Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
SAMJ: South African Medical Journal
On-line version ISSN 2078-5135
Print version ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 n.6 Pretoria Jun. 2023
http://dx.doi.org/10.7196/SAMJ.2023.v113i6.709
IN PRACTICE
CLINICAL UPDATE
Bronchiolitis v. bronchopneumonia: Navigating antibiotic use within the lower respiratory tract infection spectrum
Z DangorI, II, III,*; S G LalaIII,*; C VerweyI, II; G ReubensonVI; D WhiteVII; D P MooreI, II; P JeenaIV; R MasekelaIV; H J ZarV
IMB BCh, PhD; Vaccines and Infectious Diseases Analytics Research Unit, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIMB BCh, PhD; Department of Paediatrics and Child Health, Faculty of Health Sciences, University of the Witwatersrand, South Africa
IIIMB BCh, PhD; Paediatric Education and Research Ladder, Department of Paediatrics, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IVMB BCh, PhD; Department of Paediatrics and Child Health, School of Clinical Medicine, College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
VMB BCh, PhD; Department of Paediatrics and Child Health and MRC Unit on Child and Adolescent Health, Faculty of Health Sciences, University of Cape Town, South Africa
VIMB BCh, DTM&H; Department of Paediatrics and Child Health, Faculty of Health Sciences, University of the Witwatersrand, South Africa
VIIMB BCh, MMed (Paed); Department of Paediatrics and Child Health, Faculty of Health Sciences, University of the Witwatersrand, South Africa
ABSTRACT
Bronchiolitis, a common reason for infant hospitalisation in South Africa (SA), is caused by viral pathogens. Bronchiolitis is typically an illness of mild to moderate severity that occurs in well-nourished children. Hospitalised SA infants frequently have severe disease and/or coexisting medical conditions, and these cases of bronchiolitis may have bacterial co-infection that requires antibiotic therapy. However, the existence of widespread antimicrobial resistance in SA warrants the judicious use of antibiotics. This commentary describes: (i) common clinical pitfalls leading to an incorrect diagnosis of bronchopneumonia; and (ii) considerations for antibiotic therapy in hospitalised infants with bronchiolitis. If antibiotics are prescribed, the indication for their use should be clearly stated, and antibiotic therapy must be stopped promptly if investigations indicate that bacterial co-infection is unlikely. Until more robust data emerge, we recommend a pragmatic management strategy to inform antibiotic use in hospitalised SA infants with bronchiolitis in whom bacterial co-infection is suspected.
Bronchiolitis and bronchopneumonia are the commonest forms of lower respiratory tract infection (LRTI) in children aged <2 years. In the era of improved childhood pneumococcal and Haemophilus influenzae type b conjugate vaccination, both conditions are predominantly caused by viruses. Among hospitalised cases, the commonest cause is respiratory syncytial virus (RSV) (40 - 80% of bronchiolitis and 20 - 40% of bronchopneumonia).[1-5] Other respiratory viral pathogens commonly associated with childhood LRTI include human metapneumovirus, influenza, parainfluenza, adenovirus and human rhinovirus. Although bronchiolitis is predominantly caused by a single viral pathogen, a substantial proportion of children with LRTI will have multiple potential pathogens detectable by molecular testing of respiratory samples,[1-3,5] so determining the causative bacterial and/or viral pathogens in cases of mixed infection remains challenging. Bacterial co-infection is uncommon in bronchiolitis, but it is reported more frequently in children with severe disease, including those requiring invasive ventilation.[6]
The 'umbrella' term LRTI does not differentiate between bronchiolitis and bronchopneumonia, and the World Health Organization (WHO) case definition of pneumonia (with key presenting complaints of 'difficulty breathing or cough') is not specific and would include most cases of bronchiolitis. The WHO pneumonia case definition is intended to be nonspecific to reduce the high pneumonia-related mortality in low- and middle-income countries (LMICs) through oxygen and antibiotic use. However, with the emergence of widespread antimicrobial resistance and increasing recognition of the importance of antimicrobial stewardship, a more targeted approach to use of antibiotics is required. While empirical antibiotics are indicated for children with bronchopneumonia, antibiotics are not recommended for bronchiolitis[4,7,8] A proportion of children with bronchiolitis may, however, have bacterial co-infection(s) that warrant antibiotic therapy.[8,9] In this commentary, we highlight the challenges of identifying children with bacterial co-infection and propose a pragmatic management strategy for clinicians working in South African (SA) healthcare facilities.
Clinical features that differentiate bronchiolitis from bronchopneumonia
In the absence of a gold-standard laboratory, radiological and/ or microbiological test, a careful clinical examination, as well as epidemiological information (for example, the timing of the RSV season), becomes an indispensable requirement to differentiate bronchiolitis from bronchopneumonia.[4,81 Children with bronchiolitis have chest hyperinflation and minute-to-minute variation in clinical findings. The Hoover sign, i.e. subcostal recessions when a flattened diaphragm pulls laterally against the lower chest wall, may also be present (but is not pathognomonic of bronchiolitis). Importantly, chest auscultation usually reveals diffuse crackles with or without wheezing. Bronchiolitis may also present as apnoeic episodes in neonates and young infants.
Common reasons for misdiagnosing bronchiolitis as pneumonia include: (i) failure to detect hyperinflation; (ii) equating the detection of crackles with bronchopneumonia; (iii) failure to detect a prolonged expiratory phase and/or wheezing; and (iv) mistaking normal bronchovesicular breath sounds for bronchial breathing. To minimise these errors, clinicians should familiarise themselves with normal infant breath sounds. It is important to perform auscultation over both axillae and the lower zones posteriorly and laterally, because these auscultatory regions are further from major airways.
There are no absolute clinical features, including the severity of respiratory distress, that indicate bacterial co-infection in a child with bronchiolitis. Although several clinical scoring systems have been developed to assess the severity of bronchiolitis, these need further refinement and validation across multiple settings.[10-12] An example of such a scoring system is the modified Tal score, but this has not been validated in SA[13] (Table 1). Scoring systems can inform appropriate management and decision-making, but do not minimise the need for careful, regular monitoring, especially during the peak of disease severity (usually days 2 - 4 of illness).[8] Scoring systems are also subject to intra- and inter-observer variability.[10] We recommend that the same clinical severity criteria or scoring system be used throughout the child's admission to provide consistency and allow tracking of deterioration or improvement.
Some clinical signs are more subjective (level of retractions/ recessions, breath sound intensity, and presence and loudness of wheezing) than others, and their recognition will depend on the experience of the clinician. When assessing severity, focus on objective parameters first; these include respiratory rate, oxygen saturation, willingness to feed (normal, less than usual or not interested), and general behaviour. The respiratory rate should be evaluated over a full minute to account for the periodic breathing patterns in young infants. Failure of normalisation of oxygen saturation while receiving appropriate oxygen therapy may indicate respiratory failure. The context in which the respiratory assessment takes place is also important; note the child's level of consciousness (calm, asleep, crying or agitated) and whether they are febrile, coughing or feeding during the examination, as these may alter their clinical signs. Where possible, and after parental or caregiver consent has been obtained, video recordings of the breathing patterns should be considered.
Investigations
In general, apart from screening for HIV infection, no additional investigations (e.g. full blood count, serum electrolytes, blood culture) are warranted in a child with typical mild or moderately severe bronchiolitis - this constitutes most children hospitalised with bronchiolitis.[4,8] Measurement of biomarkers for bacterial co-infection may be indicated in children with severe bronchiolitis, those with associated comorbidities (preterm <29 weeks' gestation, chronic lung disease of prematurity, congenital heart disease with increased pulmonary blood flow, immunodeficiency or neuromuscular disorders), those who are not improving as expected after 48 hours of admission, or those presenting with recurrent episodes of bronchiolitis. Until a better diagnostic test becomes available, a C-reactive protein (CRP) level >40 mg/L is a reasonable indication to initiate antibiotic therapy.[14,15] A chest radiograph is indicated in children who may have alternative explanations for wheezing (e.g. endobronchial tuberculosis, congenital anatomical compression of the airway, foreign body), or if complications are suspected during an episode of bronchiolitis.
Treatment
Supportive oxygen therapy is the mainstay of management. In children with moderate or severe bronchiolitis, humidified and/ or high-flow nasal cannula (HFNC) oxygen may reduce the need for invasive ventilation and/or the duration of hospitalisation in resource-constrained settings.[16] Therapies that are not recommended include short-acting beta-agonists (SABAs), nebulised adrenaline, nebulised saline or hypertonic saline, nebulised or systemic corticosteroids, chest physiotherapy, antivirals or montelukast.[4,8] These therapies have not been proven to benefit children with bronchiolitis enrolled in well-designed clinical trials. The presentation of children with bronchiolitis may follow three possible scenarios that impact on treatment, namely: (i) mild or moderate; (ii) severe; or (iii) recurrent presentations (Fig. 1).
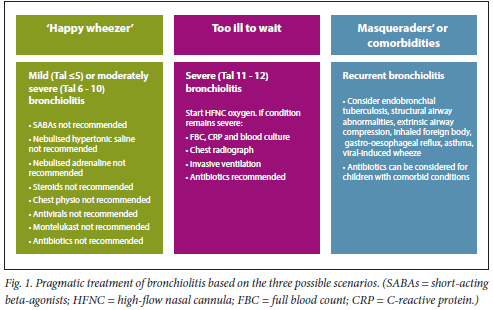
• Mild or moderately severe bronchiolitis. Supportive therapy includes oxygen to treat hypoxia (oxygen saturation <92%, or <90% at altitudes >1 800 m), adequate nutrition and hydration, and nasal suctioning in young infants who are obligate nasal breathers.
• Severe bronchiolitis. In an infant in whom standard oxygen therapy fails, we recommend that HFNC oxygen be initiated, and the child clinically reassessed at least once within the first hour thereafter, and preferably every 15 minutes (if possible). If there is no significant improvement with HFNC oxygen (i.e. a change of severity score from severe to moderate or mild), consider invasive ventilation, undertake investigations, and administer broad-spectrum antibiotics.[7]
• Recurrent bronchiolitis. If the recurrence is severe, treat as above. Recurrent bronchiolitis episodes tend to occur more frequently in children with comorbidities.[4] Alternatively, recurrent episodes may indicate asthma or other underlying conditions such as endobronchial tuberculosis, structural airway abnormalities, extrinsic airway compression, inhaled foreign body, gastro-oesophageal reflux, viral-induced wheeze (which may be a sequela of prior RSV or adenovirus infection) or cystic fibrosis.
Principles guiding potential antibiotic use in children with bronchiolitis
Antibiotics should not be prescribed for bronchiolitis of mild or moderate severity (the vast majority of cases). Until more robust data emerge for children with bronchiolitis who may have bacterial co-infection(s), we recommend the following strategy for prescribing antibiotic therapy. Antibiotics should be prescribed or considered for children with:
• severe disease, particularly those requiring invasive ventilation[6]
• associated comorbidities (uncontrolled HIV infection, severe malnutrition, preterm <29 weeks gestation, chronic lung disease of prematurity, congenital heart disease with increased pulmonary blood flow, primary immunodeficiency or neuromuscular disorders)
• neonates
• CRP >40 mg/L[14,15]
• not following the natural history of disease (prolonged fever and/ or cough).
If antibiotics are prescribed, the specific indication(s) should be documented in the clinical notes. Antibiotic choice should be based on local microbiological data (if available) or guidelines.[7]
Prevention of bronchiolitis
Antibiotic stewardship is likely to be improved when accessible effective preventive therapies for RSV are implemented. There has been considerable progress regarding the prevention of RSV bronchiolitis.[17] In SA, the only available preventive treatment is currently the short-acting monoclonal antibody palivizumab, which remains expensive and requires monthly dosing during the RSV season.[17,18] A newly developed single-dose monoclonal antibody, nirsevimab, has shown excellent safety and efficacy in preventing RSV-associated LRTI hospitalisation in preterm and full-term infants, as well as a reduction in subsequent antibiotic prescribing and LRTI episodes.[19,20] Vaccination of pregnant women, with the aim of protecting their infants in the first few months of life, is another promising strategy that has also been associated with a reduction in subsequent antibiotic use.[17,21] In clinical trials, maternal RSV vaccines are effective against RSV-LRTI, hospitalisation for RSV-LRTI and all-cause severe LRTI in infants of vaccinated mothers.[21,22] Until these preventive strategies are licensed and accessible to LMICs, the burden of RSV-LRTI will remain high.[17]
Conclusion
In children with bronchiolitis of mild or moderate severity, the best available evidence does not support any routine treatment (SABAs, nebulised adrenaline, nebulised saline or hypertonic saline, corticosteroids, chest physiotherapy, antivirals, montelukast or antibiotics), and management should be directed towards careful monitoring for worsening of clinical signs and providing supportive therapy (oxygen to reverse hypoxia, adequate nutrition and hydration). Children with severe bronchiolitis, neonates, and those with severe malnutrition, uncontrolled HIV infection, atypical or recurrent presentations and other comorbid conditions warrant additional investigations and may require empirical antibiotic therapy for bacterial co-infection. Future research on using biomarkers to guide antibiotic therapy and assessing the validity of severity scores in low- and middle-income settings is required.
Declaration. None.
Acknowledgements. None.
Author contributions. ZD wrote the first draft. All authors provided critical input and approved the final version.
Funding. HJZ is supported by the South African Medical Research Council. DPM is in part supported through a grant awarded by the Carnegie Corporation of New York. Other authors have no funding to disclose.
Conflicts of interest. None.
References
1. Jain S, Williams DJ, Arnold SR, et al. Community-acquired pneumonia requiring hospitalisation among U.S. children. N Engl J Med 2015;372(9):835-845. https://doi.org/10.1056/NEJMc1511751 [ Links ]
2. Zar HJ, Barnett W, Stadler A, Gardner-Lubbe S, Myer L, Nicol MP. Aetiology of childhood pneumonia in a well vaccinated South African birth cohort: A nested case-control study of the Drakenstein Child Health Study. Lancet Respir Med 2016;4(6):463-472. https://doi.org/10.1016/S2213-2600(16)00096-5 [ Links ]
3. Pneumonia Etiology Research for Child Health (PERCH) Study Group. Causes of severe pneumonia requiring hospital admission in children without HIV infection from Africa and Asia: The PERCH multi-country case-control study. Lancet 2019;394(10200):757-779. https://doi.org/10.1016/S0140-6736(19)30721-4 [ Links ]
4. Meissner HC. Viral bronchiolitis in children. N Engl J Med 2016;374(18):1793-1794. https://doi.org/10.1056/NEJMc1601509 [ Links ]
5. Von Mollendorf C, Berger D, Gwee A, et al. Aetiology of childhood pneumonia in low- and middle-income countries in the era of vaccination: A systematic review. J Glob Health 2022;12:10009. https://doi.org/10.7189/jogh.12.10009 [ Links ]
6. Guitart C, Alejandre C, Bobillo-Perez S, et al. Risk factors and incidence of invasive bacterial infection in severe bronchiolitis: The RICOIB prospective study. BMC Pediatr 2022;22(1):140. https://doi.org/10.1186/s12887-022-03206-4 [ Links ]
7. Zar HJ, Moore DP, Andronikou A, et al. Diagnosis and management of community-acquired pneumonia in children: South African Thoracic Society guidelines. Afr J Thorac Crit Care Med 2020;26(3):98-116. https://doi.org/10.7196/AJTCCM.2020.v26i3.104 [ Links ]
8. Florin TA, Plint AC, Zorc JJ. Viral bronchiolitis. Lancet 2017;389(10065):211-224. https://doi.org/10.1016/S0140-6736(16)30951-5 [ Links ]
9. Ralston SL, Lieberthal AS, Meissner HC, et al. Clinical practice guideline: The diagnosis, management, and prevention of bronchiolitis. Pediatrics 2014;134(5):e1474-e1502. https://doi.org/10.1542/peds.2014-2742 (Erratum in: Pediatrics 2015;136(4):782. https://doi.org/10.1542/peds.2015-2862) [ Links ]
10. Rodriguez-Martinez CE, Sossa-Briceno MP, Nino G. Systematic review of instruments aimed at evaluating the severity of bronchiolitis. Paediatr Respir Rev 2018;25:43-57. https://doi.org/10.1016/j.prrv.2016.12.006 [ Links ]
11. Hakizimana B, Saint G, van Miert C, Cartledge P. Can a respiratory severity score accurately assess respiratory distress in children with bronchiolitis in a resource-limited setting? J Trop Pediatr 2020;66(2):234-243. https://doi.org/10.1093/tropej/fmz055 [ Links ]
12. Bedson W, Wilkinson E, Hawcutt D, Mcnamara P. Severity scores used in the assessment of bronchiolitis: A systematic review. Eur Respir J 2021;58(Suppl 65):OA2846. [ Links ]
13. Golan-Tripto I, Goldbart A, Akel K, Dizitzer Y, Novack V Tal A. Modified Tal score: Validated score for prediction of bronchiolitis severity. Pediatr Pulmonol 2018;53(6):796-801. https://doi.org/10.1002/ppul.24007 [ Links ]
14. Higdon MM, Le T, O'Brien KL, et al. Association of C-reactive protein with bacterial and respiratory syncytial virus-associated pneumonia among children aged <5 years in the PERCH study. Clin Infect Dis 2017;64(Suppl_3):S378-S386. https://doi.org/10.1093/cid/cix150 [ Links ]
15. Isa HM, Mohroofi AD, Alkhan FN, et al. C-reactive protein levels in children with acute bronchiolitis. Int J Pediatr 2022;2022:1311936. https://doi.org/10.1155/2022/1311936 [ Links ]
16. Kugelman A. High-flow nasal cannula therapy: Can it be recommended as initial or rescue care for infants with moderate bronchiolitis in the paediatric ward? Eur Respir J 2020;56(1):2001020. https://doi.org/10.1183/13993003.01020-2020 [ Links ]
17. Mazur NI, Terstappen J, Baral R, et al. Respiratory syncytial virus prevention within reach: The vaccine and monoclonal antibody landscape. Lancet Infect Dis 2023;23(1):e2-e21. https://doi.org/10.1016/S1473-3099(22)00291-2 [ Links ]
18. Shahabi A, Peneva D, Incerti D, McLaurin K, Stevens W. Assessing variation in the cost of palivizumab for respiratory syncytial virus prevention in preterm infants. Pharmacoecon Open 2018;2(1):53-61. https://doi.org/10.1007/s41669-017-0042-3 [ Links ]
19. Griffin MP, Yuan Y, Takas T, et al. Single-dose nirsevimab for prevention of RSV in preterm infants. N Engl J Med 2020;383(5):415-425. https://doi.org/10.1056/NEJMoa1913556 [ Links ]
20. Hammitt LL, Dagan R, Yuan Y, et al. Nirsevimab for prevention of RSV in healthy late-preterm and term infants. N Engl J Med 2022;386(9):837-846. https://doi.org/10.1056/NEJMoa2110275 [ Links ]
21. Madhi SA, Polack FP, Piedra PA, et al. Respiratory syncytial virus vaccination during pregnancy and effects in infants. N Engl J Med 2020;383(5):426-439. https://doi.org/10.1056/NEJMoa1908380 [ Links ]
22. Simoes EAF, Center KJ, Tita ATN, et al. Prefusion F protein-based respiratory syncytial virus immunisation in pregnancy. N Engl J Med 2022;386(17):1615-1626. https://doi.org/10.1056/NEJMoa2106062 [ Links ]
 Correspondence:
Correspondence:
Z Dangor
ziyaad.dangor@wits.ac.za
Accepted 2 March 2023
* Joint first authors














