Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 n.7 Pretoria Jul. 2023
http://dx.doi.org/10.7196/SAMJ.2023.v113i7.291
RESEARCH
Private healthcare sector spine surgery: Patient and surgeon profiles from a large open medical scheme in South Africa
T N MannI, II; A J VlokIII; R N DunnIV; S MiseerV; J H DavisVI, VII
IMPhil, PhD; Institute of Orthopaedics and Rheumatology, Mediclinic Winelands Orthopaedic Hospital, Stellenbosch, South Africa
IIMPhil, PhD; Division of Orthopaedic Surgery, Department of Surgical Sciences, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IIIMMed (Neurosurgery), PhD; Division of Neurosurgery, Department of Surgical Sciences, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IVMMed (Ortho), FC Orth (SA); Division of Orthopaedic Surgery, Faculty of Medicine and Health Sciences, University of Cape Town and Groote Schuur Hospital, Cape Town, South Africa
VMMed (Ortho), FC Orth (SA); Division of Orthopaedic Surgery, Department of Surgical Sciences, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
VIMMed (Ortho), FC Orth (SA); Institute of Orthopaedics and Rheumatology, Mediclinic Winelands Orthopaedic Hospital, Stellenbosch, South Africa
VIIMMed (Ortho), FC Orth (SA); Division of Orthopaedic Surgery, Department of Surgical Sciences, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
ABSTRACT
BACKGROUND: It is generally understood that the profile of spine surgery varies by setting, based on factors such as the age profile of the population, the economic context and access to healthcare. Relatively little is known about the profile of spine surgery in South Africa (SA), although one previous report from the public healthcare sector suggested a high burden of trauma and infection-related surgery. To our knowledge, there has been no formal investigation in the private sector. A holistic understanding of spine surgery within our setting may be beneficial for applications such as resource allocation and informing the training needs of future specialists
OBJECTIVES: To provide insight into spinal surgery in the SA private healthcare sector by describing spine surgery characteristics within a large open medical scheme, including both patient and surgeon profiles
METHODS: This retrospective review included adult inpatient spine surgeries funded by the largest open medical scheme in SA between 2008 and 2017. An anonymised dataset extracted from the scheme records included patient demographics, ICD-10 codes, procedure codes and surgeon specialisation. Descriptive patient and surgery data were presented. Furthermore, the association between patient and surgery factors and surgeon specialisation was investigated using univariate and multivariate analyses
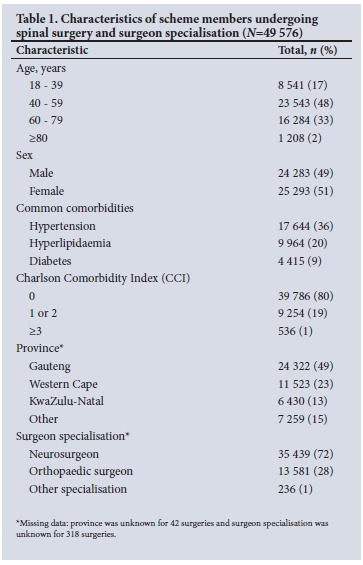
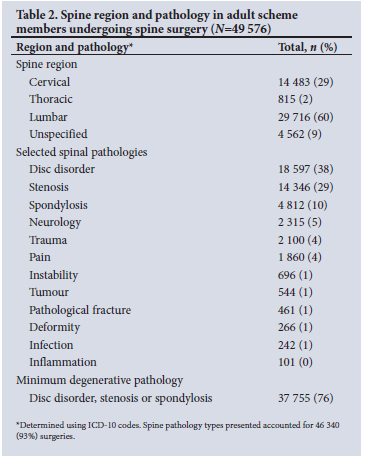
RESULTS: A total of 49 576 index spine surgeries were included. The largest proportion of surgeries involved members aged 40 - 59 years old (n=23 543, 48%), approximately half involved female members (n=25 293, 51%) and most were performed by neurosurgeons (n=35 439, 72%). At least 37 755 (76%) surgeries were for degenerative pathology, 2 100 (4%) for trauma and 242 (0.5%) for infection. Adjusted risk ratios (aRR) significantly associated with orthopaedic surgeon specialisation included cervical spine region (aRR = 0.49; 95% confidence interval (CI) 0.39 - 0.61), trauma (aRR = 1.50; 95% CI 1.20 - 1.88), deformity (aRR = 1.77; 95% CI 1.33 - 2.35) and blood transfusion (aRR = 1.46; 95% CI 1.12 - 1.91
CONCLUSION: Spine surgery in SA's largest open medical scheme was dominated by surgery for degenerative pathology in older adults, and was performed largely by neurosurgeons. This constituted a stark contrast to a previous report from the public sector and highlighted a mismatch between exposure during public sector registrar training and private practice post specialisation. The findings support the need for private-public collaboration as well as the importance of spine fellowships for all specialists intending to practise spine surgery
Spinal pathology may have significant implications for functional ability, work productivity and quality of life, highlighting the need for effective treatment.[1-3] While many spinal disorders improve with conservative management, spinal surgery may provide an equivalent or superior outcome in some cases.[4-6] Relatively few studies have investigated the overall profile of spine surgery in a particular context, with the existing literature focused largely on specific spinal pathologies or procedures.[7-10] However, it is generally understood that the profile of spine surgery varies by setting, based on factors such as the age profile of the population, the economic context, access to healthcare and the relative burden of trauma and infection.[11] In developed countries with good access to healthcare and long life expectancy, the majority of spine surgery would be expected to involve treatment of degenerative pathologies among older adults.[7,8,10-13] Conversely, in developing countries with limited healthcare resources and a lower socioeconomic context, a significant proportion of spine surgeries may involve preventable pathologies, such as trauma and infection, among relatively younger patients.[11,14,15]
In South Africa (SA), previous studies related to spinal surgeries were based in the public sector and tended to focus on specific pathologies;[16,17] to our knowledge, only one study has provided insight into the profile of spinal surgery in our setting.[15] This study described the characteristics of admissions to an orthopaedic spine unit based at a major tertiary hospital in the Western Cape Province, SA, and found that only 52% of admissions underwent spinal surgery, of which 40% were for trauma and 36% for infection.[15] While data from other centres and provinces are lacking, this study suggested that spinal surgery in the public sector is dominated by trauma and infection, notably spinal tuberculosis. Furthermore, it is generally accepted that spinal surgery in the public sector is managed largely by orthopaedic services.
Spinal surgery in the SA private healthcare sector would be expected to differ markedly from that in the public sector, and may more closely resemble the profile of higher-income countries. Spinal surgery has been described as the core business of neurosurgeons who move into private practice after specialisation,[18] therefore the surgeon profile in the private sector would also be expected to differ from that of the public sector. However, there has been little formal investigation of spinal surgery in the private sector, and these perceptions remain unsubstantiated. A holistic understanding of the profile of spinal surgery within the SA setting may be beneficial for applications such as resource allocation, identifying areas for improvement and informing the training needs of future specialists.
Therefore, the aim of this study was to provide insight into spinal surgery in the SA private healthcare sector by describing spinal surgery characteristics within a large open medical scheme, including both patient and surgeon profiles.
Methods
Ethical considerations
The study was approved by the Health Research Ethics Committee of Stellenbosch University (ref. no. N20/11/118) and by the Research Governance Committee of the medical scheme. A waiver of informed consent was granted by the ethics committee due to the use of retrospective, anonymised data.
Design
This retrospective review included inpatient spinal surgeries funded by the largest open medical scheme in SA between 1 January 2008 and 31 December 2017. Characteristics of spinal surgery were investigated based on the member's first spinal surgery within the study period, and did not account for members who had more than one spine procedure. Surgeries included in the analysis were intended to represent index surgeries.
Setting
The SA healthcare sector is comprised of the public health system, which serves ~84% of the population, and the private health system, which serves ~16% of the population. This study was set in the private health sector, which is largely accessed by those with medical scheme membership. The medical scheme that funded the spinal surgeries in the current study had an open market share of 56%, and covered 2 777 946 beneficiaries as of December 2017.[19]
Patients
All members of the medical scheme >18 years of age who underwent inpatient spinal procedures in SA during the study period were identified by the scheme for inclusion in the study. The investigators subsequently reviewed diagnostic and procedure codes for each event, and excluded members from the analysis according to the following criteria: (i) procedure codes indicated medical management only; (ii) the 'index' spine surgery was identified as a revision procedure based on diagnostic and/or procedure codes; or (iii) the diagnostic code was not related to spinal surgery and the procedure codes failed to confirm that a spinal surgery had taken place.
Variables
The spinal surgery data were provided by the medical scheme in the form of an anonymised dataset extracted from the scheme's records. Variables included member demographics, comorbidity ICD-10 codes, surgery ICD-10 code, surgery Complete Current Procedural Terminology for SA (CCSA) codes (procedure codes), surgeon specialisation, year of surgery and geographical region. Geographical region was categorised as Gauteng, Western Cape, KwaZulu-Natal or other provinces (Eastern Cape, North West, Mpumalanga, Free State, Limpopo and Northern Cape), so as to protect the identity of surgeons practising in provinces with a smaller number of spine surgeons. The specialisation of the primary surgeon associated with each spine surgery was also provided by the medical scheme along with a unique, anonymous study code.
Comorbidity ICD-10 codes were analysed for conditions included in the Charlson Comorbidity Index (CCI),[20] and CCI scores were calculated as described elsewhere.[21] The CCI is a weighted index that takes into account the number and severity of comorbid conditions. Each increase in CCI score is associated with an increased risk of death from comorbid disease.[21] The following common comorbidities were also identified by ICD-10 code: hypertension (I10), diabetes (uncomplicated or complicated, as identified for the CCI[20]) and hyperlipidaemia (E78.0 - E78.5).
Surgery ICD-10 code descriptions were analysed, and each surgery was categorised according to pathology type. Pathology categories were named according to the terminology used in the ICD-10 code descriptions as far as possible, e.g. 'M51.0 - lumbar and other intervertebral disc disorders with myelopathy (G99.2*)' was assigned to the category 'disc disorder'.
'Disc disorder', 'stenosis' and 'spondylosis' are pathologies strongly associated with degenerative processes, and these categories were pooled to represent the overall minimum burden of degenerative pathology. Surgery ICD-10 code descriptions were also analysed to identify the spine region involved, and each surgery was categorised accordingly. The spine region was categorised as 'unspecified' when the code description did not mention a region.
CCSA codes are used between hospitals and funders to provide details of the medical procedures performed. A licence to access the description associated with each CCSA code was purchased from the SA Medical Association to enable further analysis of these codes. The following common procedures were identified using CCSA codes and included in the analysis: single-level anterior cervical fusion (CPT22554, CPT63075 and CPT 22551); simple lumbar discectomy (CPT63030, CPT63056, CPT63005, CPT63047 and CPT63020); lumbar fusion with interbody fusion (CPT22630 and CPT22633); and lumbar fusion without interbody fusion (CP22612).
Data analysis
Descriptive categorical data were presented as frequencies and percentages. Crude univariate associations between surgery characteristics and surgeon specialisation (neurosurgeon v. orthopaedic surgeon) were investigated using χ2 tests. Multivariate associations between surgery characteristics and surgeon specialisation were investigated using binomial logistic regression, and correction for clustering was applied owing to the presence of multiple surgeries per surgeon in the dataset. Associations were reported as risk ratios (RR) owing to the relatively high prevalence of the outcome (orthopaedic surgeon specialisation), and were presented with 95% confidence intervals (CIs). Collinearity in multivariate regression models was assessed using variance inflation factor (VIF) and tolerance statistics. Analyses were conducted using jamovi version 1.6 (jamovi, Australia) and Stata Statistical Software version 15 (StataCorp, USA), with significance accepted at p<0.05.
Results
A total of 54 998 adult scheme members underwent inpatient spinal procedures during the study period. However, 200 cases were excluded, as the procedure codes indicated medical management only, 4 686 cases were excluded as the ICD-10 and/or procedure codes indicated a revision or follow-up surgery and 536 codes were excluded based on insufficient evidence of spine surgery from the ICD-10 or procedure codes. The remaining 49 576 were considered index spine surgeries and were included in the analysis.
Patient characteristics and surgeon specialisation
The characteristics of members who underwent spine surgery and the specialisation of the operating surgeon are shown in Table 1. Surgeries took place predominantly among adults between 40 and 59 years of age (n=23 543, 48%), and were evenly distributed between males and females. Although it was common for individuals to have at least one comorbidity, relatively few had serious conditions associated with an increased risk of mortality. Approximately half of all spine surgeries took place in Gauteng (n=24 322, 49%), and the majority of surgeries were performed by neurosurgeons (n=35 439, 72%).
Spine region and pathology
Spine region and pathology type are shown in Table 2, and the 10 most prevalent spinal surgery ICD-10 codes in Table 3. Most spinal pathology occurred in the lumbar region (n=29 716, 60%), followed by the cervical region (n=14 483, n=29%) (Table 2), and degenerative-type pathologies were predominant. The top five ICD-10 codes accounted for 59% of all spine surgeries, and all referred either to a 'disc disorder' or to stenosis as the nature of the problem (Table 3). The median age of those undergoing surgery for degenerative pathology was 54 (interquartile range 44 - 64). Only 4% of spine surgeries were related to trauma (Table 2). Spinal surgeries for deformity, infection and inflammation were the rarest overall, accounting for <1% of all surgeries, respectively (Table 2).
Neurosurgeon v. orthopaedic surgeon
Surgeon specialisation was unknown for 318 surgeries, and a further 236 surgeries had neither a neurosurgeon nor an orthopaedic surgeon associated with the surgery. The remaining 49 022 (98.9%) surgeries were associated with a neurosurgeon or orthopaedic surgeon, and were included in a subanalysis to investigate relationships between surgeon specialisation and surgery characteristics. There were significant univariate associations between surgeon specialisation and several surgery characteristics (Table 4). These crude associations are further illustrated in Fig. 1, which shows variation in the proportion of surgeries performed by each specialisation according to different surgery characteristics. For example, orthopaedic surgeons performed 28% of spine surgeries overall (Table 1) but performed 62% of all surgeries for deformity (Fig. 1).
Univariate associations between orthopaedic surgery specialisation and the baseline factors age, province, spine region and spinal pathology were then investigated using binomial regression, adjusted for clustering by individual surgeons. Province showed no significant association with surgeon specialisation after this adjustment, and only the remaining variables were included in the multivariate model (Table 5). Certain moderate, significant associations with surgeon specialisation remained in the multivariate model: after adjusting for all the factors in the model, cervical spine surgeries were less likely to be done by an orthopaedic surgeon compared with lumbar spine surgeries, and surgeries for disc disorders were less likely to be done by an orthopaedic surgeon compared with surgeries for other pathologies. However, surgeries for trauma or deformity were more likely to be done by an orthopaedic surgeon compared with surgery for other pathologies.
In a second binomial regression model, associations between surgeon specialisation and certain procedures, theatre time and blood transfusions were investigated after adjusting for patient age, pathology and surgeon clustering (Table 5). The model failed to converge with deformity included, and this variable was omitted in the model presented. Once again, small-to-moderate significant associations with surgeon specialisation were observed: after adjusting for all the factors in the model, single-level anterior cervical fusion was less likely to be done by an orthopaedic surgeon compared with other procedures, lumbar fusion without interbody fusion was more likely to be done by an orthopaedic surgeon compared with other procedures and surgeries involving a blood transfusion were more likely to be performed by an orthopaedic surgeon than those not involving a blood transfusion (Table 6).
Discussion
The current study comprised a novel investigation into spine surgery within the SA private healthcare sector. The first finding was that, within the largest open medical scheme, spine surgery was dominated by operations for degenerative pathologies in older adults, with trauma and infection representing only a very small percentage of cases. This pattern is largely in keeping with what would be expected in developed, well-resourced countries with a longer life expectancy. For example, in Japan, a high-income country with a 'super-ageing' population, a multicentre study found that 83% of surgeries were performed for degenerative pathology, 6% for trauma and 2% for infection.[12] There are few other studies from developed countries that evaluate the proportion of spinal surgery related to degenerative pathology in a similar manner. However, pathology or procedure-specific epidemiological studies suggest that surgery for degenerative pathology is very prevalent in such settings.[7,9,13] Conversely, in Nepal, a low- to middle-income country with a predominantly young population, 37% of admissions at a tertiary neurosurgery department were for degenerative pathology, 32% for trauma and 11% for infection.[14]
While the profile of spinal surgery in the medical scheme bore some similarity to that of Japan, it formed a stark contrast to previous findings from the public sector. Degenerative pathology accounted for only 10% of admissions to a tertiary hospital spine unit in the Western Cape Province, and only half of the patients concerned received surgical management.[15] It was also noted that the median age of the patients admitted for degenerative pathology in the public sector was older than those receiving spine surgery for degenerative pathology in the current study, at 59 years v. 54 years of age.[15] Older age is likely indicative of more advanced pathology at the time of surgery, and may reflect limited access to surgical care and longer waiting times in the public healthcare setting. In the public sector, the provision of elective degenerative surgery is inevitably impacted by the burden of trauma and infection, which, collectively, accounted for 75% of tertiary spine unit admissions.[15] In contrast, trauma comprised only 4% of spine surgeries in the current study, and infection <1%, allowing a large capacity for degenerative pathology surgeries. It is well known that multisectoral interventions are urgently needed to ease the burden of preventable pathology in the public sector. However, as an interim measure, a public-private partnership to accommodate patients in need of surgery for degenerative pathology within the private sector would undoubtedly have a large impact on the quality of life for this underserved group.
The second finding of the study was that the large majority of spinal surgeries in the private sector were performed by neurosurgeons, with less than a third performed by orthopaedic spinal surgeons. In contrast, at a tertiary hospital in the Western Cape province, spinal pathology was managed largely by orthopaedic surgeons.[15] More specifically, although uninstrumented spinal procedures form part of the final examinations for neurosurgery registrars, all more complex instrumented/fusion spinal procedures are generally managed by orthopaedic surgeons at the tertiary hospital level. For their part, neurosurgery departments in our setting typically manage a large burden of neurotrauma and other cranial emergencies, such as cranial oncology and vascular pathology. The shift post specialisation may arise from a combination of factors. Firstly, cranial neurosurgery may be insufficient to sustain a private neurosurgeon practitioner. Expansion into spinal surgery provides a sustainable workflow and is covered by the high medical insurance rates for which neurosurgeons are already covered. Secondly, spinal surgery is thought to be a less popular subspecialisation among orthopaedic surgeons in SA, perhaps partly owing to the high medical insurance involved. Uptake of spinal surgery among neurosurgeons, therefore, meets a need that might not otherwise have been addressed solely by orthopaedic surgeons subspecialising in spinal surgery.
Both the first and second findings of the study raise concern about an apparent mismatch between registrar training and practice post specialisation. The majority of spinal surgeries were performed by neurosurgeons who may have had limited spinal training during specialisation. Furthermore, even though orthopaedic surgeons may have had higher exposure to spine surgery during their training, this exposure would have been dominated by trauma and infection rather than the degenerative pathology seen in private practice. It is acknowledged that these are generalisations. The role of orthopaedic surgeons or neurosurgeons in spinal surgery varies by country and by institution and, likewise, the average level of trainee exposure to spinal surgery during specialisation.[14,22] A study from the USA reported considerable variation in trainee spine surgery exposure even within each specialty, and a similar situation may be expected in SA.[22] Irrespective of specialisation, it is widely recognised that spine surgery fellowships are of critical importance for specialists intending to practise in this field; individuals may even complete more than one fellowship if they aim to operate on particularly rare or complex cases.[22,23] Furthermore, such fellowships are of true benefit when they result in effective, well-rounded training rather than simply meeting caseload requirements.[22]
A third finding from the study was associations between surgeon specialisation and certain surgery characteristics. These associations are consistent with the differences in training background between the specialisations: neurosurgeons may have had higher exposure to cervical spine pathology and disc disorders as part of the surgical management of neurological deficit, whereas trauma and deformity surgery fall within the domain of orthopaedics at tertiary level. Neurosurgeons may also have received greater training in minimally invasive techniques, whereas orthopaedic surgeons may perform more invasive surgeries, sometimes requiring blood transfusions. Notably, based on the magnitude of the risk ratios, these are small-to-moderate rather than large associations. Furthermore, it was observed that patient age, province, stenosis or spondylosis pathology, certain common lumbar spine procedures and theatre time showed no significant association with surgeon specialisation in adjusted analyses. This suggests that the clear distinctions in specialty training become much less apparent among practising spine surgeons. This is likely due to completion of the aforementioned spine fellowship training to gain skills not acquired during specialisation.
The current study had several limitations. It was conducted on retrospective data collected for administrative purposes, and the findings are dependent on the accuracy with which this information was captured. Nonspecific code descriptions made it difficult to categorise surgeries in some cases: for example, spine region was unspecified in 9% of cases and it was difficult to determine surgery pathology in 7% of cases. This may have resulted in a slight underestimation within other categories, but is unlikely to have affected the overall findings. Finally, it is acknowledged that a more nuanced comparison of neurosurgeons and orthopaedic surgeons, including the complexity of the surgeries and use of specific techniques or equipment, would have been interesting, but fell beyond the scope of what could be readily accomplished with the available data. Similarly, it was not possible to evaluate whether surgeries were necessary, or the outcomes thereof. These present topics for future study.
Conclusion
The present study found that spinal surgery with the largest open medical scheme in SA was dominated by surgery for degenerative pathology in older adults, and was performed largely by neurosurgeons. The findings highlighted the stark contrast in the profile of spine surgery between the private and public sectors, and the need for private-public collaboration. Furthermore, the findings support the need for spine fellowships for all specialists intending to practise spinal surgery, so that those entering the field are well prepared for their scope of practice.
Declaration. None.
Acknowledgements. The anonymised data analysed for the purposes of this study were obtained from Discovery Health Medical Scheme, registration number 1125, and with the support and assistance of Discovery Health (Pty) Ltd, an accredited administrator and managed care provider for medical schemes. Discovery Health Medical Scheme and Discovery Health (Pty) Ltd had no influence on the methodology used, analysis completed and conclusions drawn in this research, and the outcome of the research is entirely independent from Discovery Health Medical Scheme and Discovery Health (Pty) Ltd. The authors would like to thank Dr C Lombard from the Stellenbosch University Division of Epidemiology and Biostatistics for his guidance with the statistical analyses.
Author contributions. TNM: conceptualisation, formal analysis, writing - original draft; AJV, RND and SM: writing - review and editing; [HD: conceptualisation; formal analysis; writing - review and editing.
Funding. None.
Conflicts of interest. None.
References
1. Otani K, Kikuchi S, Yabuki S, et al. Lumbar spinal stenosis has a negative impact on quality of life compared with other comorbidities: An epidemiological cross-sectional study of 1 862 community-dwelling individuals. Scien World J 2013;2013:590652. https://doi.org/10.1155/2013/590652 [ Links ]
2. Sadosky AB, DiBonaventura M, Cappelleri JC, Ebata N, Fujii K. The association between lower back pain and health status, work productivity, and health care resource use in Japan. J Pain Res 2015;2015(8):119-130. https://doi.org/10.2147/JPR.S76649 [ Links ]
3. Hartvigsen J, Hancock MJ, Kongsted A, et al. What low back pain is and why we need to pay attention. Lancet 2018;391(10137):2356-2367. https://doi.org/10.1016/S0140-6736(18)30480-X [ Links ]
4. Zaina F, Tomkins-Lane C, Carragee E, Negrini S. Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochr Database Syst Rev 2016;2016(1):CD010264. https://doi.org/10.1002/14651858.CD010264.pub2 [ Links ]
5. Fessler RG. Surgery versus nonsurgery for lumbar spinal stenosis: An in-depth analysis of the 2016 Cochrane analysis, the studies included for analysis, and Cochrane methodology. J Neurosurg Spine 2021;35(5):1-9. https://doi.org/10.3171/2021.1.SPINE201894 [ Links ]
6. Held U, Steurer J, Pichierri G, et al What is the treatment effect of surgery compared with nonoperative treatment in patients with lumbar spinal stenosis at 1-year follow-up? J Neurosurg Spine 2019;31(2):185-193. https://doi.org/10.3171/2019.1.SPINE181098 [ Links ]
7. Kotkansalo A, Leinonen V, Korajoki M, Salmenkivi J, Korhonen K, Malmivaara A. Surgery for degenerative cervical spine disease in Finland, 1999 - 2015. Acta Neurochir 2019;161(10):2147-2159. https://doi.org/10.1007/s00701-019-03958-6 [ Links ]
8. Xu Y, Yen D, Whitehead M, Xu J, Johnson AP. Use of instrumented lumbar spinal surgery for degenerative conditions: Trends and costs over time in Ontario, Canada. Can J Surg 2019;62(6):393-401. https://doi.org/10.1503/cjs.017016 [ Links ]
9. Cram P, Landon BE, Matelski J, et al. Utilisation and outcomes for spine surgery in the United States and Canada. Spine 2019;44(19):1371-1380. https://doi.org/10.1097/BRS.0000000000003083 [ Links ]
10. Martin BI, Mirza SK, Spina N, Spiker WR, Lawrence B, Brodke DS. Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the United States, 2004 to 2015. Spine 2019;44(5):369-376. https://doi.org/10.1097/BRS.0000000000002822 [ Links ]
11. Waheed MA, Hasan S, Tan LA, et al. Cervical spine pathology and treatment: A global overview. J Spine Surg 2020;6(1):340-350. https://doi.org/10.21037/jss.2020.01.12 [ Links ]
12. Kobayashi K, Sato K, Kato F, et al. Trends in the numbers of spine surgeries and spine surgeons over the past 15 years. Nagoya J Med Sci 2022;84:155-162. https://doi.org/10.18999/nagjms.84.1.155 [ Links ]
13. Grotle M, Smástuen MC, Fjeld O, et al. Lumbar spine surgery across 15 years: Trends, complications and reoperations in a longitudinal observational study from Norway. BMJ Open 2019;9(8):e028743. https://doi.org/10.1136/bmjopen-2018-028743 [ Links ]
14. Sah HK, Shrestha DK, Rajbhandari B, et al. Profile and outcome of adult spine pathologies managed in a neurosurgical tertiary care center in Nepal. J Inst Med Nepal 2020;42(1):54-58. https://doi.org/10.3126/JIOM.V42I1.37428 [ Links ]
15. Miseer S, Mann T, Davis J. Burden and profile of spinal pathology at a major tertiary hospital in the Western Cape, South Africa. SA Orth Jm2019;18(1):33-39. https://doi.org/10.17159/2309-8309/2019/v18n1a4 [ Links ]
16. Mann TN, Schaaf HS, Dunn RN, et al. Child and adult spinal tuberculosis at tertiary hospitals in the Western Cape, South Africa: 4-year burden and trend. Epidemiol Infect 2018;146(16):2107-2115. https://doi.org/10.1017/S0950268818002649 [ Links ]
17. Mkize S, Dunn R. Proximal junctional kyphosis post tuberculous spine corrective surgery in paediatric patients. Spine Deform 2021;9(1):169-174. https://doi.org/10.1007/s43390-020-00186-2 [ Links ]
18. Fieggen G. Neurosurgery in South Africa. S Afr Med J 2014;104(4):254. https://doi.org/10.7196/SAMJ.8213 [ Links ]
19. Discovery Health Medical Scheme. Results highlights for the six months ended 31 December 2017. Cape Town: DHMS, 2017. https://www.discovery.co.za/medical-aid/annual-reports-and-financials (accessed 11 October 2022). [ Links ]
20. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 2005;43(11):1130-1139. https://doi.org/10.1097/01.mlr.0000182534.19832.83 [ Links ]
21. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 1987;40(5):373-383. https://doi.org/10.1016/0021-9681(87)90171-8 [ Links ]
22. Daniels AH, Ames CP, Smith JS, Hart RA. Variability in spine surgery procedures performed during orthopaedic and neurological surgery residency training: An analysis of ACGME case log data. J Bone Joint Surg Am 2014;96(23):e196. https://doi.org/10.2106/JBJS.M.01562 [ Links ]
23. Malempati H, Wadey VMR, Paquette S, et al. Spinal surgery fellowship education in Canada: Evaluation of trainee and supervisor perspectives on cognitive and procedural competencies. Spine 2013;38(1):83-91. https://doi.org/10.1097/BRS.0B013E3182640F69 [ Links ]
 Correspondence:
Correspondence:
T N Mann
tmann@sun.ac.za
Accepted 25 April 2023














