Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 no.9 Pretoria Set. 2023
http://dx.doi.org/10.7196/samj.2023.v113i9.836
RESEARCH
Further evidence of misclassification of injury deaths in South Africa: When will the barriers to accurate injury death statistics be removed?
P GroenewaldI; N KallisII; C HolmgrenIII; T GlassIV; A AnthonyV; P MaudVI; Y AkhalwayaVII; E AfonsoVIII; I NiewoudtIX; L J MartinX, XI; C de VaalXII; M CheyipXIII; D MorofXIV; M PrinslooXV, XVI, XVII; R MatzopoulosXVIII, XIX; D BradshawXX
IMB ChB, MPH; Burden of Disease Research Unit, South African Medical Research Council, Cape Town, South Africa
IIMB ChB; Burden of Disease Research Unit, South African Medical Research Council, Cape Town, South Africa
IIIMB ChB; Burden of Disease Research Unit, South African Medical Research Council, Cape Town, South Africa
IVBComm Hons, MPH; Burden of Disease Research Unit, South African Medical Research Council, Cape Town, South Africa
VMB ChB, MPH; Department of Health and Wellness, Western Cape Department of Health, Cape Town, South Africa
VIMB ChB; Burden of Disease Research Unit, South African Medical Research Council, Cape Town, South Africa
VIIMB ChB; Family Centre for Research with Ubuntu (FAM-CRU), Department of Paediatrics, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
VIIIMMed (For Med), FC For Path (SA); Division of Forensic Medicine, Department of Pathology, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IXMB ChB; Division of Forensic Medicine, Department of Pathology, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
XMB ChB, MMed (For Med), FC For Path (SA); Division of Forensic Medicine, Department of Pathology, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
XIMB ChB, MMed (For Med), FC For Path (SA); Forensic Pathology Service, Western Cape Department of Health, Cape Town, South Africa
XIIMB ChB; Division of Forensic Medicine, Department of Pathology, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
XIIIMSc; US Centers for Disease Control and Prevention, Pretoria, South Africa
XIVMD, MSc; US Centers for Disease Control and Prevention, Pretoria, South Africa
XVMPH, PhD; Burden of Disease Research Unit, South African Medical Research Council, Cape Town, South Africa
XVIMPH, PhD; Institute for Lifecourse Development, Faculty of Education, Health and Human Sciences, University of Greenwich, London, UK
XVIIMPH, PhD; School of Public Health and Family Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
XVIIIMPhil, PhD; Burden of Disease Research Unit, South African Medical Research Council, Cape Town, South Africa
XIXMPhil, PhD; School of Public Health and Family Medicine, Faculty of Health Sciences, University of Cape Town, South Africa
XXDPhil; Burden of Disease Research Unit, South African Medical Research Council, Cape Town, South Africa
ABSTRACT
BACKGROUND: Contrary to the World Health Organization's internationally recommended medical certificate of cause of death, the South African (SA) death notification form (DNF) does not allow for the reporting of the manner of death to permit accurate coding of external causes of injury deaths
OBJECTIVES: To describe the injury cause-of-death profile from forensic pathology records collected for the National Cause-of-Death Validation (NCoDV) Project and compare it with profiles from other sources of injury mortality data. In particular, the recording of firearm use in homicides is compared between sources
METHODS: The NCoDV Project was a cross-sectional study of deaths that occurred during a fixed period in 2017 and 2018, from a nationally representative sample of 27 health subdistricts in SA. Trained fieldworkers scanned forensic records for all deaths investigated at the forensic mortuaries serving the sampled subdistricts during the study period. Forensic practitioners reviewed the records and completed a medical certificate of cause of death for each decedent. Causes of death were coded to the International Statistical Classification of Diseases, 10th revision (ICD-10), using Iris automated coding software. Cause-specific mortality fractions for injury deaths were compared with Injury Mortality Survey 2017 (IMS 2017) and Statistics South Africa 2017 (Stats SA 2017) datasets. The cause profile for all firearm-related deaths was compared between the three datasets
RESULTS: A total of 5 315 records were available for analysis. Males accounted for 77.6% of cases, and most decedents were aged between 25 and 44 years. Homicide was the leading cause of death (34.7%), followed by transport injuries (32.6%) and suicide (14.7%). This injury cause profile was similar to IMS 2017 but differed markedly from the official statistics, which showed markedly lower proportions of these three causes (15.0%, 11.6% and 0.7%, respectively), and a much higher proportion of other unintentional causes. Investigation of firearm-related deaths revealed that most were homicides in NCoDV 2017/18 (88.5%) and IMS 2017 (93.1%), while in the Stats SA 2017 data, 98.7% of firearm deaths were classified as accidental. Approximately 7% of firearm-related deaths were suicides in NCoDV 2017/18 and IMS 2017, with only 0.3% in Stats SA 2017
CONCLUSION: The official cause-of-death data for injuries in SA in 2017 differed substantially from findings from the NCoDV 2017/18 study and IMS 2017. Accurate data sources would ensure that public health interventions are designed to reduce the high injury burden. Inclusion of the manner of death on the DNF, as is recommended internationally, is critically important to enable more accurate, reliable and valid reporting of the injury profile
Although South Africa (SA) has a high burden of injury mortality, official mortality statistics in SA do not necessarily provide an accurate profile of the causes of injury deaths.[1] In order to code an injury cause accurately, the manner of death and intent of the injury are essential.[2] Intentional injuries include homicide and suicide, and unintentional injuries include any inadvertent causes. When the intent is not reported for a firearm injury, International Statistical Classification of Diseases, 10th revision (ICD-10) coding guidelines[2] specify that these injuries are coded as unintentional. While this may be a reasonable assumption for countries where unintentional injuries predominate, it is not necessarily appropriate for countries with high levels of violence.[3] Alignment to the international ICD-10 guidelines was not possible, as SA legislation does not allow for reporting the manner of death on the medical certificate of cause of death.[4] As a result, official injury mortality statistics are likely to over-estimate accidental injuries and under-estimate homicide and suicide,[1,3] limiting public health planning and monitoring of interventions for injury prevention in a country known to have an extremely high burden of injuries.[5]
Two national Injury Mortality Surveys (IMSs) were conducted in 2009 and 2017[6,7] to establish more accurate injury cause profiles in SA, with a third survey report underway for the period April 2020 - March 2021. Using trained fieldworkers to abstract data from forensic records from a nationally representative sample of mortuaries, these sample surveys have highlighted the large discrepancies between the injury mortality cause profile based on the probable manner of death from forensic records, and the official statistics.
The South African Medical Research Council (SAMRC) National Cause-of-Death Validation (NCoDV) Project set out to validate causes of death reported on official death notification forms (DNFs) against causes of death assigned from medical, forensic and verbal autopsy (VA) records in order to estimate correction factors for cause-specific mortality fractions.[8] Records from a sample of facilities were copied and reviewed by forensic pathologists to identify the cause of death, providing an opportunity to compare and validate the injury mortality profile based on vital statistics using a different method. The purpose of this article is to describe the injury cause profile from the NCoDV study and compare it with profiles from other sources of injury mortality data. Further comparison among the data sources includes the recording of firearm use in homicides.
Methods
Study design
The NCoDV Project was a cross-sectional study using data collected for deaths that occurred during a fixed period in 2017 and 2018 from a nationally representative sample of health subdistricts in SA. The full details of the study design and methodology can be found in the first report of the NCoDV study.[8]
Sampling
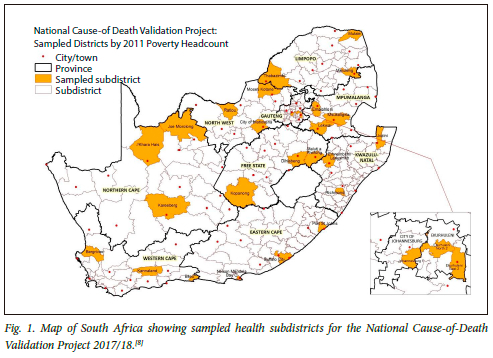
A nationally representative random sample of 27 subdistricts (Fig. 1) was selected using pseudostratification according to socioeconomic status based on the poverty headcount in each province. The poverty headcount for each subdistrict in the province was ranked and divided into tertiles. One subdistrict was randomly selected from each tertile to ensure provincial representation of all socioeconomic strata. The sample plan as per protocol was to collect medical and forensic pathology records for the decedents for whom the next of kin had consented to a VA interview on the events leading to their relative's death. However, given challenges experienced with the recruitment of next of kin for the VA interviews, the protocol was amended to increase the sample size to include all decedents (even those without a VA) who died in a health facility or were referred to Forensic Pathology Services (FPS) serving the 27 sampled subdistricts. After permission from the relevant facilities had been obtained, the data for public hospital deaths and deaths referred to FPS mortuaries during the period September 2017 - April 2018 were included in the sample. All unnatural deaths are referred to FPS for a forensic investigation. These include deaths caused by physical or chemical influences on the body, sudden unexpected deaths, procedure-related deaths, and any deaths that may have been due to omission or commission.
Data collection and processing
FPS case records for deaths that occurred during the study period were collected from the forensic mortuaries serving the sampled health districts.
Trained fieldworkers captured personal identifiers from the forensic records into a form (checklist) set up in KoboToolbox V1.23.3k (Harvard Humanitarian Initiative, USA)[9] using the KoboCollect application on android tablets. This checklist was set up to capture identification details (name, surname, national identity (ID) number, date of birth and date of death) against a unique study identity number for decedents identified as eligible for inclusion in the study.
To ensure confidentiality, pages from the records were anonymised and labelled with the assigned unique study identification number. All records relating to the scene of the injury, postmortem results and any laboratory test results were scanned using Clear Scanner 2018 (Indy Mobile App Co. Ltd, Thailand).[10] The collected images were stored on the access-controlled device and uploaded daily to the secure access-controlled Dropbox Business 2018 (Dropbox, USA)[11] folder. Quality assurance of the data collected was conducted daily, with a review of the forensic pathology files, ensuring that records were correctly deidentified and numbered.
Forensic record reviews were conducted by 10 forensic pathologists after they had received training in the medical certification of cause of death, the review of forensic records and the data collection tool. The forensic record review form was also set up using KoboToolbox and captured using the KoboCollect app on android tablets. The reviewer captured a short summary of the case, information on HIV and tuberculosis status, the manner of death and the sequence of causes leading to death, using the format of the international medical certificate of cause of death.[2] Reviewers also rated the quality of the forensic records and level of certainty for the underlying cause of death for each record based on how the diagnosis for each cause reported was confirmed. A small team of quality assurance reviewers reviewed all the forensic records to ensure that the certification of cause of death included the circumstances of the death as well as the manner of death. All records with unknown underlying cause of death were reviewed against the forensic records to ensure that no information had been missed.
The forensic records checklist dataset was checked to verify that the ID numbers were valid, and the data were linked to the Rapid Mortality Surveillance[12] database to confirm that the death had been registered. The data were checked for any inconsistencies and cleaned prior to coding the causes of death. Iris automated software, version 5.6 (Iris Institute, Germany),[13] was used to code the multiple causes of death to 4-digit ICD-10 codes and select the underlying causes of death by applying the ICD coding rules.
The external causes of death were checked manually in Excel version 2305 (Microsoft Corp., USA)[14] to identify the most common terms reported for external causes and the nature of injury. For this study, the Iris dictionary was updated to include these terms. The software assigns a code to each cause listed in the medical certificate of cause of death and then selects an underlying cause according to ICD-10 coding guidelines. Where the software is unable to assign a cause of death, the record is rejected. During the initial batch processing of these records, ~38% were rejected. These rejected records were divided into three lots and manually coded by researchers with coding training. Additional terms were added to the dictionary where required. The final codes were checked against the manner of death selected in the FPS record review.
Data analysis
The FPS data were checked and cleaned, and duplicate records, identified using the unique 13-digit SA ID number, were removed from the database. The cleaned data were put through ANACONDA[15] (Analysis of Causes of National Deaths for Action), an electronic tool for assessing the quality of information of cause-of-death data by checking for potential errors and inconsistencies, to assess the quality of the causes of death recorded on the FPS records. The underlying causes were subsequently aggregated to the following disease lists for analysis: ICD-10 chapters (21 cause groups);[2] the World Health Organization (WHO) 2016 cause-of-death list for VA (64 causes);[16] and the SA National Burden of Disease categories (144 causes).[17] Basic descriptive statistics of the FPS records, including the distribution of age and sex and the analysis of causes of death, was performed using Stata Statistical Software, release 16 (StataCorp, USA).[18] Cause-specific mortality fractions were calculated for the National Burden of Disease causes. Using the criteria developed by an expert group convened by the Bloomberg Philanthropies Data for Health Initiative and the Civil Registration and Vital Statistics Improvement project of the University of Melbourne in 2017,[15] the quality of the underlying cause information for the deaths with specified sex and age was evaluated. Cause-specific mortality fractions for injury deaths reported by NCoDV 2017/18,[8] IMS 2017[7] and Statistics South Africa 2017 (Stats SA 2017) [19] were compared. In addition, the cause profile for all firearm-related deaths was compared between the three datasets.
Ethical considerations
The project protocol was reviewed by the SAMRC ethics committee and approved on 27 June 2017 (ref. no. EC004-2/2017).
The project was reviewed in accordance with Centers for Disease Control and Prevention (CDC) human research protection procedures and was determined to be research, but CDC investigators did not interact with human subjects or have access to identifiable data or specimens for research purposes.
Permission to access information on decedents from medical and forensic records at public hospitals and FPS facilities was obtained from the national, provincial and district health departments as well as individual facilities. Despite provincial permission, the KwaZulu-Natal (KZN) FPS denied access to forensic mortuary records.
Results
A total of 5 752 FPS case records for deaths occurring between 1 September 2017 and 30 April 2018 were collected during fieldwork. Of the 5 752 case records, 148 images of the record were lost during syncing, 122 were duplicate records and 22 only had medical records available for review, leaving 5 460 for analysis. A further 145 cases were excluded because no information on the cause of death was available in the folder, or the case was reported to be a non-viable fetus or a stillbirth.
A total of 5 315 records were therefore available for analysis from 8 of the 9 provinces of SA (KZN FPS was excluded, see above). Gender was missing or ambiguous in 6 cases, and age was missing in 62 cases. Males accounted for 77.6% of the FPS cases (n=4 123/5 309). The highest proportion of cases (45.3%) were between 25 and 44 years of age (Table 1).
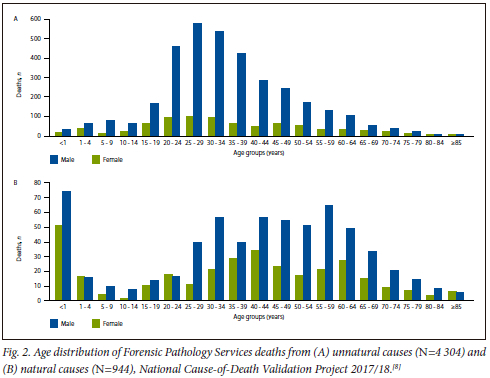
The majority (81.9%) of the FPS deaths were due to unnatural causes (n=4 355/5 315), with a significantly higher proportion of unnatural causes in males (n=3 490/4 123; 84.6%) than in females (n=862/1 186; 73.4%) (Pearson's x2(1)=89.2473; p<0.001). Males accounted for 80.2% of the unnatural deaths (n=3 490/4 352). The age distribution of unnatural deaths shows a concentration in young adults, with a peak at 25 - 29 years of age for both sexes (Fig. 2). There were high numbers of natural deaths in those aged <1 year and a distribution across older ages.
In 86% of cases, the forensic pathologist reviewers scored the quality and coherence of the forensic records (admission notes, case history and autopsy records and findings) as adequate to excellent. In the records with low scores, the major concern was poor documentation of the details of the autopsies. Another issue identified was that toxicology results were rarely available at the time of reviewing (±2 years after death).
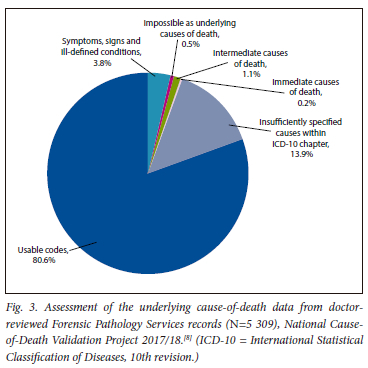
The underlying cause-of-death information was found to be of good quality. A high proportion of the causes (n=4 281/5 309; 80.6%) were coded to usable codes (codes for valid underlying causes of death), with 19.4% classified as unusable, mainly due to insufficiently specified causes within an ICD chapter (13.9%), followed by symptoms, signs and ill-defined conditions (3.8%) (Fig. 3).
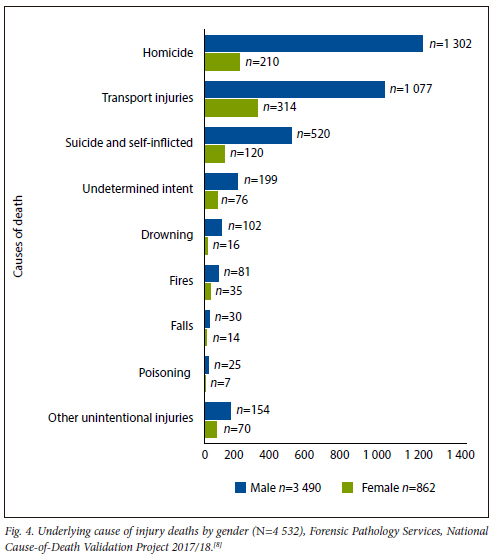
Homicide was the leading cause of death, accounting for 34.7% of injury deaths. This was followed by transport injuries (32.6%) and then suicide (14.7%). The balance of the unintentional deaths (drowning, fires, falls, poisoning and other unintentional) accounted for 11.6%, and 6.3% were of undetermined intent (Fig. 4). For injuries overall, the male-to-female ratio was 4. For homicide this increased to 6. The ranking of injury causes of death differed by gender, with homicide the leading cause in males and transport injuries the leading cause in females (Fig. 4).
A comparison of the injury cause-specific mortality fractions (CSMFs) between the NCoDV 2017/18, IMS 2017 and official DNF data (Stats SA 2017)shows that the NCoDV cause profile is very similar to the IMS profile, except for slightly higher transport injuries in the NCoDV data. The CSMFs from the official mortality data reported on the DNF are completely different, with the CSMFs for homicide, transport and suicide much lower than in IMS 2017 and NCoDV 2017/18, and that for unintentional injuries much higher (Fig. 5).
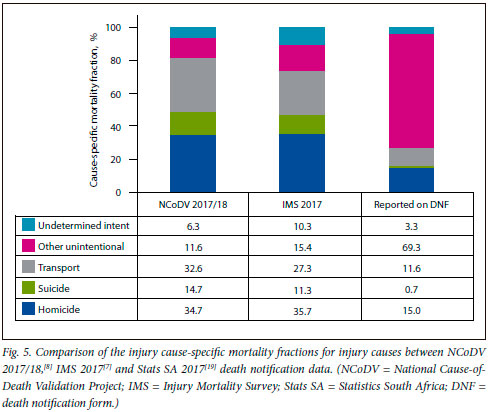
Closer investigation of firearm-related deaths (Table 2) revealed that the majority of these deaths were due to homicide in NCoDV 2017/18 (88.5%) and IMS 2017 (93.1%), while in the Stats SA 2017 data, 98.7% of firearm deaths were classified as accidental and only 1% as homicide. Approximately 7% of firearm-related deaths were classified as due to suicide in NCoDV 2017/18 and IMS 2017, with only 0.3% in Stats SA 2017.
Discussion
This study demonstrates that the information necessary to provide an accurate injury cause profile is available, but it is not currently being reported through the routine Civil Registration and Vital Statistics (CRVS) system. The fact that insufficient information is reported on the death notification form for accurate coding of cause of death may be attributed to the Inquests Act 58 of 1959,[4] which has been interpreted by some forensic pathologists as prohibiting the reporting of the manner of death on the DNF (homicide, suicide, unintentional, disease). However, the perceived prohibition does not align with the systems in place, as the autopsy report provides the courts with the anatomical cause of death to assist the courts to determine manner of death and possible accountability, whereas the DNF provides mortality data for public health planning and monitoring. This information is essential for completion of the WHO international medical certificate of cause of death to code the most specific cause. If this detailed information was reported through the CRVS system, more comprehensive injury mortality could be captured using a simpler and less costly system.
Given that the causes of death for NCoDV 2017/18 were assigned by a forensic pathologist after a record review, while the IMS 2017 causes were extracted from the forensic records by trained fieldworkers, and the injury cause profiles are very similar,[6] the cause profiles for the data extracted by the IMS 2017 fieldworkers appear to be validated. The slightly increased proportion of transport injury deaths in the NCoDV data is likely to be because the study periods are not entirely consistent, with the NCoDV study duration being shorter but covering both the Christmas and Easter periods when transport injuries are more frequent.
The NCoDV and IMS studies both provide more detailed and consistent injury cause profiles compared with data reported on the DNF, and provide more accurate information useful for public health planning or monitoring. Given the very high injury burden in SA, it is essential that the cause profile is monitored closely to enable decisions on appropriate interventions and to monitor the impact of these interventions. While the NCoDV method is likely to provide more accurate information than IMS 2017, given that forensic pathologists review the records, this is a very costly and time-consuming process and not feasible for routine surveillance.
In addition, the review of actual forensic records from all over the country suggests that the national code of guidelines for forensic pathology practice in SA as set out in the Regulations Regarding the Rendering of Forensic Pathology Service[20] is not consistently implemented or monitored, and the development of quality assurance and audit tools for assessing these regulations could improve the system. Plans are also warranted to address the backlog in toxicology screening. Toxicology results do take time, and death registration and burials cannot be delayed, so the implementation of a system for amending the cause of death once toxicology results are received would improve data quality. This is already being done at certain large facilities. In 2014, the National Forensic Pathology Services Committee was established by the Minister of Health to advise the Minister on matters pertaining to Forensic Pathology Services, and could be responding to the issues mentioned above. However, the committee has not been active since 2018/19 and could be reconvened as a matter of urgency.
More recently, the COVID-19 pandemic has raised global concern about the potential impact on mental health and suicide, particularly in middle-income countries (MICs) and low- and middle-income countries (LMICs), where the suicide burden is highest. A recent systematic review of suicide in MICs and LMICs shows no evidence of an increase in suicide during the early stages of the pandemic,[21] but there are very few data looking at the impact in later stages. This review highlighted the opportunity for ongoing real-time surveillance to monitor the impact of the pandemic on suicide in these countries. Notably, there was no evidence at all from Africa. In SA, alcohol bans during lockdowns reduced deaths due to non-natural causes dramatically, and it could be important to investigate their impact on individual external causes. However, this is not possible because, although information on suicide and other external causes is available, these data have not yet been incorporated into our official mortality statistics. This contribution could have a considerable impact on the measurement and understanding of injury and mental health conditions.[1,22]
Study limitations
We found that poor documentation of autopsy reports in 14% of cases impeded the assessment of cause of death for the NCoDV study; however, this would not necessarily have been the case for the certified cause of death reported to Stats SA, as the forensic pathologist who performed the autopsy would certify the death. Despite this limitation, given the magnitude of the difference in the injury mortality cause profiles between the NCoDV study and the Stats SA data, it is unlikely that the poor documentation of autopsy reports in 14% would have changed the overall findings. The agreement between the NCoDV and Stats SA causes of death could be measured more accurately through linking of records from these two datasets. This could also be done for the NCoDV and IMS datasets, which could clarify the slight differences in the transport fatalities.
Conclusion
The official cause-of-death data for injuries in SA do not optimally reflect the burden and types of injuries faced by the population. Based on this study, interventions that lead to improved specificity and efficient capture of injury deaths may be warranted to improve accuracy and timeliness. The development of an integrated health information system that provides local, provincial and national health departments with accurate, reliable and timeous health data required to perform their functions is critical, but would take time. However, inclusion of the manner of death on the DNF would enable more accurate, reliable and valid reporting of the injury profile. Accurate reporting directly influences fiscal allocations. The impact of inaccurate reporting is likely to include insufficient support for mental health services and suicide prevention, law enforcement in vulnerable communities, and interventions to prevent alcohol harm, among others. Ultimately the goal of collecting cause-of-death information for injuries is to decrease SA's injury burden. This will only be possible once the cause-of-death data are accurate and fit for purpose.
Declaration. None.
Acknowledgements. We acknowledge the contribution of Francois Bezuidenhout and his field workers from Geospace for data collection, the late Prof. Johan Dempers, head of the Division of Forensic Medicine, Department of Pathology, Faculty of Medicine and Health Sciences, Stellenbosch University, and his colleagues Dr Bjorn Swigelaar and Dr Janette Verster, for their valuable contributions to and support of the study, and Dr Jané Joubert, SAMRC, for her critical review of the manuscript.
Author contributions. PG, DB and RM conceptualised the article. EA, IN, CdV and YA reviewed the forensic records. NK, CH, AA and PM were responsible for quality assurance and the initial draft. TG conducted the statistical analysis. LJM, MC and DM provided technical assistance. MP provided technical expertise and training for data collection, provided data from the IMS and assisted with the analysis. All authors were involved in the writing and review of the manuscript.
Funding. This publication was supported by the President's Emergency Plan for AIDS Relief (PEPFAR) through the CDC under the terms of GH002193. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the funding agency.
Conflicts of interest. None.
References
1. Prinsloo M, Bradshaw D, Joubert J, Matzopoulos R, Groenewald P. South Africa's vital statistics are currently not suitable for monitoring progress towards injury and violence Sustainable Development Goals. S Afr Med J 2017;107(6):470-471. https://doi.org/10.7196/SAMJ.2017.v107i6.12464 [ Links ]
2. World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th revision, version for 2016. Geneva: WHO, 2016. http://apps.who.int/classifications/icd10/browse/2016/en (accessed 6 March 2023). [ Links ]
3. Matzopoulos R, Groenewald P, Abrahams N, Bradshaw D. Where have all the gun deaths gone? S Afr Med J 2016;106(6):589-591. https://doi.org/10.7196/SAMJ.2016.v106i6.10379 [ Links ]
4. South Africa. Inquests Act 58 of 1959. https://www.gov.za/documents/inquests-act-3-jul-1959-0000 (accessed 6 March 2023). [ Links ]
5. Norman R, Matzopoulos R, Groenewald P, Bradshaw D. The high burden of injuries in South Africa. Bull World Health Organ 2007;85(9):695-702. https://doi.org/10.2471/blt.06.037184 [ Links ]
6. Matzopoulos R, Prinsloo M, Bradshaw D, et al. The Injury Mortality Survey: A national study of injury mortality levels and causes in South Africa in 2009. Cape Town: South African Medical Research Council, 2013. https://www.samrc.ac.za/sites/default/files/attachments/2022-08/InjuryMortalitySurvey.pdf (accessed 9 August 2023). [ Links ]
7. Prinsloo M, Mhlongo S, Dekel B, et al. The 2nd Injury Mortality Survey: A national study of injury mortality levels and causes in South Africa in 2017. Cape Town: South African Medical Research Council, 2021. https://www.samrc.ac.za/sites/default/files/attachments/2022-08/The%202nd%20Injury%20Mortality%20Survey%20Report_FinaLpdf (accessed 9 August 2023). [ Links ]
8. Bradshaw D, Joubert JD, Maqungo M, et al. South African National Cause-of-Death Validation Project: Methodology and description of a national sample of verbal autopsies. Cape Town: South African Medical Research Council, 2020. https://www.samrc.ac.za/research-reports/south-african-national-cause-death-validation (accessed 9 August 2023). [ Links ]
9. Harvard Humanitarian Initiative. KoboToolbox: Data collection tools for challenging environments. http://www.kobotoolbox.org/ (accessed 6 March 2023). [ Links ]
10. Clear Scanner. https://dear-scanner-free-pdf-scans.en.soitonic.com/android (accessed 11 December 2019). [ Links ]
11. Dropbox Business. https://www.dropbox.com/business (accessed 11 December 2019). [ Links ]
12. Dorrington RE, Bradshaw D, Laubscher R, Nannan N. Rapid Mortality Surveillance report 2019 & 2020. Cape Town: South African Medical Research Council, 2021. https://www.samrc.ac.za/sites/default/files/attachments/2022-08/Rapid%20Mortaliy%20Surveillance%20Report%202019%262020.pdf (accessed 6 March 2023). [ Links ]
13. Iris Institute. Iris - Automated coding system for causes of death. Heidelberg, Germany: German Institute of Medical Documentation and Information (DIMDI), 2018. [ Links ]
14. Microsoft Corporation. Microsoft Excel. 2018. https://office.microsoft.com/excel (accessed 6 March 2023). [ Links ]
15. Mikkelsen L, Moesgaard K, Hegnauer M, Lopez AD. ANACONDA: A new tool to improve mortality and cause of death data. BMC Med 2020;18:61. https://doi.org/10.1186/s12916-020-01521-0 [ Links ]
16. World Health Organization. Verbal autopsy standards: The 2016 WHO verbal autopsy instrument. Geneva: WHO, 2016. https://www.who.int/publications/m/item/verbal-autopsy-standards-the-2016-who-verbal-autopsy-instrument (accessed 10 August 2023). [ Links ]
17. Pillay-van Wyk V, Laubscher R, Msemburi W, et al. Second South African National Burden of Disease Study: Data cleaning, validation and SANBD list. Cape Town: South African Medical Research Council, 2014. https://www.samrc.ac.za/sites/default/files/attachments/2022-08/SANBDReport.pdf (accessed 10 August 2023). [ Links ]
18. StataCorp. Stata Statistical Software: Release 16. College Station, Texas: StataCorp, 2019. [ Links ]
19. Statistics South Africa. Mortality and causes of death in South Africa, 2017: Findings from death notification. Pretoria: Stats SA, 26 March 2020. https://www.statssa.gov.za/publications/P03093/P030932017.pdf (accessed 10 August 2023). [ Links ]
20. South Africa. National Health Act, 2003 (Act No. 61 of 2003). Regulations regarding the rendering of Forensic Pathology Service. Government Gazette No. 41524, 23 March 2018. https://www.gov.za/sites/default/files/gcis_document/201803/41524rg10811gon359s.pdf (accessed 10 August 2023). [ Links ]
21. Knipe D, John A, Padmanathan P, et al. Suicide and self-harm in low- and middle-income countries during the COVID-19 pandemic: A systematic review. PLoS Glob Public Health 2022;2(6):e0000282. https://doi.org/10.1371/journal.pgph.0000282 [ Links ]
22. Groenewald P, Azvedo V, Daniels J, Evans J, Naledi T, Bradshaw D. The importance of identified cause-of-death information being available for public health surveillance, actions and research. S Afr Med J 2015;105(7):528-530. https://doi.org/10.7196/SAMJnew.8019 [ Links ]
 Correspondence:
Correspondence:
P Groenewald
pamela.groenewald@mrc.ac.za
Accepted 12 June 2023














