Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 n.6 Pretoria Jun. 2023
http://dx.doi.org/10.7196/SAMJ.2023.v113i6.16554
RESEARCH
Factors associated with COVID-19 inpatient mortality cases within 24 hours in South Africa
P M MphekgwanaI; M E Sono-SetatiII, III; T G TshitanganoIV; S F MatlalaV; N J RamalivhanaVI, VII
IBSc Hons, MSc; Research Administration and Development, University of Limpopo, Polokwane, South Africa
IIMB ChB, MMed (Public Health Medicine); Department of Public Health Medicine, School of Medicine, Faculty of Health Sciences, University of Limpopo, Polokwane, South Africa
IIIMB ChB, MMed (Public Health Medicine); Limpopo Department of Health, Hospital Park, Polokwane, South Africa
IVMPH, PhD; Department of Public Health, Faculty of Health Sciences, University of Venda, Ihohoyandou, South Africa
VMPH, PhD; Department of Public Health, Faculty of Health Sciences, University of Limpopo, Polokwane, South Africa
VIMPH, PhD; Limpopo Department of Health, Hospital Park, Polokwane, South Africa
VIIMPH, PhD; Department of Public Health, Faculty of Health Sciences, University of Venda, Ihohoyandou, South Africa
ABSTRACT
BACKGROUND: African countries with limited healthcare capacity are particularly vulnerable to the novel coronavirus (COVID-19). The pandemic has left health systems short on resources to safely manage patients and protect healthcare workers. South Africa (SA) is still battling the epidemic of HIV/AIDS and tuberculosis (TB), which had their programme/services interrupted due to the effects of the pandemic. Lessons learnt from the HIV/AIDS and TB programme have shown that South Africans delay seeking health services when a new disease presents itself
OBJECTIVE: To investigate the risk factors for COVID-19 inpatients' mortality within 24 hours of hospital admission in public health facilities in Limpopo Province, SA
METHODS: The study used retrospective secondary data obtained from the 1 067 clinical records of patients admitted between March 2020 and June 2021 by the Limpopo Department of Health (LDoH). A multivariable logistic regression model, both adjusted and unadjusted, was used to assess the risk factors associated with COVID-19 mortality within 24 hours of admission
RESULTS: This study, which was conducted in Limpopo public hospitals, discovered that 411 COVID-19 patients (40%) died within 24 hours of admission. The majority of the patients were aged >60 years, mostly of female gender, and had comorbidities. In terms of vital signs, most had body temperatures <38°C. Our study findings revealed that COVID-19 patients who present with fever and shortness of breath were 1.8 and 2.5 times more likely to die within 24 hours of admission to the hospital, respectively, than patients without fever and with normal respiratory rate. Hypertension was independently associated with mortality in COVID-19 patients within 24 hours of admission, with a high odds ratio (OR) for hypertensive patients (OR 1.451; 95% confidence interval 1.013 - 2.078) compared with non-hypertensive patients
CONCLUSION: Assessing demographic and clinical risk factors for COVID-19 mortality within 24 hours of admission aids in understanding and prioritising patients with severe COVID-19 and hypertension. Finally, this will provide guidelines for planning and optimising the use of LDoH healthcare resources, and also aid in public awareness endeavours
The world came to a halt as a result of the coronavirus (COVID-19) pandemic. The COVID-19 pandemic has had a significant impact on social, economic and population health around the world, and the end date of the outbreak is unknown.[14] African countries with limited healthcare capacity were particularly vulnerable to the novel Coronavirus.[4-6] In some countries, the pandemic left health systems short of resources to safely manage patients and protect healthcare workers.[6] South Africa (SA) is one of the developing countries still battling HIV/AIDS and tuberculosis (TB), leaving the country unsure of how the pandemic will progress. [7,8] COVID-19 presents as a complicated clinical illness with a potential for complications that may necessitate ongoing clinical care.[9,10] The disease's clinical manifestation can be mild, moderate to severe or critical.
According to recent studies, the most common symptoms of COVID-19 at the onset of the illness were fever, cough, fatigue, dyspnoea and headache.[11,12] Excess mortality has been reported in studies conducted worldwide, which are associated with comorbidities such as cancer, chronic kidney diseases, diabetes mellitus and hypertension.[11,13,14] Behavioural risk factors such as being a smoker were also noted as associated factors of COVID-19.[15] Length of hospital stay was significantly associated with severe COVID-19 patients.[12]
The length of hospital stay varies by country, with the USA, Italy and Germany having 2 - 10, 1 - 6 and 5-19 days, respectively, and China having 4-53 days.[16,17] Studies conducted in SA reported a median length of stay of 7 - 8 days in previous waves (1, 2 and 3) and 3 days in wave 4.[18] Patients who present with breathing difficulties, incident organ failure, a low leukocyte count, age >60 years and a high blood urea nitrogen level should be expected to stay in the hospital for an extended period.[11,19] However, our knowledge of the literature on risk factors for mortality in public hospitals within 24 hours of patient admission is limited, particularly in SA. The present study sought to fill a gap in the literature by investigating risk factors for COVID-19 inpatient mortality within 24 hours of hospital admission in public health facilities in Limpopo Province, SA. This will aid in COVID-19 prevention and public awareness endeavours, as well as the planning and allocation of health resources in public hospitals.
Methods
Study setting, period and design
This study was carried out in Limpopo Province using retrospective secondary COVID-19 data from the Limpopo Department of Health (LDoH)'s public hospitals across all districts. Limpopo Province has
41 public hospitals that admitted COVID-19 patients referred from home, clinics and other hospitals. The study used retrospective secondary data collected from 1 067 patients' clinical records of laboratory-confirmed COVID-19 cases admitted between March 2020 and June 2021. Non-laboratory-confirmed COVID-19 cases were excluded. In our previous study, it was reported that Capricorn had the highest case fatality rate (CFR) (4%), followed by Vhembe (3.9%), then Mopani (3.8%), with Waterberg (3.1%) and Sekhukhune (2.5%) having the smallest CFRs.[14] Furthermore, the overall Limpopo Province COVID-19 inpatient CFR was 3.55 (cumulative admission cases = 63 473 and COVID-19 deaths cases = 2 256).
Statistical analysis
The data were retrieved from LDoH databases, coded, recorded and entered into Excel (Microsoft Corp., USA) before being imported into the Statistical Package for Social Sciences (SPSS) version 26 (IBM Corp., USA) for further analysis. The information was presented in the form of frequency and percentages. A multivariable logistic regression model, both adjusted for gender and unadjusted, was used to assess the clinical risk factors associated with COVID-19 mortality within 24 hours of admission in Limpopo Province, SA. All statistical analyses were carried out using SPSS version 26, and predictor variables were presented using both adjusted and unadjusted odds ratios (ORs) at 95% confidence intervals (CIs). The statistical significance was set at 5%.
Ethical approval
The study was approved by the University of Limpopo Research Ethics Committee (ref. no. TREC/293/2021: IR) and the Limpopo Provincial Health Research Committee (ref. no. LP_2021-11-017).
Results
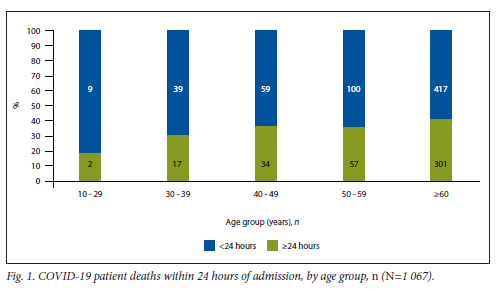
Table 1 shows the total cases of inpatient admissions and the case fatality rate within 24 hours of admission in Limpopo Province's five districts. COVID-19 patients admitted to the hospital had the highest mortality rate within 24 hours in the Sekhukhune and Mopani districts. Patients aged >60 years showed the highest proportion of patients dying within 24 hours of admission to the hospital (Fig. 1). The lowest rate was observed in patients between 10 and 30 years of age. Furthermore, patients with body temperatures ranging from 0°C to 30°C had the highest proportion of patients dying within 24 hours of being admitted to the hospital (Table 1). A total of 411 (40%) COVID-19 patients died within 24 hours of admission.
Of the 1 067 hospitalised COVID-19 patients, the majority were hypertensive (n=683, 64%), followed by those suffering from diabetes mellitus (n=555, 52%) (Fig. 2). In terms of the clinical presentations of these COVID-19 patients, shortness of breath was common (n=896, 84%), followed by coughing (n=865, 81%) (Fig. 3). The study also observed that a small proportion of COVID-19 patients admitted to hospitals did not have any COVID-19 symptoms (n=29).
The logistic regression of the association between COVID-19 mortality within 24 hours of hospital admission and the clinical presentations before admission are illustrated in Table 2. There was a significant (p<0.05) association between COVID-19 mortality within 24 hours of hospital admission and shortness of breath among admitted COVID-19 patients, both unadjusted (OR 2.387; 95% CI 1.307 - 4.359) and adjusted (OR 2.565; 95% CI 1.390 -4.734) for gender. Only the adjusted model revealed a significant association between COVID-19 mortality within 24 hours of hospital admission and fever (OR 1.832; 95% CI 1.035 - 3.243) and coughing (OR 0.552; 95% CI 0.306 - 0.997).
The logistic regression of the association between COVID-19 mortality within 24 hours of hospital admission and comorbid conditions before admission is illustrated in Table 3. There was a significant (p<0.05) association between COVID-19 mortality within 24 hours of hospital admission and hypertension among admitted COVID-19 patients, both unadjusted (OR 1.450; 95% CI 1.012 - 2.078) and adjusted (OR 1.451; 95% CI 1.013 - 2.078) according to gender.
Discussion
This study determined factors associated with death among COVID-19 admitted patients in public hospitals in Limpopo Province. The study found a high COVID-19 inpatient case fatality rate within 24 hours of patient hospitalisation in the Sekhukhune and Mopani districts. To the best of our knowledge, this could be due to both patient and health system factors, such as late patient presentation and long hospital turnaround times (TAT) for COVID-19 laboratory results. According to a study done at Dhulikhel Hospital-Kathmandu University Hospital, Nepal, to determine the factors influencing TAT in the clinical laboratory nearly 36% of reports exceeded the predefined TAT, while only 7% of reports for routine tests did so.[20] Around 75% of reports with prolonged TAT were delayed for various additional analytical reasons, and 48% of all delayed reports were only discovered due to error by cash unit.
For both males and females, the highest percentage of COVID-19 deaths occurred between the ages of 55 and 59 years and 60 and 64 years, respectively[11,19] Our study found similar results, with patients aged >50 years having the highest mortality rate and patients between 10 and 30 years of age recording the lowest mortality rate. Overall, patients who died within 24 hours of hospitalisation had body temperatures <38°C. Our findings are similar to those of the study by Tharakan et αl.,[21] who reported that low body temperature at the time of COVID-19 patient hospitalisation is associated with a poor prognosis. Another study found that about a quarter of patients who tested positive for COVID-19 did not have a fever of >38°C at their arrival.[22] Higher body temperature at initial presentation did not show a significant association with mortality[21,22]
The literature shows that gender, fever, chronic kidney or liver disease before admission and increasing creatinine levels were associated with prolonged length of stay in patients with COVID-19.[11,13] Our study findings revealed that COVID-19 patients who presented with fever were 1.8 times more likely to die within 24 hours of admission to hospital than patients without fever. In contrast, Shi et al.[23] discovered that fever was not associated with an increased risk of mortality in COVID-19 patients. The difference in findings could also be attributed to the fact that our study focused on mortality within 24 hours of hospitalisation, and retrospective data collected for other purposes. Our study found that COVID-19 patients with a cough may have a lower risk of mortality within 24 hours of admission to hospital.
COVID-19 patients who presented with shortness of breath were found to be 2.5 times more likely to die within 24 hours of admission to the hospital than patients with no shortness of breath. These findings are consistent with recent studies that found shortness of breath to be positively associated with COVID-19 progressions, such as severe illness and death.[19,23] Shortness of breath in COVID-19 patients has a higher risk of mortality within 24 hours of admission. Anosmia, sore throat, dysgeusia, body aches, diarrhoea, chest pain and loss of appetite are some of the most common presenting symptoms of COVID-19.[15,24,25] However, in the present study, it was found that clinical presentations such as anosmia, sore throat, dysgeusia, body aches, diarrhoea, chest pain and/or loss of appetite were not significantly associated with COVID-19 mortality within 24 hours of admission. The discrepancy could be attributed to the fact that these were new symptoms discovered following the pandemic s second wave. Between March and August of 2020, no data were collected on patients regarding these variables.
The most common comorbidities among COVID-19 patients were hypertension (58.3%), diabetes mellitus (29.8%) and heart disease.[15,26-28] Diabetes mellitus and hypertension were reported in previous studies as independently associated with mortality in COVID-19 patients, with chronic kidney disease being the most common comorbidity leading to death.[27-29] These results are comparable with our study results, which show that the odds of COVID-19 patients with hypertension dying within 24 hours of admission to the hospital are -50% higher than the odds of normotensive patients dying within 24 hours of admission to the hospital (OR 1.450; 95% CI 1.012 - 2.078). It was found that common comorbidities such as HIV/AIDS, TB, diabetes mellitus, obesity and cancer are not significantly associated with COVID-19 mortality within 24 hours of admission. This contradicts previous studies that show a statistically significant link between HIV/AIDS, TB, diabetes and obesity and COVID-19 death.[30-33] However, one metaanalysis study found that people living with HIV had a higher risk of COVID-19 mortality than those who did not have HIV infection in the USA and SA, but no significant association was found in the UK.[34] The differences in the findings could be attributed to differences in location, population age, other demographic/ social factors and HIV prevalence, as there were few HIV-infected patients in the present study. This was a retrospective secondary study using clinical records. One limitation is that records/files with missing information were excluded, which might have lost valuable information, and influenced the findings negatively. In addition, the study excluded clinical records of non-laboratory-confirmed COVID-19 cases.
Conclusion
This study used data from all 41 public hospitals in Limpopo Province and found that 411 COVID-19 patients (40%) died within 24 hours of admission. Patients who presented at the hospital with shortness of breath, fever and hypertension were at higher risk of dying within 24 hours. Assessing risk factors for COVID-19 mortality within 24 hours of admission will assist in determining intervention to prevent late presentation, and aid the understanding and prioritising of patients with severe/critical COVID-19 and comorbidities such as hypertension.
Declaration. None.
Acknowledgements. The LDoH COVID-19 response committees and teams at the provincial, district and facility levels. Employees from the World Health Organization and the Cuban medical brigade. Our sincere thanks are due to anonymous reviewers for their excellent comments and suggestions, which improved the presentation.
Author contributions. The study's conceptualisation and data interpretation were done by all the authors. The statistical analysis was carried out by PMM.
Funding. None.
Conflicts of interest. None.
References
1. Wang Y, Ma S, Yang C, et al. Acute psychological effects of coronavirus disease 2019 outbreak among healthcare workers in China. A cross-sectional study. Translationai Psychiatr 2020;10(1):348. https://doi.org/10.1038/s41398-020-01031-w [ Links ]
2. Almansour A, Alagil J, Alamoudi NB, et al. The influence of physical activity on COVID-19 prevention among quarantined individuals. A case-control study. J Muitidisciplin Healthcare 2022;15:271-280. https://doi.org/10.2147/jmdh.s352753 [ Links ]
3. Makgahlela M, Mothiba TM, Mokwena JP, Mphekgwana P. Measures to enhance student learning and well-being during the COVID-19 pandemic. Perspectives of students from a historically disadvantaged university. Edu Sci 2021;11(5):212. https://doi.org/10.3390/educsci11050212 [ Links ]
4. Vaiensisi G. COVID-19 and global poverty. Are LDCs being left behind? Eur J Dev Res 2020;32(5):1535-1557. https://doi.org/10.1057/s41287-020-00314-8 [ Links ]
5. Gilbert M, Puliano G, Pinotti F, et al. Preparedness and vulnerability of African countries against importations of COVID-19. A modelling study. Lancet 2020;395(10227):871-877. https://doi.org/10.1016/s0140-6736(20)30411-6 [ Links ]
6. Chersich MF, Gray G, Fairlie L, et al. COVID-19 in Africa. Care and protection for frontline healthcare workers. Glob Health 2020;16(1):1-6. [ Links ]
7. Bulled N, Singer M. In the shadow of HLV & TB. A commentary on the COVID epidemic in South Africa. Glob Pub Health 2020;15(8):1231-1243. https://doi.org/10.1080/17441692.2020.1775275 [ Links ]
8. Piliay-van Wyk V, Msemburi W, Laubscher R, et al. Mortality trends and differentials in South Africa from 1997 to 2012. Second National Burden of Disease Study. Lancet Glob Health 2016;4(9):e642-e653. https://doi.org/10.1016/S2214-109X(16)30113-9 [ Links ]
9. Whittaker A, Anson M, Harky A. Neurological manifestations of COVID-19. A systematic review and current update. Acta Neurologica Scandinavica 2020;142(1):14-22. https://doi.org/10.1111/ane.13266 [ Links ]
10. Lavery AM, Preston LE, Ko JY, et al. Characteristics of hospitalised COVID-19 patients discharged and experiencing same-hospital readmission - United States, March - August 2020. Morbid Mortal Week Rep 2020;69(45):1695. https://doi.org/10.15585%2Fmmwr.mm6945e2 [ Links ]
11. Guo A, Lu J, Tan H, et al. Risk factors on admission associated with hospital length of stay in patients with COVID-19: A retrospective cohort study. Sci Rep 2021;11(1):1-7. https://doi.org/10.1038%2Fs41598-021-86853-4 [ Links ]
12. Sarker SS, Hasan SA, Islam MS, et al. Length of hospital stay of COVID-19 patients and its relationship with liver function abnormalities. Bangabandhu Sheikh Mujib Med Uni J 2021;7:8-12. https://doi.org/10.3329/bsmmuj.vl4i3.54674 [ Links ]
13. Hu Y, Sun J, Dai Z, et al. Prevalence and severity of corona virus disease 2019 (COVID-19). A systematic review and meta-analysis. J Clin Virol 2020;127:104371. https://doi.org/10.1016%2Fj.jcv.2020.104371 [ Links ]
14. Tshitangano TG, Setati ME, Mphekgwana PM, Ramalivhana NJ, Matlala SF. Epidemiological characteristics of COVID-19 inpatient deaths during the first and second waves in Limpopo Province, South Africa. J Respir 2022;2(2):111-122. https://doi.org/10.3390/jor2020009 [ Links ]
15. Htun YM, Win TT, Aung A, et al. Initial presenting symptoms, comorbidities and severity of COVID-19 patients during the second wave of epidemic in Myanmar. Trop Med Health 2021;49(1):62. https://doi.org/10.1186/s41182-021-00353-9 [ Links ]
16. Tamshidi B, Tamshidi Zargaran S, Bekrizadeh H, Rezaei M, Najafi F. Comparing length of hospital stay during COVID-19 pandemic in the USA, Italy and Germany. Int J Qual Health Care 2021;33(1):mzab050. https://doi.org/10.1093/intqhc/mzab050 [ Links ]
17. Rees EM, Nightingale ES, Tafari Y, et al. COVID-19 length of hospital stay. A systematic review and data synthesis. BMC Med 2020;18(1):1-22. [ Links ]
18. Maslo C, Friedland R, Toubkin M, Laubscher A, Akaioo T, Kama B. Characteristics and outcomes of hospitalised patients in South Africa during the COVID-19 Omicron wave compared with previous waves. JAMA 2022;327(6):583-584. https://doi.org/10.1001/jama.2021.24868 [ Links ]
19. Birhanu A, Merga BT, Ayana GM, Alemu A, Negash B, Dessie Y. Factors associated with prolonged length of hospital stay among COVID-19 cases admitted to the largest treatment center in Eastern Ethiopia. SAGE Open Med 2022;10:20503121211070366. https://doi.org/10.1177/20503121211070366 [ Links ]
20. Bhatt RD, Shrestha C, Risal P. Factors affecting turnaround time in the clinical laboratory of the Kathmandu University Hospital, Nepal. ETIFCC 2019;30(1):14-24. [ Links ]
21. Tharakan S, Nomoto K, Miyashita S, Ishikawa K. Body temperature correlates with mortality in COVID-19 patients. Crit Care 2020;24(1):1-3. https://doi.org/10.1186/s13054-020-03045-8 [ Links ]
22. Vilke GM, Brennan TT, Cronin AO, Castillo EM. Clinical features of patients with COVID-19. Is temperature screening useful? J Emerg Med 2020;59(6):952-956. https://doi.org/10.1016%2Fj.jemermed.2020.09.048 [ Links ]
23. Shi L, Wang Y, Wang Y, Duan G, Yang H. Dyspnea rather than fever is a risk factor for predicting mortality in patients with COVID-19. J Infect 2020;81(4):647-679. https://doi.org/10.1016%2Fj.jinf.2020.05.013 [ Links ]
24. World Health Organization. Clinical management of COVID-19: Interim guidance, 27 May 2020. Geneva. World Health Organization, 2020. [ Links ]
25. Afshar Y, Gaw SL, Flaherman VJ, et al. Clinical presentation of coronavirus disease 2019 (COVID-19) in pregnant and recently pregnant people. Obstet Gynecol 2020;136(6):1117-1125. https://doi.org/10.1097/AOG.0000000000004178 [ Links ]
26. Sanyaolu A, Okorie C, Marinkovic A, et al. Comorbidity and its impact on patients with COVID-19. SN Comp Clin Med 2020;2(8):1069-1076. https://doi.org/10.1007%2Fs42399-020-00363-4 [ Links ]
27. Osibogun A, Baiogun M, Abayomi A, et al. Outcomes of COVID-19 patients with comorbidities in southwest Nigeria. PloS ONE 2021;16(3):e0248281. https://doi.org/10.1371/journal.pone.0248281 [ Links ]
28. Ng WH, Tipih T, Makoah NA, et al. Comorbidities in SARS-CoV-2 patients. A systematic review and meta-analysis. mBio 2021;12(1):e03647-20. https://doi.org/10.1128/mbio.03647-20 [ Links ]
29. Ansari KA, Alwazzeh MJ, Alkuwaiti FA, et al. Early determinants of mortality in hospitalised COVID-19 patients in the Eastern Province of Saudi Arabia.Int J Gen Med 2022;15:1689-1701. https://doi.org/10.2147/IJGM.S349598 [ Links ]
30. Bhaskaran K, Rentsch CT, MacKenna B, et al. HIV infection and COVID-19 death. A population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet HIV 2021;8(1):e24-e32. [ Links ]
31. Mahamat-Saieh Y, Fiolet T, Rebeaud ME, et al. Diabetes, hypertension, body mass index, smoking and COVID-19-related mortality. A systematic review and meta-analysis of observational studies. BMJ Open 2021;11(10):e052777. [ Links ]
32. Gao Y, Liu M, Chen Y, Shi S, Geng J, Tian J. Association between tuberculosis and COVID-19 severity and mortality. A rapid systematic review and meta-analysis. J Med Virol 2021;93(1):194-196. https://doi.org/10.1002/jmv.26311 [ Links ]
33. Chanda D, Minchelia PA, Kampamba D, et al. COVID-19 severity and COVID-19-associated deaths among hospitalised patients with HIV infection - Zambia, March - December 2020. Morbid Mortal Week Rep 2021;70(22):807. https://doi.org/10.15585/mmwr.mm7022a2 [ Links ]
34. Dong Y, Li Z, Ding S, et al. HIV infection and risk of COVID-19 mortality. A meta-analysis. Medicine 2021;100(26):e26573. https://doi.org/10.1097/MD.0000000000026573 [ Links ]
 Correspondence:
Correspondence:
P M Mphekgwana
peter.mphekgwana@ul.ac.za
Accepted 22 March 2023














