Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
SAMJ: South African Medical Journal
versión On-line ISSN 2078-5135
versión impresa ISSN 0256-9574
SAMJ, S. Afr. med. j. vol.113 no.6 Pretoria jun. 2023
http://dx.doi.org/10.7196/SAMJ.2023.v113i6.1037
CME
Approach to the diagnosis and management of snakebite envenomation in South Africa in humans: The hospital phase - emergency unit general principles
T C HardcastleI, II, III; A EngelbrechtIV, V; V LallooVI, VII; C BellVIII, IX; M ToubkinX, XI
IMMed (Chir), PhD; Trauma and Burns Service, Inkosi Albert Luthuli Central Hospital, and KwaZulu-Natal Department of Health, Durban, South Africa
IIMMed (Chir), PhD; Department of Surgical Sciences, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IIIMMed (Chir), PhD; National Snakebite Advisory Group, Durban, South Africa
IVMMed (Farn Med), FCEM (SA); National Snakebite Advisory Group, Durban, South Africa
VMMed (Farn Med), FCEM (SA); Department of Emergency Medicine, Faculty of Health Sciences, University of Pretoria, South Africa
VIMMed (EM), FC EM (SA); National Snakebite Advisory Group, Durban, South Africa
VIIMMed (EM), FC EM (SA); Department of Emergency Medicine, Faculty of Health Sciences, University of Pretoria, South Africa
VIIIMB ChB; National Snakebite Advisory Group, Durban, South Africa
IXMB ChB; Mosvold Hospital, KwaZulu-Natal Department of Health, and Department of Family Medicine, University of KwaZulu-Natal, Durban, South Africa
XRN (Trauma/Crit Care), MSc (EM); National Snakebite Advisory Group, Durban, South Africa
XIRN (Trauma/Crit Care), MSc (EM); Netcare Emergency, Trauma and Transplant, NetcareHead Office, Johannesburg, South Africa
ABSTRACT
Snakebite management is largely driven by expert opinion and consensus. However, there are a few large retrospective studies and randomised controlled trials that have improved the quality of medical guidance currently available. South African snakes are different in venomous potential to snakes in other parts of the world, and it behoves the hospital provider and the average medical practitioner to know the current best practice concepts concerning assessment, treatment and antivenom use. The recent South African Snakebite Symposium meeting in July 2022 provided an update and national consensus from which this Hospital Care document is derived.
Treatment strategies that apply to snake envenomation from the Americas, Middle East, Asia and Australasia are inappropriate for Africa, owing to species and venom-action variance, or the significant antivenom differences. The content of this article is part of a CME series resulting from the multidisciplinary 2-day South African Snakebite Symposium meeting and the many pre-meeting online round-robin sessions.
Admittedly, the content is largely expert opinion based on retrospective data, with little or no randomised or prospective studies available (except for those on adrenaline pre-dosing) on the treatment of snake envenomation in South Africa (SA).[1,2] The document aims to provide the current best evidence and best practice information for the hospital care phase from the general perspective. The essential aspects are also available in the form of a flipchart addressing in-hospital treatment.
Since the emergency unit is usually the first point of contact for snakebite victims, all emergency unit staff should be familiar with the principles of snakebite management. Antivenom should be available in any hospital where snakebite victims are likely to present and be managed.[3,4]
General management on presentation to the emergency unit is provided in the hospital provider flipchart and a protocol document.[5,6]
A detailed handover should be received from the emergency medical service (EMS) or persons accompanying the patient. If the snake is known, or if a photo is provided, this can aid further management. However, if the snake is unknown (often the case with legitimate bites), the syndromic approach to management is advocated.[7]
Essential aspects of the history and physical examination include:
• How did the bite occur? (gives an indication to dry bite/scratch v. an angry snake with a proper bite)
• Where on the body was the patient bitten?
• How long has it been since the snakebite?
• Is there an identification/description of the snake?
• What activity was performed at the time of the bite and what treatment was given?
• Has the patient sustained a snakebite before, or received an antivenom previously? (the more antivenom received previously, the greater the chances of allergic reactions)
• When doing the clinical examination: fang marks - absence of fang marks does not rule out snakebite; a double row of teeth marks without distinct fang marks may suggest less venomous species, while two distinct fang marks suggest a venomous snake. A single row of teeth marks on the opposite side of fang marks are sometimes seen and caused by the teeth in the lower jaw of a venomous snake.
Signs and symptoms
Look for signs of progressive weakness: Ps: paralysis, ptosis, paraesthesia, pupillary dilatation and Ss: sweating, salivation, slurred speech, swallowing difficulties. Other features include ataxia and the 'broken neck syndrome' (decreased tone in the muscles of the neck causing 'slumping forward' of the neck.
Painful progressive swelling: swelling, blisters, skin discoloration, frank necrosis of skin.
Bleeding: may be delayed or initially from mucosa only There should be an active search for signs of respiratory distress or shock.
General measures on patient arrival include:
(i) Place the patient on cardiac and vital signs monitors.
(ii) Administer supplemental oxygen via nasal prongs and/or face mask should the oxygen saturation level be <94% on room air. Bag-valve-mask ventilation may be needed for patients with severe neurotoxic envenomation.
(iii) Obtain good intravenous (IV) access.
(iv) Prepare resuscitation equipment for airway, ventilation, shock and anaphylaxis.
(v) Simple analgesia should be provided (IV/oral paracetamol). Opiates can complicate and exacerbate a neurotoxic picture and non-steroidal agents worsen bleeding risk/renal failure with cytotoxic or mixed-syndrome bites.
(vi) Tetanus toxoid 0.5 mL intramuscular injection (IMI) is indicated
(vii) Do not elevate limbs excessively - it increases the spread of venom. Limbs should be kept at the level of the heart.
(viii) No antibiotics initially, but may be required later if tissue necrosis occurs (after 72 hours).
(ix) No steroids or antihistamines recommended as prophylaxis, although they may be used to treat an anaphylactic reaction to the antivenom (as adjuncts to adrenaline).
(x) Appropriate laboratory blood tests include: full blood count, urea, creatinine and electrolytes, clotting screen (or thromboelastography/rotational thromboelastometry (TEG/ ROTEM)) and calcium, magnesium, phosphate. In cases with suspected haemotoxic envenomation the 20-minute whole blood clotting test is useful as a bedside test. In cytotoxic bites, creatinine kinase is recommended.[8]
(xi) For those with neurotoxic envenomation and progressive paralysis early intubation and mechanical ventilation is recommended along with antivenom administration -despite antivenom duration of ventilation can be up to 7 days. An algorithm for intubation and ventilation is provided in Fig. 1.
When a snakebite victim presents to the emergency unit in a stable condition and does not have indications for antivenom administration, a minimum of a 12-hour period of observation is recommended. A pitfall in snakebite management is not recognising clinical decline timeously, leading to missed opportunities for intubation, ventilation and antivenom administration.
Observation is an important part of snakebite management. It should preferably be done in a high care or intensive care unit (ICU) setting where monitoring is more intensive than a regular ward. Recommended monitoring includes:
• continuous end-tidal C02 or pulse oximetry
• half-hourly respiratory rate, heart rate, blood pressure and level of consciousness
• half-hourly peak flow measurements if neurotoxic bite a possibility
• hourly urine output
• hourly longitudinal and circumferential measurements of a swollen limb.
Loss of life or limb from snakebite is preventable by meticulous observations.
The management of a patient with a snakebite from an undefined snake is best accomplished using the syndromic approach. The various syndromes are detailed below, along with the common dangerous species that lead to the syndromes (see also Fig. 2).
Painful progressive swelling syndrome
• Swelling due to predominantly cytotoxic venom, starting at the bite site and progressing up the limb.
• Immense pain with the affected area being warm and tense.
• Symptoms include: blistering, discoloration, subcutaneous haemorrhage, necrosis.
• Complications include: pseudocompartment syndrome, nerve and vessel entrapment, deep vein thrombosis, hypotension, and hypovolaemic shock. True compartment syndrome is rare. Ultrasound is an option to differentiate true from pseudocompartment syndrome.[9]
• 'Skip lesions' are reported in Mozambique spitting cobra bites: these are areas of necrosis with sparing of certain regions in between. Debate exists to whether these are caused by irregular lymphatic spread or simply multiple bites.
• Species responsible: puff adder, Gaboon adder, some of the dwarf adder species, spitting cobras (Mozambique spitting cobra and black spitting cobra), stiletto snakes, and night adders.
Progressive weakness syndrome
• Progressive weakness and paralysis are due to neurotoxic venoms.
• This syndrome can lead to complete paralysis, respiratory failure and cardiac arrest.
• Symptoms include: muscle spasms, drooling, incontinence, salivation, lacrimation, diaphoresis, dilated pupils, fasciculations, dyspnoea, respiratory failure and death.
Species responsible: black mamba, green mamba, non-spitting cobras (Cape cobra, snouted cobra and forest cobra), berg adder and desert mountain adder.
Bleeding syndrome
• History may include need for the snake to be 'pulled off the bite site with some difficulty owing to the back-fanged nature of these snakes.
• Bleeding tendencies are caused by haemotoxic venom leading to a venom-induced consumption coagulopathy (VICC) that develops over time.
• Early symptoms are usually absent. This is followed by bleeding at the bite-site, bruising and a prolonged 20-minute whole blood clotting time - the whole blood clotting time may be abnormal as early as half- to 1 -hour post bite.
• This syndrome eventually leads to widespread internal bleeding.
• Symptoms (although delayed) include: bleeding at the bite site, bleeding from drip sites, bleeding from mucous membranes and epistaxis.
• Later complications include: haematuria, haemoptysis, melena, cerebral haemorrhage, hypotension and hypovolaemic shock (12 -36 hours).
Species responsible: boomslang and vine snakes
Mixed painful progressive swelling and bleeding syndrome
• Mix of complications from the painful progressive swelling as well as bleeding syndromes
Species responsible: puff adder, Gaboon adder.
Mixed painful progressive swelling and progressive weakness syndrome
• Mix of complications from the painful progressive swelling as well as progressive weakness syndromes, although the weakness is usually less severe.
Species responsible: rinkhals, snouted cobra, berg adder and forest cobra
Indications for antivenom[6]
A balance should be struck between snake identification and the syndromic approach. If the snake is positively identified as one of the 10 snakes covered by polyvalent antivenom, or a boomslang is suspected, then antivenom should strongly be considered. If the snake is not positively identified, then the following serves as indications for antivenom using the syndromic approach (Fig. 3).
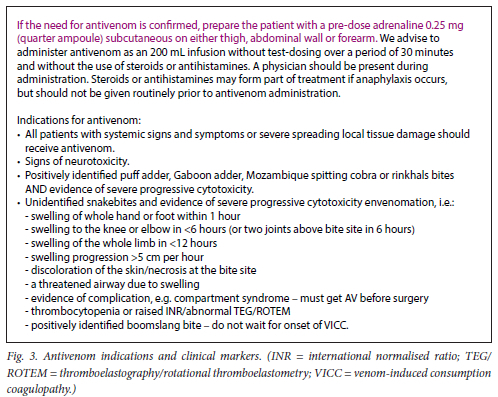
All patients with systemic signs and symptoms or severe spreading local tissue damage should receive antivenom (Fig. 3):
• any signs of neurotoxicity (Ps and Ss)
• positively identified puff adder, Gaboon adder, Mozambique spitting cobra or rinkhals bites AND evidence of severe progressive cytotoxicity.
Unidentified snakebites and evidence of severe progressive cytotoxicity envenomation, i.e.:
• swelling of whole hand or foot within 1 hour
• swelling to the knee or elbow in <6 hours (or two joints above bite site in 6 hours)
• swelling of the whole limb in <12 hours
• swelling progression >7 - 15 cm per hour
• discoloration of the skin/necrosis at the bite site
• a threatened airway due to swelling
• evidence of complications, e.g. pseudo or actual compartment
syndrome - must get antivenom before surgery
• thrombocytopenia, or raised international normalised ratio (INR)/ abnormal TEG/ ROTEM, or drop in haemoglobin[8,10,11]
• positively identified boomslang bite - do not wait for onset of VICG
The South African Vaccine Producers (SAVP) have produced two types of antivenom using equine serum: polyvalent antivenom (PAV) and monovalent antivenom (MAV). The polyvalent antivenom covers 10 snakes and can be easily remembered by the adage '1,2,3,4':[6,12]
1. Rinkhals
2. Adders: puff adder and Gaboon adder
3. Mambas: black mamba; green mamba; Jameson's mamba
4. Cobras: Cape cobra; snouted cobra; Mozambique spitting cobra; forest cobra
A separate MAV is available and is specific for boomslang bites.[6,10,12,13]
Antivenom administration
The practice of testing for equine protein sensitivity is no longer considered useful. Such testing is unreliable and unnecessarily delays antivenom therapy.
Preparation
(i) Monitors should be placed and resuscitation equipment should be ready.
(ii) All drugs should be ready for the treatment of anaphylaxis and 0.5 mL of a 1:1 000 solution of adrenalin (0.3 mL of 1:1 000 solution in children) should be drawn up to be available for immediate intramuscular administration in case of severe anaphylaxis.
Premedication with 0.25 mg adrenaline subcutaneously (or IMI) for the prevention of anaphylaxis is the only evidence-based prophylaxis against reactions available,[6,14,15] although a recent local article suggests it may be less effective on local snakes.[16] Steroids and antihistamines have no prophylactic role.[6,8,15,16]
Corticosteroids have been shown to be ineffective and possibly harmful in the prevention of anaphylaxis in snakebite treatment. They also diminish the effect of subcutaneous adrenaline. Similarly antihistamines are ineffective in the prevention of anaphylaxis from equine antivenom administration, and may complicate the clinical picture (ptosis v. sedation from antihistamine) in neurotoxic snakebites.[6,8,15,16]
Patients with previous antivenom exposure, and atopic individuals, such as those with asthma and eczema, are at higher risk for the development of acute venom-induced anaphylaxis, and should be closely monitored.[8] Finally, avoid adrenaline premedication in patients with a history of ischaemic heart disease, previous stroke, hypertension and tachyarrhythmias.[10]
Administration
The dose of antivenom varies for the different snakes. A safe approach, when unsure, is to administer 10 vials of PAV or one vial of MAV. It may be repeated in increments of two vials PAV (20 mL) or one vial MAV (10 mL) over 10 minutes every subsequent 2 hours, as necessitated by the presence of continued signs and symptoms of envenomation. This may be necessary in the case of multiple bites or bites from large snakes.
(i) The suggested initial dose for patients presenting with a painful progressive swelling syndrome is 6 - 8 vials.
(ii) The suggested initial dose for patients presenting with a progressive weakness syndrome is 8 - 12 vials.
(iii) In the rare event that the identified snake is a Gaboon adder, 20 vials of PAV is recommended.
(iv) For patients presenting with a bleeding syndrome, 1 vial of MAV is recommended as the starting dose.
Technical aspects of administration
Dilute the contents of 10 vials of PAV in normal saline to a total volume of 200 mL. Administer the antivenom intravenously over 30 - 60 minutes at a rate of 200 -400 mL/hour (i.e. 200 mL in 30 minutes).
MAV can be administered as push-dose direct injection in a large-bore IV line or administered as an infusion diluted in 50 mL saline over 15 minutes (Fig. 2).
Tourniquet removal
In some cases, patients present with a tourniquet in place (commercial or improvised). If the bite is considered a 'progressive weakness' or predominantly neurotoxic bite, the following should be done: after 10 minutes of antivenom administration, the tourniquet/splint/ bandages may be removed. This should be done very slowly to prevent a sudden venom rush into the body. Venom and metabolic toxin rush with potentially fatal respiratory failure may be averted by gradual, cautious removal of field-applied tourniquets with concomitant antivenom administration.[17]
In the case of a tourniquet, apply a blood pressure cuff proximally. Inflate to 10 mmHg above the level of the patient's systolic blood pressure. Remove the tourniquet. Slowly release the blood pressure cuff by 5 mmHg every 2 minutes. If the patient's condition worsens, re-inflate the blood pressure cuff and wait for a further 10 minutes before continuing with the procedure. Be aware of the risk for compartment syndrome and reperfusion injury to the kidneys in this context.[17]
Management of anaphylaxis
Should any signs of anaphylaxis develop, e.g. bronchospasnx dyspnoea, hypotension and/or urticaria, immediately discontinue the antivenom. Treat anaphylaxis as per the national resuscitation council guidelines with adrenaline (0.5 mg 1:1 000 IMI), volume resuscitation and salbutamol/ipratropium bromide nebulisations, corticosteroids (200 mg IV injection) or IMI), promethazine (25 mg IMI/IVI) or ranitidine (50 mg IMI/IVI). As soon as the patient is stabilised, continue the antivenom infusion at a slower rate (i.e. 100 - 200 mL/hour). This is usually possible after 20 - 60 minutes of treatment. Should the anaphylaxis reappear, antivenom should be permanently discontinued.
Serum sickness can occur 1-4 weeks post antivenom with a nephritis-like syndrome that responds well to oral steroids in most cases.'3
Additional therapies
For non-spitting cobras
Neostigmine: in the case of a mild presentation of progressive weakness, where antivenom is contraindicated or not available, or where the response to an adequate dose of antivenom is not achieved consider the administration 0.6 mg of glycopyrrolate IV, followed by 2.5 mg of neostigmine IV every 30 minutes up to a maximum of 10 mg neostigmine (four doses) over 24 hours.[10]
Berg adder bites
Patients usually present with anosmia and a neurotoxic progressive weakness syndrome. PAV should not be administered for confirmed berg adder bites, since berg adder venom is not neutralised by the current antivenom. Such patients should receive supportive care in a high care/ICU setting. Monitor for hyponatraemia, which may present as seizures. This should be treated with hypertonic saline (5 mL/kg of 3% hypertonic saline or 100 mL of sodium bicarbonate solution) over 15 minutes.[6,8,10]
Gaboon adder bites
These are known to have a mixed toxicity, including cytotoxic, cardiotoxic, neurotoxic and haemotoxic effects. Cardiotoxic effects include electrocardiogram (ECG) changes such as prolonged QT intervals, inverted T waves, and supraventricular tachycardias that may persist for days after the initial envenomation. Supportive treatment is indicated. Severe bradyarrythmias may require the use of a temporary pacemaker to ensure adequate cardiac output and to prevent cardiac arrest. Gaboon adder venom has a thrombin-like enzyme that quickly depletes serum fibrin levels, thus rendering the blood uncoagulable. In addition, the venom has haemorrhagic activity as it causes widespread damage to the microvasculature. Of note, the lungs and gastrointestinal tract are extremely sensitive to this.
Puff adder bites
Puff adder venom causes painful progressive swelling. In severe envenomation, it may have significant haematological effects. This may necessitate the administration of blood products, including whole blood, packed red cells, platelets, cryoprecipitate, and fresh frozen plasma. Monitoring with TEG/ROTEM or INR is advised in these bites.
Boomslang and vine snake bites
A TEG maybe done when antivenom is ineffective for boomslang bites or for bleeding syndromes from snakes not covered by the SA MAV. TEG is also useful to identify coagulopathy in a suspected boomslang bite before the patient becomes symptomatic, to aid in the decision to give antivenom. It may also assist in evaluating the effectiveness of antivenom, and guide adding further doses.[18] It will guide the use of plasma products, cryoprecipitate and platelet concentrations. Heparin and antifibrinolytic agents (such as tranexamic acid) should not be given.
Snake identification
Snake identification should be carried out by an expert herpetologist. Snake-identification charts provided by herpetologists are useful and should be available in all emergency centres to enable patients to try to indicate the snake type soon after arrival, if conscious.[19] However, snake identification by patients has been studied in SA, and is notoriously unreliable.[20] In SA, these identification charts are freely available from the African Snakebite Institute (https://www.africansnakebiteinstitute.com/) and African Reptiles and Venom (https://africanreptiles-venom.co.za/), among others. Locally relevant posters are recommended.
Differential diagnosis
The differential diagnosis is broad, and includes other neurotoxic bites and stings (spider and scorpion), intoxications, herbal medication toxicity and poisoning from other sources. Guillain-Barré syndrome, tetanus or even botulism may mimic neurotoxic bites.[21] Cellulitis and necrotising fasciitis may mimic cytotoxic bites or complicate them. Cytotoxic spider bites may be confused with the minor cytotoxic adders.[22]
Conclusion
Most deaths related to snakebites and the associated serious sequelae are largely preventable, provided that there is rapid treatment (safe and effective antivenom and supportive care) available locally, and that the healthcare providers are suitably trained in the management of snakebite envenoming, which is the purpose of this article.
Declaration. None.
Acknowledgements. The authors acknowledge the participation of the SASS consensus group in the discussion around snakebite and the contribution of Gift of the Givers to conference support
Author contributions. All authors contributed equally in the preparation of the document and the corresponding author managed submission and queries.
Funding. None.
Conflicts of interest. None.
References
1. World Health Organization Africa Office, Sambo LG. Foreword. In. Guidelines for the Prevention and Clinical Management of Snakebite in Africa. Brazzaville. WHO, 2010 [ Links ]
2. Wilhams DJ, Faiz MA, Abela-Ridder B, et al. Strategy for a globally coordinated response to a priority neglected tropical disease. Snakebite envenoming. PLoS Negl Trop Dis 2019;13(2):e0007059. https://doi.org/10.1371/journalpntd.0007059 [ Links ]
3. Le Geyt J, Pach S, Gutierrez JM, al. Paediatric snakebite envenoming. Recognition and management of cases. Arch Dis Child 2021;106(1):14-19. https://doi.org/10.1136/archdischild-2020-319428 [ Links ]
4. National Department of Health, South Africa. Chapter 19. In. National Department of Health, South Africa. Essential Drugs Programme. Hospital level (Adults) Standard Treatment Guidelines and Essential Medicines List. 5th ed. Pretoria. NDoH, 2019. [ Links ]
5. South African Snakebite Symposium. Hospital Care Provider flipper. Nelspruit. SASS, 2022 [ Links ]
6. South African Snakebite Symposium. Snakebite management. South African consensus guidelines 2022. Nelspruit. SASS, 2022. [ Links ]
7. Curry SC, Horning D, Brady P, Requa R, Kunkel DB, Vance MV. The legitimacy of rattlesnake bites in central Arizona. Ann Emerg Med 1989;18(6):658-663. https://doi.org/10.1016/s0196-0644(89)80523-2 [ Links ]
8. Pattinson JP, Oosthuizen G, Tilbury CR, Wood D. Approaches to snake envenomation in Southern Africa. In. Mackessy SP, ed.. Handbook of Venoms and Toxins of Reptiles. 2nd ed. London. CRC Press, 2021. [ Links ]
9. Wood D, Sartorius B, Hift R Ultrasound findings in 42 patients with cytotoxic tissue damage following bites by South African snakes. Emerg Med J 2016;33(7):477-481. https://doi.org/10.1136/emermed-2015-205279 [ Links ]
10. Müller GJ, Modler H, Wium CA, Veale DJH, Marks CJ. Snake bite in southern Africa. Diagnosis and management. CME 2012;30(10):362-382. [ Links ]
11. Wood D, Sartorius B, Hift R. Classifying snakebite in South Africa. Validating a scoring system. S Afr Med J 2017;107(1):46-51. https://doi.org/10.7196/SAMJ.2017.v107i1.11361 [ Links ]
12. Schrire L, Muller GJ, Pantanowitz L. The diagnosis and treatment of envenomation in South Africa. Rietfontein. South African Vaccine Producers, 1996. [ Links ]
13. Blaylock RS. The identification and syndromic management of snakebite in South Africa. S Afr Fam Pract 2005;47(9):48-53. [ Links ]
14. Premawardhena AP, de Silva CE, Fonseka MM, Gunatilake SB, de Silva HJ. Low dose subcutaneous adrenaline to prevent acute adverse reactions to antivenom serum in people bitten by snakes. Randomised, placebo controlled trial. Br Med J 1999;318(7190):1041-1043. https://doi.org/10.1136/bmj.318.7190.1041 [ Links ]
15. De Silva HA, Pathmeswaran A, Ranasinha CD, et al. Low-dose adrenaline, promethazine, and hydrocortisone in the prevention of acute adverse reactions to antivenom following snakebite. A randomised, double-blind, place bo-controlled trial. PLoS Med 2011;8(5):e1000435. https://doi.org/10.1371/journal.pmed.1000435 [ Links ]
16. Giles T, Cacaia SR, Wood D, Klopper J, Oosthuizen G. A retrospective study of antivenom-associated adverse reaction and anaphylaxis at Ngwelezana Hospital, South Africa. Toxicon 2022;217:1-4. https://doi.org/10.1016/j.toxicon.2022.07.008 [ Links ]
17. Pelle RR Engelbrecht A, Lalloo V. Case Report. Safe tourniquet removal in black mamba (Dendroaspis polylepis) bites. Am J Trop Med Hyg 2021;106(1):338-341. https://doi.org/10.4269/ajtmh.21-0374 [ Links ]
18. Tambwe MJ, Lalioo V, Engelbrecht A, Pelle P. A case report of detecting subclinical coagulopathy in a patient with boomslang (Dipholidus typus) bite. S Afr Fam Pract 2021;63(1):a5299. https://doi.org/10.4102/safp.v63i1.529990 [ Links ]
19. Durso AM, Bolon I, Klein hesselink AR, et al; Crowdsourcing snake identification with online communities of professional herpetologists and avocational snake enthusiasts. R Soc Open Sci 2021;8(1):201273. https://doi.org/10.1098/rsos.201273 [ Links ]
20. Blaylock RS. Epidemiology of snakebite in Eshowe, KwaZulu-Natal, South Africa. Toxicon 2004;43:159166. [ Links ]
21. Müller GJ, Modler H, Wium CJ, Veale DJH. Scorpion sting in southern Africa. Diagnosis and management. CME 2012;30(10):356-361. [ Links ]
22. Müller GJ, Wium CJ, Marks CJ, du Plessis CE, Veale DJH. Spider bite in southern Africa. Diagnosis an management. CME 2012;30(10):382-392. [ Links ]
 Correspondence:
Correspondence:
T C Hardcastle
hardcastle@ukzn.ac.za
Accepted 2 May 2023














