africa, African Journal of AIDS Research 2020;19(3):177-185. https://doi.org/10.2989/16085906.2020.1790398 [ Links ]
23. Soleman N, Chandramohan D, Shibuya K. Verbal autopsy: Current practices and challenges. Bull World Health Org 2006;84:239-245. [ Links ]
24. Lopman BA, Barnabas RV, Boerma JT, et al. Creating and validating an algorithm to measure AIDS mortality in the adult population using verbal autopsy. PLoS Med 2006;3(8):e312. https://doi.org/10.1371/journal.pmed.0030312 [ Links ]
25. World Health Organization. Verbal autopsy standards: Ascertaining and attributing cause of death. Geneva: WHO, 2007. [ Links ]
 Correspondence:
Correspondence:
A Edwards
anita.edwards@ahri.org
Accepted 13 April 2023














