Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
SAMJ: South African Medical Journal
versão On-line ISSN 2078-5135
versão impressa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 no.7 Pretoria Jul. 2023
http://dx.doi.org/10.7196/SAMJ.2023.v113i7.365
RESEARCH
Evaluation of the national clinical sentinel surveillance system for sexually transmitted infections in South Africa: Analysis of provincial and district-level data
D FrankI; T KufaII, III; P DorrellIV; R KularatneV; R MaithufiVI; T ChidarikireVII; Y PillayVIII, IX; M MokgatleX
IBPharm, M.Pharm; Clinton Health Access Initiative, Johannesburg, South Africa
IIMB ChB, PhD; Centre for HIV and STIs, National Institute of Communicable Diseases, Johannesburg, South Africa
IIIMB ChB, PhD; School of Public Health, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IVBA Hons, MPhil; Clinton Health Access Initiative, Johannesburg, South Africa
VMB ChB, FCPath; Department of Clinical Microbiology and Infectious Diseases, School of Pathology, Faculty of Health Sciences, University of the Witwatersrand., Johannesburg, South Africa
VIBNurs, MPH; National Department of Health, Pretoria, South Africa
VIIBSc, PhD; National Department of Health, Pretoria, South Africa
VIIIBSc, PhD; Clinton Health Access Initiative, Johannesburg, South Africa
IXBSc, PhD; Department of Global Health, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
XBrad (Diagn), PhD; School of Public Health, Sefako Makgatho Health Sciences University, Pretoria, South Africa
ABSTRACT
BACKGROUND: Globally, >1 million new cases of curable sexually transmitted infections (STIs) are estimated to occur daily, an alarming rate that has prevailed for over a decade. Modelled STI prevalence estimates for South Africa (SA) are among the highest globally. Robust STI surveillance systems have implications for policy and planning, antimicrobial stewardship and prevention strategies, and are critical in stemming the tide of STIs
OBJECTIVES: To evaluate the STI clinical sentinel surveillance system (STI CSSS) in SA, to describe the population incidence of four designated STI syndromes in males and females >15 years, and to provide recommendations for strengthening the STI CSSS
METHODS: This was a retrospective analysis of the STI CSSS in SA. Distribution of the primary healthcare facilities designated as STI CSSS sites was described, taking into account provincial population distribution and headcount coverage of STI CSSS facilities. Reporting compliance was evaluated to determine completion of data reporting. Further analysis was undertaken for those provinces that had good reporting compliance over a 12-month period. Population-level and demographic STI syndrome incidence were estimated from CSSS data using case reports of male urethritis syndrome (MUS) as a proxy for data extrapolation
RESULTS: Reporting compliance exceeded 70% for seven of the nine provinces. STI syndromes with the highest incidence were MUS and vaginal discharge syndrome (VDS). The 20 - 24 years age group had the highest STI incidence, at least double the incidence estimated in the other two age groups. Overall STI incidence in females was higher than among males in all provinces, except Limpopo and Western Cape. The 15-19 years age group had the most prominent gender disparity, with the national STI incidence in females 70% higher than in males. District-level analysis revealed high regional STI incidence even in provinces with lower overall incidence
CONCLUSION: The STI CSSS is pivotal to epidemiological monitoring and proactive management of STIs, especially in view of the high HIV prevalence in SA. CSSS processes and facility selection should be reviewed and revised to be representative and responsive to the current STI needs of the country, with biennial analysis and reporting to support evidence-based policy development and targeted implementation
Sexually transmitted infections (STIs) remain a significant global health challenge owing to the impact on population health outcomes, healthcare resource challenges and socioeconomic burden.[1] In 2017, World Health Organization estimates of syphilis, gonorrhoea and chlamydia infections in South Africa (SA) suggested >4 million cases in women and 6-10 million cases in men aged 15-49 years.[2] Prevalence estimates of 6.6% and 3.4% for gonorrhoea and 14.7% and 6.0% for chlamydia in women and men, respectively, are among the highest globally[2] In addition to acute illness, which is often easily treatable, undiagnosed, untreated or suboptimally treated STIs and repeated infections may increase the risk of severe sequelae, vertical transmission and HIV acquisition or transmission.[1,3-6] STI surveillance and control interventions are, therefore, increasingly recognised as a public health priority.
In SA, primary healthcare (PHC) services in the public sector are provided free of charge through >3 500 clinics and community health centres, located within 5 km of 90% of the population.[7] Symptomatic STIs are managed syndromically, whereby individuals are treated for all common aetiological agents associated with the presenting symptoms.[8] STI surveillance in the country includes a combination of (i) clinical sentinel syndromic reporting and (a) aetiological testing studies with relative prevalence estimation and antimicrobial resistance monitoring. The former is conducted on an ongoing basis, has a larger population coverage and can provide timeous, nationally representative data to guide evidence-based interventions and monitor the impact of interventions. Since data collection is undertaken at a small number of facilities, sentinel surveillance enables STI epidemiological monitoring, without overburdening the healthcare system through data collection. This article describes the functionality of the STI clinical sentinel surveillance system (CSSS) in SA and the estimated incidences of designated STI syndromes among specified populations, and provides recommendations to strengthen the system.
Methods
STI clinical sentinel surveillance system
The STI CSSS operates at -270 PHC facilities, in 47 of the 52 health districts across all nine provinces in SA. Initial facility selection was done such that each province had 30 reporting facilities, each with a headcount >5 000 and treating >25 male urethritis syndrome (MUS) cases monthly. Subsequently, provincial distribution of facilities changed for various reasons.
Between April 2019 and March 2020, the STI CSSS included 24 data elements incorporating syndromic and demographic components of new STI cases. STI syndromes included MUS and MUS treatment failure, vaginal discharge syndrome (VDS), genital ulcer syndrome (GUS), genital warts (GW), lower abdominal pain in females (LAP) and an umbrella data element termed other STIs'. Additionally, syphilis among pregnant women and treatment with benzathine benzylpenicillin G was reported. Age and gender stratification of STI patients ranged from children <10 years to adults >25 years. The complete list of data elements is presented in Table SI appendix: https://www.samedical.org/file/2038). Data collection tools used for the STI CSSS were (i) tally sheets, used to record individual cases daily, and (ii) summary tools, whereby all facility-level data were aggregated monthly and reported through the STI Sentinel Surveillance module on the National Department of Health (NDoH) Integrated Web District Health Information System (DHIS). Data reporting ceased from April 2020 owing to removal of this module from the DHIS.
Data extraction and management
Monthly data for all 24 STI data elements from all STI CSSS facilities for the period April 2015 to March 2020 were extracted during June 2020 as an Excel (Microsoft Corp., USA) spreadsheet, and analysed in Excel.[9] The provincial distribution of STI CSSS facilities, provincial populations and provincial PHC attendance at STI CSSS facilities were investigated. The complete data set was used to determine reporting compliance, as an indication of the data reporting performance of STI CSSS facilities. Further data analysis was undertaken on four selected STI syndromes (MUS, VDS, GUS and GW), as well as total STI incidence in males and females aged 15-19 years, 20 - 24 years and >25 years for the period April 2019 to March 2020, which will be the focus of this publication. Data elements that were not sufficiently specific or did not add significant value to STI trend analyses, as well as data elements for age groups >15 years where the data reports were low and erratic, were excluded from the evaluation.
Data analysis
Descriptive statistics were used to describe the STI CSSS. Reporting compliance for the evaluation period was determined at facility level and aggregated to subnational and national levels. Reporting compliance was calculated as follows:
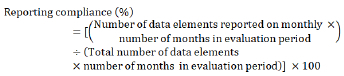
All zero reports were considered legitimate data reports, with the assumption that there were no cases treated during that month at the relevant facility. To assess the magnitude of zero reports, an analysis was performed at district level to determine the proportion of data reports that were zero reports for MUS and VDS, the two data elements where zero reports are least likely. Provincial monthly reporting compliance was also calculated excluding zero reports for MUS and VDS.
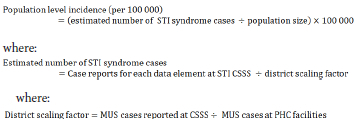
STI cases reported at STI CSSS facilities were extrapolated to estimate population-level incidence. MUS is the only data element reported at STI CSSS facilities as well as all other PHC facilities, and was therefore used as the basis for extrapolation. The underlying assumption was that reporting trends would not differ significantly across individual STI CSSS data elements. This assumption was supported by comparing reporting compliances calculated for each data element. A district-level scaling factor was calculated using the proportion of MUS cases reported at CSSS facilities relative to MUS cases reported across all PHC facilities in a district. This scaling factor was applied to all data elements reported at CSSS facilities to estimate the total cases of each STI syndrome, or clients who would have been treated in each district, and aggregated to provincial and national levels. Mid-year district-level population (15 -49 years) estimates from the DHIS were used to calculate population-level incidence of the selected STI syndromes or in selected demographic groups, as follows:
Results
The STI clinical sentinel surveillance system
Previous CSSS site selection criteria have resulted in inequitable provincial distribution of STI CSSS facilities relative to provincial populations, as shown in Table S2 (appendix). KwaZulu-Natal and Gauteng provinces were significantly under-represented in the number of designated STI CSSS facilities compared with the provincial populations. Northern Cape Province had a notably high proportion of STI CSSS facilities relative to the provincial population. The proportion of CSSS facilities in Limpopo, Mpumalanga and Western Cape provinces aligned more closely with their relative provincial population sizes. There was also notable interprovincial variation in the proportion of total provincial PHC headcount attending designated STI CSSS facilities (range 9 - 25%).
Reporting compliance
Reporting compliance at STI CSSS facilities was low, and variable across all provinces prior to April 2019. Fig. 1 illustrates provincial reporting compliance between November 2018 and March 2020, highlighting the significant increase in reporting compliance for all provinces in April 2019. Between April 2019 and March 2020, seven provinces demonstrated consistent data reporting, with average reporting compliance >70%. Hence, this period was selected as the evaluation period for this report.
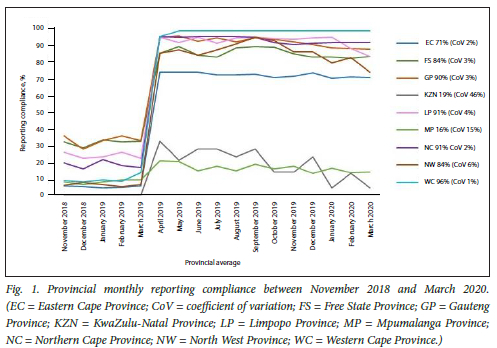
Western Cape province had the most consistent reporting and the highest average reporting compliance over the evaluation period followed by Northern Cape, Limpopo and Gauteng provinces, all >90%. Of the provinces with acceptable average reporting compliance, North West had the greatest variation in reporting compliance across the evaluation period. Despite also demonstrating an increase in reporting compliance since April 2019, the overall reporting compliances for KwaZulu-Natal and Mpumalanga provinces were very low and inconsistent over the evaluation period.
Twenty-one districts had a reporting compliance >90% over the evaluation period. Four districts in KwaZulu-Natal had 0% reporting compliance. Reporting compliances for the three districts in Mpumalanga ranged between 15 and 18%. Low reporting compliance (defined as <50% for the purpose of this evaluation) compromised the ability to draw insightful conclusions from the data and skewed national statistics, hence data from KwaZulu-Natal and Mpumalanga were excluded from the subsequent analyses.
The proportion of zero reports for MUS and VDS at district level ranged between 0% and 35% and 2% and 83%, respectively. Seven of the 38 districts had the proportion of zero reports to all MUS data reports > 10%, and for VDS this increased to 29 districts. When zero reports for MUS and VDS were excluded, the decrease in overall provincial reporting compliance was insignificant (<2%). The provincial proportions of zero reports for MUS and VDS are presented in Table S3 (appendix).
Overall STI incidence
Nationally, there were >76 000 cases of the four designated STI syndromes reported at CSSS facilities during the evaluation period. Estimated incidence rates for each STI syndrome are presented in Table 1. There are three provinces with overall high STI burden, namely Eastern Cape, Free State and Gauteng, while Limpopo and North West appeared to have low STI incidence rates. However, the analysis of zero reports highlighted a distinct inverse relationship between proportion of zero reports and estimated STI incidence rates, i.e. provinces with a high proportion of zero reports had lower estimated STI incidence rates, which may be a result of inaccurate reporting.
Male urethritis syndrome
MUS had the highest estimated incidence of all the STI syndromes reported. Over 39 000 MUS cases were reported at STI CSSS facilities, with a national estimated incidence of 1 913 cases/100 000 population. Eastern Cape and Western Cape provinces reported the highest estimated provincial MUS incidence, which were more than double the lowest estimated incidence reported in North West.
Four districts in Eastern Cape Province (Chris Hani, Oliver Tambo, Joe Gqabi and Buffalo City) had the highest estimated district MUS incidence, as illustrated in Fig. 2. Sixteen districts (42%) had estimated MUS incidence above the national average, which, with the exception of North West, included at least one district from each province and all eight districts from Eastern Cape. Despite Limpopo having a low estimated provincial MUS incidence, Waterberg ranked among these 16 districts.
Vaginal discharge syndrome
VDS was the second most frequently reported STI syndrome, with >31 000 cases reported at STI CSSS facilities and an estimated national incidence of 1 569/100 000 population. The highest estimated provincial VDS incidences were reported in Eastern Cape, Free State and Gauteng provinces. North West and Limpopo had the lowest estimated VDS incidences, less than half that of the three highest-burdened provinces.
Sixteen districts had estimated VDS incidences above the national average (Fig. 3), which included at least one district from each province, except Limpopo. Despite North West having a low estimated provincial VDS incidence, Dr Ruth Segomotsi Mompati district ranked among these 16 districts. Xhariep had a notably high estimated VDS incidence, >35% higher than the next highest estimated district incidence reported in Chris Hani, and almost five-fold the estimated incidence in neighbouring Mangaung.
Genital ulcer syndrome
Nationally, >3 700 GUS cases were reported at STI CSSS facilities, 54% of which were in females. Females had a higher estimated GUS incidence than males nationally and in all provinces except Limpopo and North West. Gauteng had the highest provincial estimated GUS incidence for both genders. For males, the estimated incidence in Gauteng was significantly higher than other provinces, 57% higher than the next highest estimated incidence reported in Free State and >3 times higher than the lowest estimated incidence reported in Limpopo. The largest gender disparity in estimated GUS incidence was observed in Eastern Cape, where the incidence in females exceeded that in males by >80%.
Fig. 4 presents district GUS incidence rates by gender. Six districts had GUS incidence >200/100 000 population in females. In males, City of Johannesburg, Joe Gqabi and City of Tshwane had the highest estimated GUS incidences. Seventeen districts for females and 12 districts for males had estimated GUS incidence higher than the national average, nine of which were common to both genders. This included Overberg and West Coast in Western Cape, where overall provincial incidences for males and females was low. The largest gender disparities in estimated GUS incidence were observed in Buffalo City, Sedibeng, Xhariep and Chris Hani.
Genital warts
Over 1 600 GW cases were reported at STI CSSS facilities nationally, with females accounting for 62% of cases. Free State and Gauteng provinces equally demonstrated the highest estimated GW incidence in females. Free State also had the highest estimated GW incidence in males, followed by Eastern Cape and Gauteng.
Fig. 5 presents estimated district GW incidences by gender. Four districts (Xhariep, Sedibeng, Amathole and Lejweleputswa) had estimated GW incidence in females > 100/100 000 population. In males, Joe Gqabi reported the highest estimated GW incidence, >60% higher than Capricorn, the second-highest district.
Estimated STI incidence by age and gender
Females had a higher overall STI incidence than males nationally, and in all provinces except Limpopo and Western Cape, where STI incidence in males was respectively 15% and 18% higher than in females. Table 2 outlines the estimated national and provincial STI incidences in males and females in each of the three age groups. The largest gender disparity in estimated STI incidence was observed in the 15 - 19-year age group, and reduced progressively with the older age groups. The estimated STI incidence was highest in the 20 - 24-year age group for both genders, significantly higher than the 15 - 19-year and >25-year age groups.
Fig. 6 illustrates the estimated district STI incidence for males and females in each age group. Some districts demonstrated distinct trends in the age/gender demographic groups with high estimated STI incidences. For example, City of Cape Town ranked among the top 10 districts for males in all three age groups, and Xhariep, Lejweleputswa, City of Tshwane and Sedibeng for females. City of Johannesburg and Amathole demonstrated high estimated STI incidences in males and females aged 15 - 19 and 20 - 24 years. Seven districts (John Taolo Gaetsewe, West Coast, Buffalo City, Mangaung, Fezile Dabi, West Rand and Thabo Mofutsanyana) featured among the highest 10 districts only for the >25 years age group. Despite Limpopo having among the lowest provincial estimated STI incidences for all age/ gender demographic groups, Waterberg featured among the highest 10 districts for males aged 20 - 24 years.
Discussion
Low reporting compliance prior to April 2019 may be attributed to inconsistent availability of data collection tools in facilities. This challenge was addressed in 2019 through national co-ordination addressing availability of data collection tools. In addition, challenges with the DHIS STI Sentinel Surveillance module were addressed, and regular meetings were initiated with provincial managers, which are all thought to have contributed to improved reporting rates. However critical shortfalls in completion and quality of data reports were identified, which compromises surveillance efforts. Since MUS is part of the national indicator data set (NIDS), the notably higher proportion of zero reports for VDS compared to MUS suggests under-reporting for STI CSSS data elements. The analysis of these zero reports found a pertinent correlation between the proportion of zero reports for MUS and VDS and the relative estimated STI burden in provinces, i.e. provinces with a high proportion of zero reports appeared to have lower STI incidence than those with lower proportions of zero reports. Hence, STI incidence presented in this evaluation may be underestimated, and classification of provinces as relatively low incidence should be applied with caution. Notwithstanding these limitations, the analysis provided valuable insights on incidence of STI syndromes in SA - identifying geographical and demographic hotspots for STI syndromes. Importantly, this analysis also provides a baseline for longitudinal trend analysis and measuring the impact of programmatic changes.
Based on sentinel surveillance, four provinces were identified as relatively high-burdened provinces: Gauteng, Eastern Cape, Western Cape and Free State. District-level analysis proved critical, since localised hotspots were masked by prevailing provincial trends. Reported data also demonstrated the relative burden of different STI syndromes. MUS and VDS had the highest estimated incidences, with the incidence of GUS, the next most-frequently reported syndrome, being 7 - 10-fold lower. The data indicate a high crude estimated STI incidence of almost 2 000/100 000 population in both males and females, with the highest incidence in the 20 -24-year age group. Adolescent girls and young women (15 -24 years) demonstrated the highest STI incidence. This mirrors, and could possibly be contributing to, the HIV incidence trends in the country.[10] In addition, this finding highlights the importance for STI and HIV service integration at facilities and the need for interventions that are within the control of females. Within each province, age/gender stratification further revealed specific demographic hotspots. For instance, age stratification revealed that the estimated STI incidence in Free State is noticeably skewed towards the >25-year age group, while gender stratification showed that Western Cape has notably higher STI incidence in males. It is important to note that these incidence rates are likely underestimates of the true population burden in the provinces, as they represent only symptomatic patients accessing healthcare services at public sector PHC facilities.
In SA, the predominant causative organism of MUS is Neisseria gonorrhoeae, with prevalence estimates of 75% - 85% in national and sentinel surveys.[8,11,12] Neisseria gonorrhoeae is a rapidly evolving organism with a remarkable capacity to acquire resistance to first-line antimicrobial agents used for gonorrhoea/MUS treatment.[8,13] Monitoring antimicrobial resistance profiles through aetiological surveillance of MUS is critical for revision of STI syndromic management guidelines. MUS incidence trends generated from STI CSSS data would provide essential information for STI aetiological, risk factor and antimicrobial resistance surveillance studies.
Treponema pallidum, the causative agent of syphilis, is the second most commonly implicated pathogen in GUS, after herpes simplex virus, accounting for -10% of GUS cases in a sentinel aetiological surveillance study.[12] Congenital syphilis is targeted for eradication locally and globally, hence GUS incidence trends and antenatal syphilis prevalence are key data points for surveillance.
The findings described above and the identification of regional STI hotspots are important for effective health service planning, to forecast needs and determine resource allocation. It is also a crucial input to designing effective and evidence-based STI/HIV prevention strategies. For instance, identification of areas with higher STI incidence in females could be used to target demand generation for female condoms, since this will have the advantage of being an effective self-initiated contraceptive and STI/HIV prevention method. Regions with high STI incidence in males may be targeted for tailored, male-focused interventions and delivery methods, and areas with high STI incidence in males and females could be targeted for intensified STI and HIV prevention interventions and studies to determine the underlying reasons and guide the interventions. In addition, healthcare worker capacitation could be enhanced and tailored to be responsive to the needs of particularly vulnerable demographic cohorts in different regions.
Limitations
Interprovincial distribution of STI CSSS facilities was inequitable, potentially limiting the generalisability of surveillance data, which undermines the premise of sentinel surveillance.
The validity of the data presented is entirely dependent on the accuracy and completeness of data reporting. Data auditing and validation with clinical records were beyond the scope of this evaluation, resulting in a reliance on data quality assurance at subnational levels prior to reporting on DHIS. A few reporting anomalies were identified, which were adjusted to mirror the prevailing trend for the facility. This also highlights the pivotal role of sub-national capacitation and strengthening for data quality assurance processes.
The high number of facilities reporting 0 cases of common syndromes such as MUS and VDS is a cause for concern. The lack of any reporting for these very common syndromes from facilities with high headcounts raises fundamental concerns about the accuracy of the data reporting. Lastly, the sentinel surveillance that produces this data is conducted at PHC facilities, and the estimates of incidence are therefore affected by both burden of disease in the catchment areas of the clinics as well as health-seeking behaviours. The relative contribution of disease burden and health-seeking practices to these estimates cannot be determined with the information that is available. Population-based surveys to determine STI burden maybe informative.
Recommendations and implications for the STI programme
The STI CSSS is a uniquely detailed data source, and as such can have far-reaching impact on how the national STI programme can be designed to best achieve the goals of the National Strategic Plan for HIV, TB and STIs.[14] While there are several recommendations that can be drawn at the local level from this data, some high-level recommendations are as follows:
• Selection of CSSS facilities should be re-evaluated to ensure equitable representation across provinces, ensuring accurate generalisability of surveillance outcomes.
• The STI CSSS should be strengthened through review of the data elements collected and the data collection and reporting processes, to ensure that the input justifies the value and is responsive to the current needs of the heath system.
• STI geographic and demographic hotspots should be prioritised for STI awareness-building and prevention interventions. These interventions should be conducted in all provinces with campaigns adjusted to address specific areas of concern, e.g. 15 -19-year-olds in Eastern Cape Province.
• Subnational capacitation is required for effective data reporting, monitoring and evaluation, to improve data quality and facilitate identification, investigation and resolution of potential data anomalies in a timeous manner. Quarterly data reviews and meetings with provincial managers should be initiated, at least for the first year following reintroduction of the STI CSSS, to support high and consistent data completion and quality.
• The current data should be used as a baseline for future trend analysis on a biennial basis, at a minimum. Efforts to ensure that these data are consistently collected through the DHIS should be prioritised.
• To optimise value of the STI CSSS, the functionality of the system should be routinely evaluated, and a change management process implemented to strengthen the system.
Conclusion
The STI CSSS has several crucial implications across the health system, and ongoing surveillance and regular publication of the data are critical to evidence-based strategic planning, policy development and effective utilisation of resources to optimise impact. The CSSS should be periodically reviewed to ensure that the value-add of the system is maintained. This system could play a pivotal role in designing and monitoring interventions that will accelerate progress towards the National Strategic Plan STI-related goals.
Declaration. None.
Acknowledgements. The authors would like to acknowledge the healthcare workers and data capturers at the STI CSSS facilities, and district and provincial managers for the data reporting that supported this publication.
Author contributions. DF: manuscript conceptualisation, data extraction and analysis, drafted background section and contributed to all other sections, preparation of figures and tables, review of manuscript. T K-C: data analysis, drafted methods section, review of manuscript. PD: conceptualisation of manuscript, contributed to all sections, and review of manuscript. RK: contributed to manuscript design, interpretation of results, drafted discussion section and critical review of manuscript. RM: contributed to recommendations and implications for the STI programme section. TC: review of manuscript. YP: critical review of manuscript. MM: preliminary data analysis, drafted results section, final review.
Funding. This work was funded by the Bill and Melinda Gates Foundation as part of a grant awarded to the Clinton Health Access Initiative. The publication costs were funded by the School of Public Health Sefako Makgatho Health Sciences University.
Conflicts of interest. None.
References
1. Eisinger R W, Erbelding E, Fauci AS. Refocusing research on sexually transmitted infections. J Infect Dis 2020;222(9):1432-1434. https://doi.org/10.1093/infdis/jiz442 [ Links ]
2. Kularatne R S, Niit R Rowley J, et al. Adult gonorrhea, chlamydia and syphilis prevalence, incidence, treatment and syndromic case reporting in South Africa. Estimates using the Spectrum-STI model, 1990-2017. PLoS One 2018;13(10):0205863. https://doi.org/10.1371/journal.pone.0205863 [ Links ]
3. Rowley J, Vander Hoorn S, Korenromp E, et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis, global prevalence and incidence estimates, 2016. Bull World Health Org 2019;97(8):548-562. https://doi.org/10.2471/BLT.18.228486 [ Links ]
4. World Health Organization. Global health sector strategy on sexually transmitted infections 20162021. Geneva. WHO, 2016. https://apps.who.int/iris/bitstream/handle/10665/246296/?sequence=1 (accessed 8 July 2021). [ Links ]
5. Cohen M S. Classical Sexually transmitted diseases drive the spread of HIV-1. Back to the future. I Infect Dis 2012;206(1):1-2. https://doi.org/10.1093/infdis/jis303 [ Links ]
6. Ramjee G, Wilhams B, Gouws E,van Dyck E, Deken B, Karim SA. The impact of incident and prevalent herpes simplex virus-2 infection on the incidence of HIV-1 infection among commercial sex workers in South Africa. J AIDS 2005;39(3):333-339. https://doi.org/10.1097/01.qai.0000144445.44518.ea [ Links ]
7. World Health Organization, Alliance for Health Policy and Systems Research. Primary Health Care Systems (PRIMASYS). A case study from South Africa, abridged version. Geneva. WHO, 2017. https://apps.who.int/iris/handle/10665/341145 (accessed 8 July 2021). [ Links ]
8. Kularatne R Maseko V, Gumede L, Kufa T. Trends in Neisseria gonorrhoeae antimicrobial resistance over a ten-year surveillance period, Johannesburg, South Africa, 2008-2017. Antibiotics 2018;7(3):58. https://doi.org/10.3390/antibiotics7030058 [ Links ]
9. National Department of Health, South Africa. District Health Information System. [ Links ]
10. Dellar RC, Diamini S, Karim QA. Adolescent girls and young women. Key populations for HIV epidemic control J Int AIDS Soc 2015;18(2S1):19408. https://doi.org/10.7448/IAS.18.2.19408 [ Links ]
11. Kularatne R Radebe F, Kufa-Chakezha T, Mbulawa Z, Lewis D. Sentinel surveillance of sexually transmitted infection syndrome aetiologies and HPV genotypes among patients attending primary healthcare facilities in South Africa, April 2014-September 2015. Johannesburg National Institute for Communicable Diseases, Centre for HIV & STIs, 2017. https://www.nicd.ac.za/wp-content/uploads/2017/03/3Final-25-April-2017_Revised-NAS_v5_NICD.pdf (accessed 8 July 2021). [ Links ]
12. Kularatne R. Aetiological surveillance of sexually transmitted infection syndromes at sentinel sites. GERMS SA 2018. Johannesburg National Institute of Communicable Diseases, 2019. [ Links ]
13. Unemo M, Shafer W M. Antimicrobial resistance in Neisseria gonorrhoeae in the 21st century. Past evolution and future. Clin Microbiol Rev 2014;27(3):587-613. https://doi.org/10.1128/CMR.00010-14 [ Links ]
14. South African National Department of Health. South Africa's national strategic plan for HIV, TB and STIS 2017-2022. Pretoria. NDoH, 2017. [ Links ]
 Correspondence:
Correspondence:
D Frank
derushaf@gmail.com
Accepted 13 April 2023














